Abstract
Contrast-enhanced multi-detector row spiral computed tomography (MDCT) was introduced as a promising noninvasive method for vascular imaging. This study examined the accuracy of this technique for detecting significant coronary artery stenoses. Both MDCT(Sensation 16, Siemens, Germany, 12 × 0.75 mm collimation and 0.42 sec rotation speed, 120 kV, 500 effective mA, and 2.7 mm/rotation table-feed) and invasive coronary angiography (CAG) were performed on 61 patients (mean age 59.2 ± 10, 44 men) who were suspected of having coronary artery disease. All patients were treated with atenolol (25 - 50 mg) prior to imaging and the heart rate was maintained below 65 beats per minutes during image acquisition. The images were reconstructed in the diastole around TI - 400 ms with a 0.5 mm increment and a 1.0 mm thickness. All coronary arteries with a diameter of 2.0 mm or more were assessed for the presence of a stenosis (> 50% luminal narrowing). Two independent radiologists who were unaware of the results of the invasive CAG evaluated the MDCT data, and the results were compared with those from the invasive CAG (interval 1- 27, mean 11 days). An evaluation of the CT coronary angiogram (CTCA) was possible in 58 of the 61 patients (95%). Image acquisition of the major coronary arteries including the left main trunk was available in 229 out of 244 arteries. Invasive CAG showed that 35 out of 58 patients had significant coronary artery stenoses by. patient analysis of those who could be evaluated showed that CT coronary angiography correctly classified 30 out of 35 patients as having at least 1 coronary stenosis (sensitivity 85.7%, specificity 91.3%, positive predictive value 93.8%, negative predictive value 80.8%). By analyzing each coronary artery, CAG found 62 stenotic coronary arteries in the 229 coronary arteries that could be evaluated. MDCT correctly detected 50 out of 62 stenotic coronary arteries and an absence of stenosis was correctly identified in 156 out of 167 normal coronary arteries (sensitivity 80.6%, specificity 93.4%, positive predictive value 81.9%, negative predictive value 92.8%). The non-invasive technique of MDCT for examining the coronary artery appears to be a useful method for detecting coronary artery stenoses with a high accuracy particularly with the proximal portion and large arteries.
For almost 50 years, selective coronary angiography has remained the clinical "gold standard" for evaluating the coronary anatomy and defining epicardial coronary artery disease. While conventional invasive coronary angiography provides exceptional spatial resolution and a general map of the coronary system, it is expensive and has a small but definite risk of complications. In addition, it requires either a brief hospitalization period or a period of observation for several hours after the procedure in a specialized monitoring unit. The replacement of even a fraction of these procedures with noninvasive imaging modalities would constitute an important advance in the care of patients suspected of having coronary artery disease. Currently, a number of imaging modalities are used for diagnosing epicardial coronary artery disease. Most identify the luminal diameter or stenosis, wall thickness, and plaque volume.1 Since 1999, multi-detector row spiral computed tomography (MDCT) scanners have been available for coronary artery scanning.2 The increased scan speed results in thinner collimated slice widths and an improved spatial and temporal resolution.
Recently, with the introduction of MDCT combined with a subsecond rotation and retrospective electrocardographic (ECG) gating, the invasive modalities have been challenged by an additional new noninvasive assessment of coronary artery stenoses.3 However, the image quality has been insufficient for the reliable detection of coronary stenoses in a substantial number of cases. Calcifications often hinder an evaluation of severely diseased coronary segments, and the coronary arteries are frequently affected by motion artifacts.4-8 In addition, it has been observed that the patient's heart rate during the scan critically influences the image quality.9,10 Therefore, heart rate control is one of the most important factors in better image acquisition. Accordingly, the current technique for image acquisition with MDCT requires pre-medication with beta-blockers.11
This study evaluated the diagnostic accuracy of MDCT angiography in determining significant coronary artery stenoses (≥ 50% lumen diameter narrowing in angiography) and occlusions compared with conventional invasive angiography in Korean patients who had their heart rate controlled with beta-blockers. In addition, the detection rate of computed tomographic coronary angiography (CTCA) in each coronary arterial segment and the detection rate by the location of the stenotic lesion were assessed.
