Abstract
As the Korean government's recognition of the importance of hospice service grows, the government has initiated a variety of hospice services in Korea. Each hospice organization has shown a significant difference in its health care delivery methods, constitution and care content. Developing a clinical protocol is essential for establishing standardized hospice services. A preliminary protocol was drawn up by examining the records of terminal patients (n=541) in a home hospice organization while elucidating the health problems as well as classifying them through the Home Health Care Classification (HHCC), and by reviewing the relevant nursing interventions and medical treatments in the literature concerning the clinical protocols. Korea's leading hospice specialty groups participated in four rounds of content validity verification processes in order to establish a protocol. A guideline was developed through a team approach, integrating the opinions of doctors, nurses, ministers, volunteers, patients' families, nutritionists and pharmacists. Eighteen health problems and a total of 223 interventions (173 major treatments and nursing interventions, and 50 optional interventions) were included in the final clinical protocol. This study is expected to contribute to the overall qualitative improvement of home hospice care and the subsequent shortening of documentation time. Evaluation tools and a regulatory feedback system need to be developed in order to maintain consistent evaluation procedures based on the continuous promotion and use of the protocol.
The primary cause of death in Korea is cancer, and its mortality rate has consistently increased over the last decade to a total of 131.9 per 100,000 persons.1 As people with advanced stages of cancer approach their impending death, they often experience severe distress, not only physically but also with respect to the psychological, spiritual, social and financial aspects. Due to immense burdens that cancer patients and their families encounter, specialized treatment services as well as effective and systematic management plans for terminal cancer patients are urgently needed in order to maximize their quality of life within the limits of their unique physical conditions. Hospice care is one of the most suitable care regimens in this regard.2 Hospice care gives specialized and holistic care for a dying person in that it provides the patients and their families with legal, financial, emotional and spiritual counseling in addition to meeting the patients' immediate physical needs.3
64 such institutions are presently operating through out Korea. Forty of these institutions are affiliated with medical centers, and 29 such institutions provide home hospice services. Each hospice organization exhibits significant differences with respect to the organization and delivery of care providers and the content and quality of services, and as well as employing differing service models such as home hospital team care service, hospice units in hospital, services scattered through a hospital and independent operations.4 However, the current shortage of home hospice services in Korea demonstrates the ineffectiveness of the Korean health care delivery system in providing timely and efficient interventions for the terminal patients when compared to other developed countries.5 The government began to recognize the importance of hospice services, and so it began to develop a demonstration project in 2002. A balanced systematic financial support system and standardized in management for consistent quality of care are important tasks to achieve this goal. Standardization of hospice care such as developing clinical protocols is essential not only for providing terminal patients and their families with quality hospice care, but also for assisting the government and health care providers to more effectively utilize medical resources.
Research has shown that pain, fatigue, dyspnea and constipation are among the most common symptoms experienced by the patients with cancer that are receiving hospice care.6,7 A number of emotional problems such as worry (73%), sadness (67%), nervousness (62%), sleeping difficulties (53%), irritability (47%), and difficulty in concentrating (40%) have been identified for the people with cancer.8 Symptom distress is the strongest predictor of the overall quality of life for people with advanced cancer as well.9 Substantial research studying the prevalence of symptom distress for patients with terminal cancer or for patients receiving home care has been performed, but there has been little research that has focused on their health problems together with the related interventions that the patients and their families experience with hospice care in a home setting.
One study developed a home health care nursing intervention list that was compiled through an analysis of home health care nursing records, and it identified 43 categories of nursing diagnoses that were used 595 times with 2, 814 nursing interventions, which indicated a statistical mean of 4.73 nursing interventions per diagnosis.10 Forty percent of the subjects in this research project were cancer patients and the others had various diseases, so the findings do not exactly fit certain home hospice care interventions. In comparison, research on home care nursing interventions for hospice and general patients according to the Nursing Intervention Classification (NIC) system, found that 2380 nursing interventions were used for hospice patients and 8725 nursing interventions were used for general home care patients.11 This study showed that there was a lack of specialized hospice nursing interventions for such needs as emotional, family and spiritual support and care for end-of-life hospice patients. A comparative study between nursing interventions for terminal cancer patients in hospice units and general hospital units using the NIC found that hospice units provided more comprehensive nursing interventions including psychological, spiritual and family care as well as providing physical care for the terminal cancer patients than did the general hospital units.12 Nursing interventions that were conducted in hospice units used more multidisciplinary care conferences than did the general hospital units.
