Abstract
Esophageal duplication cysts are congenital anomalies of the foregut that are rarely found in the abdomen. An accurate preoperative diagnosis is not always possible, so the definitive diagnosis can be made by histologic examination of the surgical specimen. We experienced a case of Intra-abdominal esophageal duplication cyst in a 52-year-old female, who initially presented with an esophageal submucosal tumor on upper gastrointestinal endoscopy. She did not have any gastrointestinal symptoms. Barium esophagography, chest computed tomography scan and endoscopic ultrasonography demonstrated the cystic lesion in the intra-abdominal esophagus. Transhiatal enucleation of the lesion was performed successfully via the abdominal approach with no postoperative complications. Histologic study showed that the cyst wall contained a two-layered muscle coat and the surface of the lumen was lined by pseudo-ciliated columnar epithelium. The patient has been doing well without any complaints for 3 months of follow-up period.
Esophageal duplication cysts, first described in 1711, are rare developmental anomalies of the foregut that constitute 0.5-2.5% of all esophageal tumors.1 Autopsy studies reported an incidence of one in 8,200.2 Esophageal duplication cysts are usually found in the mediastinum but rarely in the abdomen.3
Congenital esophageal cysts can be classified as duplication, bronchogenic, gastric and inclusion cyst.2 To be diagnosed as the duplication cyst, a lesion must meet the following criteria. 1) attachment to the esophagus, 2) epithelium representing some level of the gastrointestinal tract, 3) presence of two layers of muscularis propria.1 Duplication cyst may be confused with bronchogenic cyst, but, histologically, the presence of cartilage plates and seromucous respiratory glands favors the bronchial origin.4
We hereby present a case of an intra-abdominal esophageal duplication cyst successfully treated by transhiatal enucleation.
A 52-year-old woman was referred to our hospital because of findings on an upper gastrointestinal endoscopy, performed for a routine health check-up at a local community hospital, showed a submucosal tumor with no ulceration in the distal esophagus. The patient denied any history of gastrointestinal disturbances including dysphagia and epigastric pain. Physical examination and routine laboratory studies were unremarkable.
Barium esophagography showed a well defined filling defect arising from the anterior left side of the distal esophagus (Fig. 1). The chest computed tomography (CT) scan revealed a unilocular cystic mass, measuring 4×3 cm, and it was not enhanced by contrast dye (Fig. 2). Endoscopic ultrasonography (EUS) demonstrated a heterogenous hypoechoic mass within the muscularis propria of the esophagus.
On exploration, a 4×3 cm sized, cystic mass was found just proximal to the gastroesophageal junction within the muscular layers of the intraabdominal esophagus. The muscular layers were divided to expose the surface of the tumor. The mass was then successfully enucleated without any injury to the mucosal-submucosal layer (Fig. 3). The consistency of the esophageal wall was confirmed by an injection of gentian violet dye through a nasogastric tube. The defect of the muscular layers were repaired with 3-0 silk interrupted sutures.
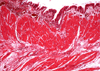
The cyst itself was filled with thick mucinous content. The histologic findings were consistent with the features of a duplication cyst. The cyst wall contained a two-layered muscle coat (Fig. 4) and the surface of the lumen was covered by a lining of pseudo-ciliated columnar epithelium.
Upon follow-up barium esophagography performed on 6th postoperative day, there was no leakage or stenosis in the distal esophagus (Fig. 5). The patient was discharged on 9th postoperative day without any complications. She has been doing well during a follow-up period of three months.
Esophageal duplication cysts arise from developmental disturbances between the fifth and eighth weeks of embryonic life. During this period, vacuoles develop within the solid esophagus and these normally coalesce longitudinally to form the esophageal lumen. When a vacuole persists, an intramural esophageal cyst may develop and form a true duplication.4,5
Most esophageal cysts are in the lower third (60%) and do not communicate with the lumen (90%).6 Although usually asymptomatic, they may cause respiratory or gastrointestinal symptoms. On rare occasions, acute chest pain and arrhythmia may be readily confused with other conditions.7
The preoperative diagnosis is based on the radiologic findings and on endoscopy. Plain chest X-ray and barium esophagography often reveal a mass lesion. CT scan and MR imaging are useful methods for excluding malignancy, but these modalities are not always reliable because depending on the cyst contents, the attenuation values on CT and the signal analysis on MR imaging are variable.8 EUS usually reveals an air-fluid interface or echo density of fluid within the lesion. It is important that there is continuity between the muscularis propria of the esophagus and that of the cyst wall.9
Although infrequent, complications such as infection, perforation, bleeding and malignancy have been reported,10 surgical excision is strongly recommended whether symptomatic or not. The muscular edges of the esophagus should be approximated to prevent a pseudo-diverticulum after enucleation of the esophageal cyst.11 Puncture and drainage of the cyst, guided by endoscopy or CT, can be the alternative option in patients with high surgical risks or those who refuse surgery.10
Figures and Tables
Fig. 1
A barium esophagography shows a well defined intramural lesion with an intact mucosa in the lower third of the esophagus (arrow).

Fig. 2
Chest CT scan shows a homogenous, low density mass anterior to the intra-abdominal esophagus.

Fig. 3
The defect of the muscular layer is shown in the intra-abdominal esophagus (arrow). During the procedure, there was no injury to the mucosal-submucosal layer.

References
1. Whitaker JA, Deffenbaugh LD, Cooke AR. Esophageal duplication cyst. Case report. Am J Gastroenterol. 1980. 73:329–332.
2. Arbona JL, Fazzi JG, Mayoral J. Congenital esophageal cysts: case report and review of literature. Am J Gastroenterol. 1984. 79:177–182.
3. Harvell JD, Macho JR, Klein HZ. Isolated intra-abdominal esophageal cyst. Case report and review of the literature. Am J Surg Pathol. 1996. 20:476–479.
4. Salyer DC, Salyer WR, Eggleston JC. Benign developmental cysts of the mediastinum. Arch Pathol Lab Med. 1977. 101:136–139.
5. Tapia RH, White VA. Squamous cell carcinoma arising in a duplication cyst of the esophagus. Am J Gastroenterol. 1985. 80:325–329.
6. Nelms CD, White R, Matthews BD, Ballinger WE Jr, Sing RF, Heniford BT. Thoracoabdominal esophageal duplication cyst. J Am Coll Surg. 2002. 194:674–675.
7. Kolomainen D, Hurley PR, Ebbs SR. Esophageal duplication cyst: case report and review of the literature. Dis Esophagus. 1998. 11:62–65.
8. Janssen H, Fiedler PN. Isolated intraabdominal esophageal cyst. Am J Roentgenol. 1998. 170:389–390.
9. Bhutani MS, Hoffman BJ, Reed C. Endosonographic diagnosis of an esophageal duplication cyst. Endoscopy. 1996. 28:396–397.
10. Diaz de Liano A, Ciga MA, Trujillo R, Aizcorbe M, Cobo F, Oteiza F. Congenital esophageal cysts-two cases in adult patients. Hepatogastroenterology. 1999. 46:2405–2408.
11. Cioffi U, Bonavina L, De Simone M, Santambrogio L, Pavoni G, Testori A, et al. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest. 1998. 113:1492–1496.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download