The study was performed prospectively from February to July 2003. CTCA was performed on 61 patients who were suspected of having coronary artery disease (20 - 76 years, mean 59.3 ± 10.0 years). They underwent CTCA, as well as invasive coronary angiography, over a six-month period. The average time between the two examinations was 11 days (range: 1 - 27 days). All the patients were treated with atenolol (25 - 50 mg) and four patients with heart rates higher than 70 bpm received a short-lasting beta-blocker (propranolol 40 mg) prior to imaging. Only those patients in a sinus rhythm, without implanted pacemakers or valve prostheses, and without contraindications to the administration of an iodinated contrast agent were enrolled in this study. Hemodynamicaly unstable patients were excluded and all patients were allowed to continue concurrent medications with no additional medications except for the beta-blockers. The patients who previously had coronary artery stents inserted were included in this study. Twenty-one patients had previously undergone percutaneous transluminal coronary angioplasty with a stent implantation.
CT was performed by using a 16-slice CT (Sensation 16, Siemens, Germany) with 12 × 0.75 mm collimation and 0.42s rotation speed. 120 kV, 500 effective mA, and 2.7 mm/rotation table-feed. Images were reconstructed in the diastole around TI-400 ms with a 0.5 mm increment and a 1.0 mm thickness.
All the data was compared with the results of the invasive coronary angiography. The invasive coronary angiograms were evaluated by a blinded independent observer using quantitative coronary angiography (QCA) and was used as the gold standard for detecting a stenosis. Lesions with a diameter reduction of 50% or more were considered to be significant stenoses. In addition, the reference diameter of the lesion (vessel diameter in the non-diseased artery immediately proximal to the lesion) was documented because only those lesions with a lumen diameter ≥ 2.0 mm were included in the analysis.
An evaluation of the coronary arteries and each of the segments was performed according to the classification of the American Heart Aoosciation.12 Two independent radiologists who were unaware of the results of the invasive coronary angiography evaluated all the MDCT data. By a visual estimation, the coronary arteries were classified according to those that could be evaluated and those that could not. In those arteries that could be evaluated, the presence of significant stenoses (exceeding 50% diameter reduction) was visually assessed and measured. The result was analyzed first by a patient evaluation i.e. how accurately the method detected a patient with coronary artery occlusive disease (CAOD). The overall sensitivity and overall specificity were checked by patient analysis. Second, the results were analyzed according to each coronary artery (LAD, LCx, RCA and Left main trunk) and the sensitivity, specificity, positive predictive value and negative predictive value of each coronary artery was then calculated. Finally the detection rate for stenotic lesion was evaluated depending on the location of the lesion in order to determine if it could influence the detection of stenosis.
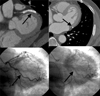
CTCA was performed without complications in all patients (mean age: 59.3 ± 10.0 years, M : F=44 : 17) (Fig. 1). An evaluation of CTCA was possible in 58 out of 61 patients (95%). Invasive coronary angiography indicated 38 patients with significant coronary artery stenoses (1 vessel disease: 17 cases, 2 vessel disease: 11 cases, 3 vessel disease: 10 cases) and 23 patients with a normal coronary artery or minimal coronary artery stenoses (< 50% luminal narrowing). The images of the 3 patients were could not be evaluated due to blurring artifacts, which were due to an increased heart rate during the scanning procedures and motion artifacts. The image acquisition of the major coronary arteries including the left main trunk was available in 229 out of 244 arteries (Table 1).