The Home Health Care Classification (HHCC, Saba 1992) system has been approved by the American Nurses Association and the American National Standards Institute Healthcare Informatics Standards Board.13 The HHCC system's two taxonomies make it possible not only to assess and document intervention, but also to code, index, classify, link and map the care process according to 20 care component concepts.14 Therefore, the development of standardized clinical protocols for home hospice care is necessary, and the HHCC system is appropriate for application to home hospice protocols.
The purpose of this study is to develop clinical protocols for the home hospice care required for effective home hospice services in Korea. The study's specific purposes are as follows: 1) To describe the major problems of home hospice recipients by classifying the health problems of patients and their families according to the HHCC system; 2) To develop a preliminary protocol by connecting each health problem with its definition, nursing interventions and treatment, and the expected outcomes; and 3) To develop a clinical protocol for home hospice care through a thorough content validity verification process
A total of 778 patients' medical and nursing records spanning 12 years, from 1988 to June 2000, were collected from a home hospice organization located in a university hospital in Korea. From these files, 237 records were found to lack documentation of the deduced health problems and they did not adequately describe interventions; thus, only 541 records were selected for inclusion to our study. The experts chosen to verify the content validity of the guideline consisted of 37 members, including board members of the Korean Society for Hospice and Palliative Care, board members of the Korean Hospice Nurses Association, members of the Korean Hospice Association, and nurses affiliated with the Catholic Hospice Association.
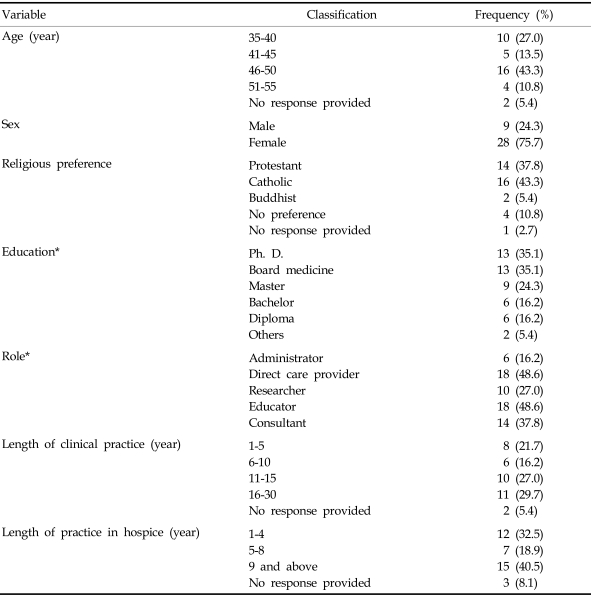
The general characteristics of the experts who participated in verifying the content validity of the clinical protocol in this study are presented in Table 1. 37 experts from various fields of expertise participated in the four rounds of the validity verification process. Thirteen (35.1%) of them were doctors of family medicine, oncology, anesthesiology and surgery. More than a third of the experts were doctoral degree holders. Nearly half were engaged in direct nursing and associated education roles; this was followed by professionals in consulting (37.8%) and research roles (27.0%). In terms of activity types, 21 (56.8%) provided hospice services by visiting homes, 14 (37.8%) were professors and 12 (32.4%) provided hospice services in a hospital. The average clinical career of the panel members was 12.4 years, and the average period of hospice focused activities aside from clinical practice was 6.7 years.
Measurement: This study analyzed the major health problems of hospice recipients according to the HHCC format, we matched primary health problems with related nursing and treatment interventions, and then we verified the nursing and treatment validity. Nursing interventions were reorganized into 60 major classifications as well as 100 sub-classifications, and intervention activities were reclassified into the following four areas: assessment (the collection and analysis of data concerning health conditions), direct nursing (the performance of treatment activities), education (the transfer of knowledge and skills), and management (mediation and referral).15 The experts graded the intervention names, the definitions of the interventions and the intervention activities from 1 (not important) to 5 (very important) in accordance with the associated health problems.
