Abstract
This study was performed to analyze the efficacy of the prophylactic use of octreotide (Novartis, Stein, Switzerland) for pancreatic fistula following a pancreaticoduodenectomy. The medical records of 190 patients who underwent a pancreaticoduodenectomy at the Samsung Medical Center in Seoul, Korea between January 2000 and December 2002 were reviewed. Patients were divided into either the octreotide (n = 81) or control group (n = 109). The octreotide group received subcutaneous injections of 100 µg of octreotide every 12 hours for more than five days after surgery. The control group was not treated with octreotide. The criterion of pancreatic fistula was the drainage of the amylase rich fluid, over 500 U/mL in the three days after surgery. The morbidity and mortality rates were 32.1% and 1.2% in the octreotide group and 31.2% and 0% in the control group, respectively. Pancreatic fistula was the second most common complication (8.4%). In the univariate analysis, octreotide was ineffective in reducing pancreatic fistula (p = 0.26). However, in the multivariate regression analysis, combined gastrectomy (p = 0.018), cellular origin of the disease (p = 0.049), and use of octreotide (p = 0.044) were the risk factors that increased the frequency of pancreatic fistula. Therefore, the routine use of octreotide after a pancreaticoduodenectomy should be avoided until a worldwide consensus is established.
Pancreatic fistula after a pancreaticoduodenectomy is a common, but dangerous complication.1-3 The major causes of mortality after a pancreaticoduodenectomy are intra-abdominal sepsis or hemorrhage, which frequently precedes pancreatic fistula.4,5 These complications also prolong the hospital stay after surgery. Thus, pancreatic surgeons have been interested in the prevention of pancreaticoduodenectomy-related pancreatic fistula. Several techniques and modifications for the management of the residual pancreas have been developed.6-9 However, a standard technique for the reduction of pancreatic fistula has not yet been determined.
The outcome of clinical trials evaluating the efficacy of various drugs for the prevention of fistula formation remains controversial. Although prospective randomized studies conducted in Europe showed that perioperative treatment using octreotide as a prophylaxis was associated with a lower incidence of pancreatic fistula,10-13 the prospective randomized placebo-controlled studies performed in North America revealed that the prophylactic use of octreotide should be eliminated.14,15 Even meta-analysis studies showed contradictory results in the effectiveness of prophylactic octreotide.16-18
In our hospital, the synthetic somatostatin analogue octreotide19 has been used since 1995 for the prevention of pancreatic fistula associated with a pancreaticoduodenectomy. Recently, the use of octreotide has increased due to the propensity of individual surgeons. Here, we evaluate the efficacy of octreotide, administered after a pancreaticoduodenectomy, in preventing pancreatic fistula. In this study, pancreatic fistula refers to the drainage of more than 500 U/mL of amylaserich fluids during the three days after surgery or overt clinical findings, regardless of the amount of turbid drainage fluid, leukocytosis, erosion of the skin, etc.
Between January 2000 and December 2002, 237 patients underwent a pancreaticoduodenectomy in the Department of Surgery at Samsung Medical Center in Seoul, Korea. The following patients were excluded from the study: 16 patients who had a total pancreatectomy and 31 patients treated with octreotide for less than five days or without immediate treatment after the operation. The remaining 190 patients were examined. The control group included 109 patients who had never received octreotide, while the octreotide group consisted of 81 patients treated with octreotide, via a subcutaneous injection of 100 µg every 12 hours for more than five days (9.38 days ± 8.88) immediately following the surgery. Whether octreotide was administered or not was based on the individual surgeons' propensity for octreotide, which was believed to have changed over time. Therefore, the number of patients in the octreotide group increased with time, with 71.6% of the group seen in the last half of the study.
Pancreaticoduodenectomies were performed according to the classic Whipple procedure or via a pylorus-preserving method. All pancreaticojejunostomies were carried out with either the end-to-end or end-to-side telescoping (invagination/double layer) method. A short silicon stent was routinely intubated into the remaining pancreatic duct, depending on the duct's diameter. The tip of the tube was placed 1.0 - 1.5 cm into the jejunum. Also, two closed-suction drains were inserted through the separated site and placed in the vicinity of the pancreaticojejunostomy in order to prevent direct contact with the anastomotic site.
Statistical analysis was made using SPSS 11.0 for Windows. To compare the incidence of pancreatic fistula in the two groups, Chi-square statistics, Fisher's exact test, and the Student's t-test were used. A p-value of less than 0.05 was considered significant. Multivariate comparison was made using a logistic regression of the variables that were originally used in the univariate analysis.
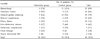
Among the 190 patients who underwent a pancreaticoduodenectomy, 60 patients (31.6%) had one or more complications (32.1% in the octreotide group and 31.2% in the control group). The most common complication was hemorrhage (8.9% overall, 7.4% in the octreotide group, and 10.1% in the control group), followed by pancreatic fistula (8.4% overall, 9.9% in the octreotide group, and 7.8% in the control group), and delayed gastric emptying (7.9% overall, 6.2% in the octreotide group, and 9.2% in the control group). One patient from the octreotide group died from hemorrhage (0.5%) (Table 1).