Table 2 shows a comparison between the MDCT and invasive coronary angiography. CTCA correctly classified 30 out of 35 patients who had significant coronary artery stenoses as having coronary artery stenoses. Five patients who were incorrectly classified by CTCA had only one vessel stenosis. Among the remaining 5 cases, one case had a lesion of a total occlusion in the proximal RCA, which was interpreted as a diminutive RCA. A second case with a stenotic lesion in the PL (posterolateral) branch was not detected because it was located far distal. A misdiagnosis of the third case with a proximal LAD lesion was attributed to motion artifacts. A stenotic lesion at the proximal edge of a previous RCA stent and the lesion of the diagonal branch ostium adjust to the previous proximal LAD stent were not correctly assessed in the fourth and fifth case, respectively. In the last 2 cases, the previously inserted stent interfered with the detection of the coronary artery lesions, known as metallic stent artifact in CTCA. Therefore, by patient analysis, CTCA correctly classified 30 out of 35 patients, who could be evaluated, as having at least one coronary artery stenosis (overall sensitivity 85.7%, overall specificity 91.3%, overall positive predictive value 93.8%, overall negative predictive value 80.8% and accuracy 87.9%) (Table 2) (Fig. 2).
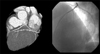
The sensitivity, specificity, positive predictive value and negative predictive value were compared by coronary vessel analysis and the results are shown in Table 3. Image acquisition of the major coronary arteries (LAD, LCx, RCA, Left main trunk) was available in 229 out of 244 (61×4) arteries. CTCA correctly detected 50 out of 62 stenotic coronary artery and an absence of stenosis was correctly identified in 156 out of 167 normal coronary arteries (sensitivity 80.6%, specificity 93.4%, positive predictive value 81.9%, negative predictive value 92.8%). In the LAD, there was a relatively high level of coronary vessels that could not be evaluated (8.2%). On the other hand, it was lowest in the LCx (4.2%). This might be due to the coronary artery calcifications, which were more frequently identified in the LAD than in the other arteries in this study group. Previous reports4 showed the reasons why some segments could not be assessed. The presence of extensive calcifications can complicate a correct assessment of the lumen of the coronary arteries particularly the LAD and motion artifacts of the CTCA developed frequently in the RCA. Occasionally, small sized LCx could not be evaluated using the CTCA modality. The other values showed similar levels. Only one case had a significant stenosis in the Lt. main trunk in invasive coronary angiography (Fig. 3).
The high spatial resolution associated with contrast-enhanced multi-detector row coronary CT angiography may provide a great deal of information on coronary artery stenotic lesions and noninvasive images of the coronary artery wall.13
Recently, Achenbach et al.6 reported a sensitivity of 85% in detecting a significant stenotic coronary artery with contrast-enhanced MDCT in the interpretable native coronary arteries (luminal diameter ≥ 2 mm vessels were assessed) and only 68% of all the coronary arteries could be interpreted. Ropers et al.11 reported a sensitivity of 92% in detecting a significant stenotic coronary artery using contrast-enhanced MDCT in coronary arteries that could be interpreted (luminal diameter ≥ 1.5 mm vessels were assessed). And they reported that 88% of coronary arteries could be evaluated using beta-blockade pre-medication.
This study demonstrated that CTCA allows the detection of coronary artery stenoses and occlusions with a high sensitivity (80.6%) and specificity (93.4%) if sufficient image quality for an evaluation can be obtained. In this study, 93.8% of all coronary arteries could be evaluated with beta-blocker pre-medication. The sensitivity and specificity were similar to those of CTCA in other research centers6-8,11,14-16 but the portion of artery that could be interpreted was relatively higher than in the other results.
In contrast to previous studies, the CTCA results were verified by QCA and all vessel segments, proximal and distal segments, including side branches, were included in the analysis if the vessel diameter measured more than 2.0 mm. The cut off value of 2.0 mm means that stenoses in vessels smaller than 2.0 mm rarely constitute targets for revascularization.17,18
This study demonstrates that in the proximal and mid segments of all 3 major arteries and the left main trunk, CTCA has a high accuracy in excluding coronary artery disease and identifying significant stenoses, but CTCA is relatively limited in the diagnosis of the distal arteries, the side branches and near the previous stent legion. This suggests that stenoses of the relative large vessels were detected more easily by CTCA, suggesting the utility of MDCT as a feasible diagnostic modality and a noninvasive technique for the selection of a revascularization target.