Procedure: The research procedure is shown by a flow chart (Fig. 1).
Data analysis: Descriptive statistics were produced for the major health problems of patients under home hospice care and descriptive statistics were also produced on the general characteristics of the participants. Fehring's method was used to estimate the experts' content validity. Numbers were assigned as the response values to our queries: 5=1, 4=.75, 3=.50, 2=.25 and 1=0. We summed the points answered for each item, divided them by the total number of respondents and calculated the Index of Content Validity (ICV) for each item.16
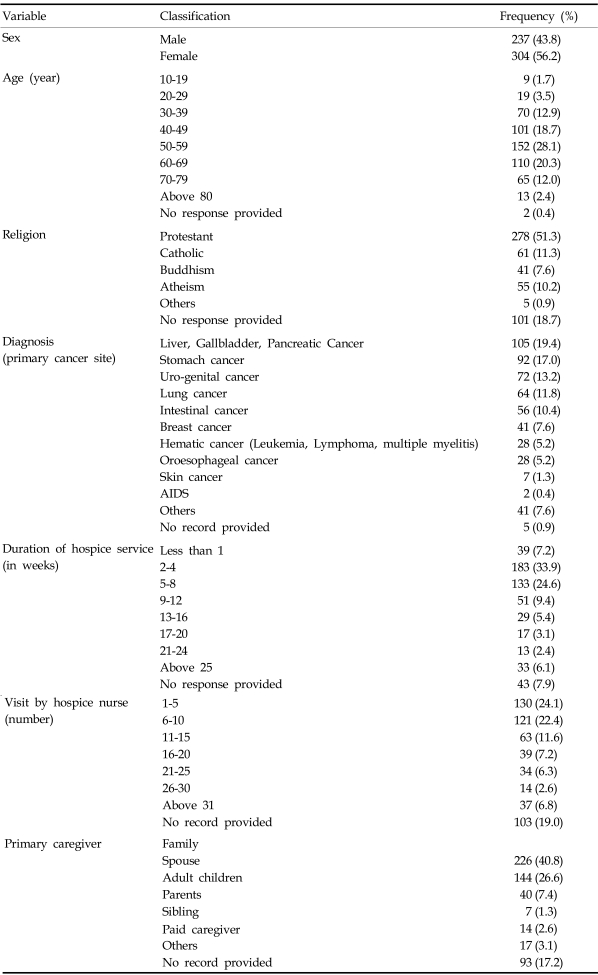
The general characteristics of the 541 patients whose treatment and nursing records were used in this study are presented in Table 2. The general characteristics of the hospice recipients were categorized as follows: the gender (304 females; 56.2%, 237 males; 43.8%) and age (10 to 80) were diverse, and the majority of recipients ranged between 40 and 69 years of age (67.1%). In terms of distribution by medical diagnoses, liver, gall bladder and pancreatic cancer were the most frequent diagnosis (19.4%), and this was followed by gastric cancer (17%), and urinary system and genital cancer (13.3%). Metastases occurred in 28.7% of the total cases reviewed.
A total of 86 health problems were identified, and the 20 highest rankings of health problems accounted for 88.2% of the total in terms of frequency. Pain was identified as the most common problem by 408 recipients (75.5%). Malnutrition (44.6%), skin damage (30.9%), constipation (26.8%), ineffective coping by family members (22.4%), spiritual distress (21.5%), ineffective breathing (19.0%), dysuria (16.6%), insecurity (12.9%), motor function disturbance (11.8%), fluid volume excess (8.5%), sleep disturbance (7.2%), lack of family support resources (5.7%), risk of infection (5.0%), fluid volume deficit (4.8%), oral mucous membrane impairment (4.6%), abdominal distension (4.6%), skin integrity impairment risk (3.9%), activity intolerance (3.7%), and caregiver role strain (3.5%) were ranked after pain.