The limitation of CTCA was a calcification of the coronary arteries. In this study, some patients had severe coronary calcification and an accurate evaluation of the CTCA image was difficult, resulting in these lesions often being misdiagnosed as severe stenoses. However, in this group, some patients had only minimal luminal narrowing or did not have a severe coronary stenosis in the invasive coronary angiography. Other studies19 have reported that although this finding was a limitation for an accurate diagnosis using MDCT, the presence of any calcium was strongly suggestive of the presence of atherosclerosis in the coronary artery. Hence, patients with no significant stenoses in the invasive coronary angiography but with detectable calcification by MDCT could be diagnosed with coronary artery disease. This fact might be one of the advantages of CTCA.
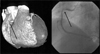
The other limitation was stent imaging. Coronary artery stenting is currently the most common form of non-surgical myocardial revascularization. However, the stent restenosis remains a clinical problem. Therefore, a noninvasive assessment of the stented segment in these patients is highly desirable. It was reported that EBCT (Electron Beam Computed Tomography) was successfully used for a stent patency evaluation but the stent lumen itself could not be accurately visualized.20-22 In this study, 24 of the patients previously underwent coronary stenting in 38 lesions. The radiologists often misdiagnosed the previous stented segments and the luminal narrowing could not be accurately measured. In the presence of intracoronary stents, high-density artifacts, combined with partial volume effects, prevent an adequate assessment of the vessel lumen within the struts of the stent. However, the patency can be assessed if it is enhanced by administering a contrast medium to the vessel segment distal to the stent.4 Although the stent lumen cannot be visualized in most stents, a reliable evaluation of the stent patency is possible by visualizing the distal flow and measuring the attenuation changes in the visible stent lumen and outside the stent. However, the enhancement of the stent distal flow by the antegrade collateral flow in total occluded stents was not correctly assessed. In our study, 33 out of 38 coronary stents (21 patients) could be evaluated using these methods (86.8%) and MDCT correctly classified 31 out of these 33 stents as being either patent (28 stents) or occluded (3 stents) and only two stents were misdiagnosis. Some cases of an in-stent restenosis but with patent distal flow were also classified as being patent by MDCT. Because the stent lumen could be partially visualized in most stents, a reliable evaluation of an in-stent restenosis remains to be assessed in the future.
It is clear that the CTCA is a feasible diagnostic method for detecting coronary artery stenoses with a high sensitivity and specificity under the appropriate heart rate controls. In particular, CTCA showed a high accuracy in the detection of proximal lesion stenoses. However, because most of the segments that could not be evaluated were affected by the coronary motion and coronary artery stents, a further shortening the image acquisition window and technical advances is needed. The non-invasive technique of MDCT for assessing the coronary artery appears to be a useful method for detecting coronary artery stenoses with a high accuracy particularly to the proximal lesions and large arteries. In addition, MDCT angiography is a rapidly developing imaging modality and further technical advances aimed at improving the diagnostic accuracy and clinical utility are expected in the future.23 MDCT angiography is expected to be a good screening modality of coronary artery disease. Besides being a non-invasive alternative, MDCT can offer additional information about the spatial orientation of the vessels and can also identify and quantify the level of calcium deposition within the coronary vessel wall.
Figures and Tables
Fig. 4
Stent patency evaluation by MDCT. The stent patency evaluation was possible by a density measurement and a direct visual assessment in the lumen of the stent.
References
1. Fayad ZA, Fuster V. Clinical imaging of the high-risk or vulnerable atherosclerotic plaque. Circ Res. 2001. 89:305–316.
2. Klingenbeck-Regn K, Schaller S, Flohr T, Ohnesorge B, Kopp AF, Baum U. Subsecond multi-slice computed tomography: basics and applications. Eur J Radiol. 1999. 31:110–124.
3. Knez A, Becker CR, Ohnesorge B, Haberl R, Reiser M, Steinbeck G. Noninvasive detection of coronary artery stenosis by multislice helical computed tomography. Circulation. 2000. 101:221–222.
4. Nieman K, Oudkerk M, Rensing BJ, Ooijen P, Munne A, Geuns RJ, et al. Coronary angiography with multislice computed tomography. Lancet. 2001. 357:599–603.
5. Kopp AF, Schroeder S, Kuettner A, Baumbach A, Georg C, Kuzo R, et al. Non-invasive coronary angiography with high resolution multidetector-row computed tomography. Eur Heart J. 2002. 23:1714–1725.