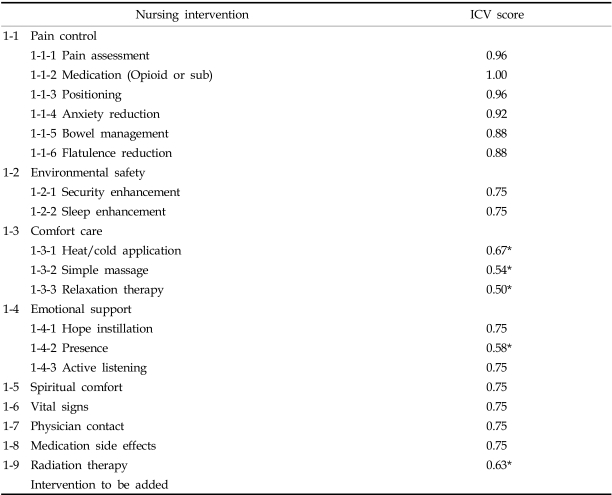
A preliminary clinical protocol that classified the health problems of hospice recipients according to the HHCC components was also developed. It presented the definitions, symptoms goals and intervention names of the health problems as well as the definitions of the interventions, and we recorded the types of intervening activities. Only the example of "pain" is shown in Table 3. The following 17 components and 19 health problems were included: pain, malnutrition, skin damage disturbance, constipation, family coping impairment, spiritual distress, inefficient breathing, dysuria, ineffective patient coping, motor function disturbance, insecurity, sleep disturbance, fluid volume excess, lack of knowledge related to the progress of disease, failure to implement medication, risk of infection, danger of injury, swallowing impairment, and danger of medication side effect.
As predicted in the preliminary clinical protocol, the first content validity verification processreached agreement on 19 health problems and their associated interventions. The content validity concerning 291 intervention names was agreed upon by using ICV points that identified the definitions. Of these, 241 (84%) intervention items scoring over 0.75 ICV points were identified and described by the major intervention names. The remaining 50 intervention items that scored below 0.75 ICV points were classified as optional interventions.
Based on the ICV points agreed upon during the first content validity round, it was necessary to revise and supplement the protocol according to the characteristics of hospice services rather than limiting it to the HHCC format The expert panel convened for a workshop where the following three points were agreed upon: (1) medication prescribed for hospice recipients would be included into the contents of protocols so that the practitioners could use the protocol more effectively; (2) a cooperative attitude and mutual respect component such as acknowledging each other's specialty or particular expertise and cooperating with each other would be added since hospice care is based on a team interventional approach; and (3) the clinical protocol should be approached as a holistic care regimen rather than a classification by internal organs or diseases. The panel members subsequently reflected upon the outcomes of the collected opinions, and then they revised and merged the contents of the preliminary protocols. As a result, the 19 health problems in the preliminary protocol were then revised to 18 problems. The intervention names were reduced from 241 items to 234 while only 207 were selected as major intervention names, and the other 27 were prescribed as optional interventions. In addition, the definitions, symptoms and related factors underlying the health problems as well as definitions of the intervention names were revised and supplemented.
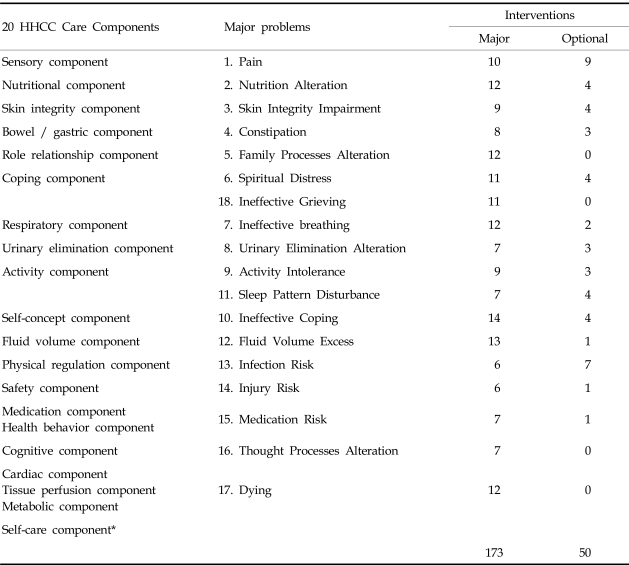
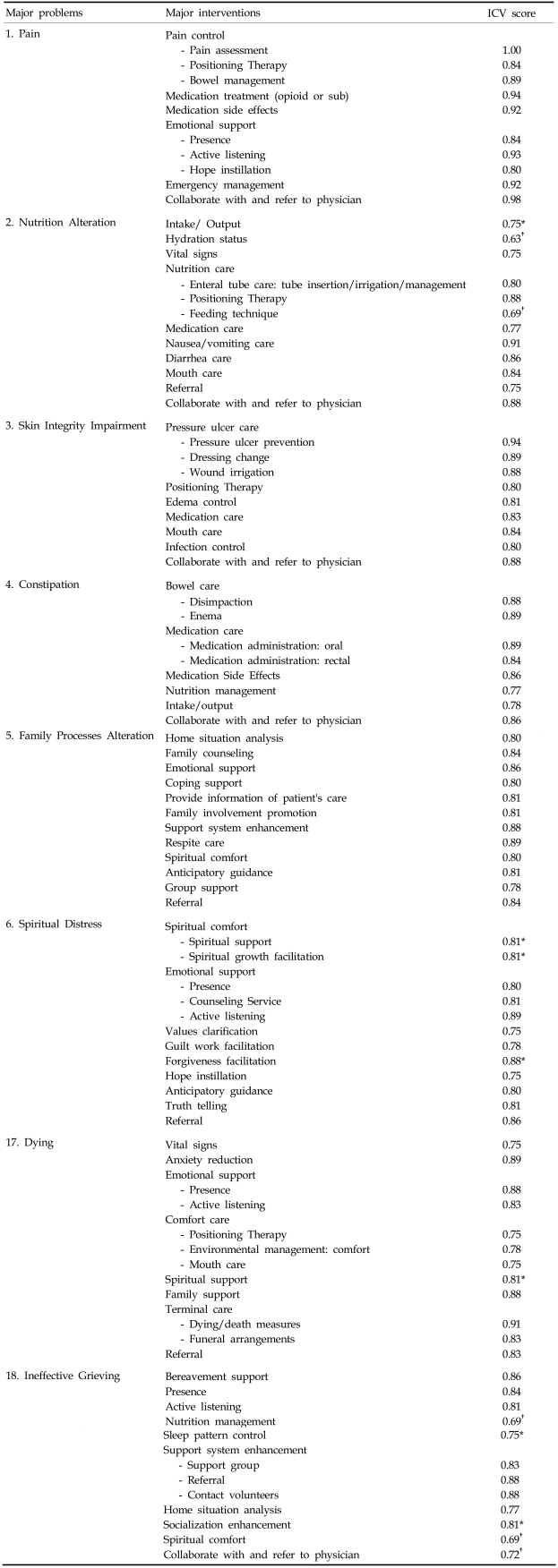
Through the third validity verification process, 50 (21%) out of 234 intervention items were areas of physician-nurse disagreement; in other words, the ICV points of those intervention items were scored as less than 0.75 by the physicians' group while they were scored as over 0.75 by the nurses' group. Problems such as spiritual distress, ineffective individual coping, pain, nutrition alteration and skin integrity impairment were the source of high levels of physician-nurse disagreement for their interventions. To reevaluate the items that physicians and nurses disagreed upon, the Delphi technique was used and the items were transferred into a 5-point scale. The fourth content validity verification results were not significantly different from the third validity verification; only 7 out of 50 items with disagreement scored over an 80% agreement rate. Thirty five out of the 43 major intervention items that were disagreed upon were changed to optional interventions, and 8 major interventions were retained according to the holistic philosophy of hospice care; therefore, interventions in the final guideline after the fourth validity round included 173 major interventions and 50 optional ones, leading to a total of 223 (Table 4).
Table 5 presents the final clinical protocol for home hospice care. Eight of the major health problems in hospice care with their major interventions are presented from all 18 problems due to the space limitations for the article. These ICV scores were the results of the final validity tests.