6. Achenbach S, Giesler T, Ropers D, Ulzheimer S, Derlien H, Schulte C, et al. Detection of coronary artery stenoses by contrast-enhanced, retrospectively ECG-gated, multi-slice spiral CT. Circulation. 2001. 103:2535–2538.
7. Knez A, Becker CR, Leber A, Ohnesorge B, Becker A, White C, et al. Usefulness of multislice spiral computed tomography angiography for determination of coronary artery stenoses. Am J Cardiol. 2001. 88:1191–1194.
8. Vogl TJ, Abolmaali ND, Diebold T, Engelmann K, Ay M, Dogan S, et al. Techniques for the detection of coronary atherosclerosis: multi-detector row CT coronary angiography. Radiology. 2002. 223:212–220.
9. Schroeder S, Kopp AF, Kuettner A, Burgstahler C, Herdeg C, Heuschmid M, et al. Influence of heart rate on vessel visibility in noninvasive coronary angiography using new multislice computed tomography: experience in 94 patients. Clin Imaging. 2002. 26:106–111.
10. Giesler T, Baum U, Ropers D, Ulzheimer S, Wenkel E, Mennicke M, et al. Noninvasive visualization of coronary arteries using contrast-enhanced multidetector CT: Influence of heart rate on image quality and stenosis detection. Am J Roentgenol. 2002. 179:911–916.
11. Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, Ohnesorge B, et al. Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003. 107:664–666.
12. Detre KM, Wright E, Murphy ML, Takaro T. Observer agreement in evaluating coronary angiograms. Circulation. 1975. 52:979–986.
13. Becker CR, Ohnesorge BM, Joseph Schoepf U, Reiser MF. Current development of cardiac imaging with multi-detector row CT. Eur J Radiol. 2000. 36:97–103.
14. Achenbach S, Moshage W, Ropers D, Nossen J, Daniel WG. Value of electron-beam computed tomography for the detection of high-grade coronary artery stenoses and occlusions. N Engl J Med. 1998. 339:1964–1971.
15. Ha JW, Cho SY, Shim WH, Chung N, Jang Y, Lee HM, et al. Noninvasive evaluation of coronary artery bypass graft patency using three-dimensional angiography obtained with contrast-enhanced electron beam CT. Am J Roentgenol. 1999. 172:1055–1059.
16. Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, de Feyter PJ. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation. 2002. 106:2051–2054.
17. Reddy G, Chernoff DM, Adams JR, Higgins CB, et al. Coronary artery stenoses: assessment with contrast-enhanced electron-beam CT and axial reconstructions. Radiology. 1998. 208:167–172.
18. Schmermund A, Rensing BJ, Sheedy PF, Bell MR, Rumberger JA. Intravenous electron-beam computed tomographic coronary angiography for segmental analysis of coronary artery stenoses. J Am Coll Cardiol. 1998. 31:1547–1554.
19. Rumberger JA. Noninvasive coronary angiography using computed tomography Ready to kick it up another notch? Circulation. 2002. 106:2036–2038.
20. Pump H, Mohlenkamp S, Sehnert CA, Schimpf SS, Schmidt A, Erbel R, et al. Coronary arterial stent patency: assessment with electron-beam CT. Radiology. 2000. 214:447–452.
21. Mohlenkamps S, Pump H, Baumgart D, Haude M, Gronemeyer DH, Seibel RM, et al. Minimally invasive evaluation of coronary stents with electron beam computed tomography: in vivo and in vitro experience. Catheter Cardiovasc Interv. 1999. 48:39–47.
22. Maintz D, Juergens KU, Wichter T, Grude M, Heindel W, Fischbach R. Imaging of coronary artery stents using multislice computed tomography: in vitro evaluation. Eur Radiol. 2003. 13:830–835.
23. Fayad ZA, Fuster V, Nikolaou K, Becker C. Computed tomography and magnetic resonance imaging for noninvasive coronary angiography and plaque imaging: Current and potential future concepts. Circulation. 2002. 106:2026–2034.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download