The usefulness of Saba's HHCC system has been proven for home care nursing recipients with its various clinical diagnoses, its easy format and its systematic recording. Classifying and computerizing the interventions of hospice care by using the HHCC format was much simpler, effective and easy than using the NIC format. In spite of the usefulness of HHCC, limitations of the HHCC system existed such as the difficulties on the part of the hospice members in accurately understanding of contents for linking diagnoses with the interventions. When the HHCC intervention lists related to the major health problems in hospice care were compared with the system's contents that showed the relevant interventions in the Oxford textbook of palliative medicine, in the hospice care guidelines, and in the hospice care handbooks, the overall interventions must be referred to and supported by linkages between the NANDA diagnoses and the NIC interventions introduced in the NIC 3rd ed.17
Using the HHCC system as the basic classification format of this study, the 18 health problems of health care recipients were divided into 20 care components. Considering the characteristics of the hospice recipients, problems of the cardiac, metabolic and tissue perfusion components could not be seen as peculiar symptoms even though most patients suffered from complex problems due to the progressive nature of their cancers. In response, the researchers developed a new problem "dying" that involved those three components considered as complex problems of terminal patients close to death. Researchers also created a new problem identified as "ineffective grieving" because bereavement care, which is essential to hospice care, was not included in the HHCC.
A standardized clinical protocol of home hospice care was developed after four rounds of an internal content validity process by hospice experts. The items receiving greater than 60% and less than 80% agreement rate after the first round of content validity were classified as optional interventions. Optional interventions were concerned with the health problems of pain included sleep aids, hot/cold application, simple massage, simple relaxation therapy, security reinforcement, and radiation therapy care. For the health problem of nutrition alteration the ICV point of intervention "environmental safety" was 0.5; indicating a low agreement rate. A lack of understanding of the intervention names was proven through the study of "Korean Language Validity on HHCC", which was the basis of this study.18
In the second content validity verification, the specific names of medicines used for medication intervention were inserted in the guideline so that they could be used effectively in the practical affairs of home hospice intervention delivery methods. The experts considered it appropriate to put "individual coping impairment" and "insecurity" into the health problem category of "inefficient reaction of the individual" because those two elements had many interventions in common. They also decided to include "swallowing impairment" into "inefficient breathing". The problems "lack of knowledge related to the progress of diseases" and "failure to implement medication" were deleted because of their low priority in hospice care.
This study was based on a multidisciplinary team approach as being the basic philosophy of hospice and the hospice protocol was developed with the participation of physicians, nurses, pharmacists, nutritionists, ministers, social workers and volunteers. However, many items of disagreement between physicians and nurses were presented in the outcomes of content validity verification section. This indicated the differences of the underlying perspectives and roles between the physicians and nurses. Collaboration between physicians and nurses ensure quality care and cost effectiveness. It is especially critical that physicians and nurses share the same philosophy in hospice care in order to promote an effective team approach. Therefore, the exchange of mutual opinions through open and clear communication channels has to be established among of hospice service members, and systematic education regarding hospice philosophy is needed.
An intervention "refer to volunteer" was also added to the interventions presented in the category "ineffective grieving" in order to utilize resources of volunteers because well educated, mature and experienced volunteers are a valuable resource necessary for effective home hospice care.
This study recognized the basic philosophy of hospice as holistic care with respect to the physical, psychosocial and spiritual aspects of patients during their end-of-life experience. For example, interventions for pain in this protocol consisted not only of physical treatments such as flatulence reduction, vital signs, sleep enhancement, heat/cold application and simple massage but also of emotional support such as being present, actively listening, instilling hope and offering spiritual support.
A limitation of this study was that these clinical protocols are not reflected in all the hospice services offered by every institution in Korean because few institutions met the required terms of organizing hospice teams and holding regular conferences. A reluctance to share data was noted in some institutions, and it was discovered that documentation was not put into practice even though many of the interventions were offered to hospice recipients in practice. Differences arose when we looked into the problems of the recipients due to different educational backgrounds and experiences of the hospice nurses that were recording the problems.
In conclusion, this study developed a Korean clinical protocol for home hospice care through a content validity verification process done by Korea's leading hospice specialty groups. The clinical protocols based on the HHCC system consist of 19 care components, 18 health problems categories, 173 major interventions, and 50 optional interventions. This clinical protocol of home hospice care can be used as the basic database for systematizing hospice care; it can also serve to influence policy development by the Korean government for dealing with the practical affairs necessary for offering hospice services using hospice models. The protocol's usefulness and thoroughness is currently being evaluated by various home hospice agencies for further development. Future studies should focus on the continuous use and evaluations of the clinical protocols in order to eventually establish a unified Koreanized hospice clinical protocol. Research on the computerization of the protocol would provide information on the ways to deliver consistent and effective hospice care. Policies on hospice training/education and research concerning hospice service financing are also required.
ACKNOWLEDGEMENT
The authors wish to acknowledge Mira Lee, Young Jin Kim, the Board members of the Korean Society for Hospice and Palliative Care, the Korea Hospice Association, the Catholic Hospice Association, and the Korean Hospice Nurses Association for their support throughout this study.
References
1. Korea National Statistical Office. Korea Statistical Yearbook. 2002. Seoul: Statistical Publication Div..
2. Korean Society for Hospice and Palliative Care. Dying with dignity-Hospice Guide -. 2003. Seoul: Institute of Korean Medicine.
3. National Hospice Organization. Standards of a hospice program of care. Hosp J. 1994; 9:39–74.
4. Yun Y, Choi E, Lee Y, Lee J, You C, Kim H, et al. Survey on the Quality of Hospice · Palliative Care Programs in Korea. Korean J Hospice and Palliative Care. 2002; 5:1.
5. Ministry of Health and Welfare. A Guide of Pilot Project for Hospice Service. 2003.
6. Donnelly S, Walsh D, Rybicki L. The symptoms of advanced cancer in 1,000 patients. J Palliat Care. 1994; 10:57. PMID: 8089819.
7. Weitzner M, Moody L, McMillan S. Symptom management issues in hospice care. Am J Hosp Palliat Care. 1997; 4:190–195. PMID: 9295429.

8. Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu F, et al. The Memorial Symptom Assessment Scale: An instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994; 30A:1326–1336. PMID: 7999421.

9. McMillan SC, Small BJ. Symptom distress and quality of life in patients with cancer newly admitted to hospice home care. Oncol Nurs Forum. 2002; 29:1421–1428. PMID: 12432413.

10. Park HG, Kim CJ, Kang GS, Sin HS. Development of a home health care nursing intervention list through analysis of home health care nursing records. J Korean Acad Fund Nurs. 2001; 8:402–415.
11. Yong JS, Ro YJ, Han SS, Kim MJ. A comparison between home care nursing interventions for hospice and general patients. J Korean Acad Nurs. 2001; 31:897–911.

12. Ro YJ, Han SS, Yong JS, Song MS, Hong HU. A comparison of nursing Interventions with terminal cancer patients in a hospice unit and general units. J Korean Acad Adult Nurs. 2002; 14:543–553.
13. Saba VK. The classification of home health care nursing diagnosis and intervention. Caring. 1992a; 11:50–57. PMID: 10183631.
14. Saba VK. Nursing classifications: Home Health Care Classification System (HHCC): an overview. Online J Issues Nurs. 2002; 7:9. PMID: 12410634.
15. Saba VK. Home Health Care Classification. Caring. 1992b; 11:58–60. PMID: 10117730.
16. Fehring RJ. Method to validate nursing diagnosis. Heart Lung. 1987; 16:625–629. PMID: 3679856.
17. McCloskey JC, Bulechek GM. Nursing Interventions Classification (NIC). 2000. 3rd ed. Philadelpia: Mosby.
18. Park HY, Kim JY, Hwang JY, Choi YH, Lee HR, Park HK. Home Health Care Classification standardization and validity study of Korean nomenclatures of the Home Health Care Classification. J Korean Acad Adult Nurs. 1999; 11:52–66.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download