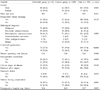
Comparing the octreotide and control groups, the differences in gender, mean age, preoperative biliary drainage, histological diagnosis, median operation time, origin of disease, incidence of complication, and incidence of pancreatic fistula were not statistically significant. On the other hand, the differences in the combined gastrectomy (p<0.001), intra-operative transfusion (p = 0.009), and duration of post-operative hospital stay (p = 0.015) were significant (Table 2). The combined gastrectomy and intra-operative transfusion were considered to be effect modifiers, rather than compounders. In the multivariate comparison for the association of pancreatic fistula with perioperative factors, the use of prophylactic octreotide (p = 0.044), cellular origin of the disease (p = 0.049), and combined gastrectomy (p = 0.018) were selected as the independent variables (Table 3).
Our data showed that the use of octreotide to prevent pancreatic fistula after a pancreaticoduodenectomy is ineffective. Since this study was not a prospective randomized trial, we failed to determine a clear indication for the administration of octreotide, other than simply a change in the surgeons' propensity. However, we recommend discontinuing routine use of octreotide a pancreaticoduodenectomy, based on our results. Although several prospective randomized studies6,10,12-15 and meta-analyses16-18,20 have investigated the effect of octreotide after a pancreatectomy, no clear conclusion can be made since the results of these studies were contradictory. This may be attributed to the variations in the definition of pancreatic fistula, patient characteristics, dosages of octreotide, perioperative treatment modalities, and surgical procedures. Thus, an international consensus on the definition of pancreatic fistula after a pancreaticoduodenectomy should be reached prior to the routine prophylactic use of octreotide for pancreatic fistula.
Pancreatic fistula is defined according to the concentration of amylase in the drainage fluid, volume of drainage, and clinical manifestation. In 1992, Buchler et al.10 defined it as a concentration of amylase in the drainage fluid three times more than the serum concentration, and a drainage volume of more than 10 mL during a 24 hour period. Patients were injected subcutaneously with 100 µg of octreotide every eight hours for seven days. In 1994, Pederzoli et al.12 defined pancreatic fistula as the presence of drainage fluid exceeding 10 ml per 24 hours for at least four days, starting from the fourth day after the operation, and an amylase content of at least three times more than the maximum normal value. In 1997, Lowy et al.14 defined it as the clinical pancreatic anastomotic leak (2.5 times more than the upper limit of the normal serum amylase) in association with a fever (over 38℃), leukocytosis (a white blood cell count over 10,000/L), sepsis (homodynamic instability requiring treatment in the intensive care unit), or a need of percutaneous drainage of the amylase-rich fluid collection. They also defined it as a biochemical pancreatic anastomotic leak with an elevated level of amylase (more than 2.5 times higher than the upper limit of normal serum amylase) in the drainage fluid or three days after surgery, even if it was asymptomatic and resolved spontaneously. Such patients were treated subcutaneously with 150 µg of octreotide every eight hours for five days. In 2000, Yeo et al.15 defined pancreatic fistula as a drainage of greater than 50 mL of amylase-rich fluid (three-fold more than the normal upper limit in the serum) per day by surgically placed drains or ten days after surgery, or pancreatic anastomotic disruption demonstrated by a radiograph. Such patients were treated subcutaneously with 250 µg of octreotide every eight hours for seven days, until the fistula resolved. We defined pancreatic fistula as more than 500 U/mL of amylase-rich fluid from the surgical drain three days after surgery. Such patients were treated with 100 µg of octreotide subcutaneously every 12 hours.
Without proper adjustment to the various definitions of pancreatic fistula, as well as variation in the dosage of octreotide among the reported studies, it is difficult to reach a conclusion on the use of octreotide treatment based on the practice of evidence-based-medicine. Until there is a consensus on the definition of pancreatic fistula and the proper dosage of octreotide is established by new prospective randomized studies, the results obtained by an individual institution should be considered only as a sample applicable to their own conditions.
In our study, the incidence of pancreatic fistula was influenced independently by the cellular origin of the disease and combined gastrectomy (Table 3). In most studies, the personal technical skill of the surgeons and the hardness of the residual pancreas have been reported to be important factors in the occurrence of complications after a pancreaticoduodenectomy.1-2,21-27 In some studies, patients who underwent a pancreaticoduodenectomy were classified into high-risk and low-risk groups,10,12,14 which were dependent on the hardness of the remaining pancreas and the amount of pancreatic secretion. In our study, the cellular origin of the disease was considered to be a main factor in determining the feasibility of a pancreaticojejunostomy. We observed that the incidence of pancreatic fistula in the pylorus preserving pancreaticoduodenectomy was lower than in the conventional pancreaticoduodenectomy (Table 3). Even though the mechanism is unclear, this could be attributed to the unknown function of the remaining duodenum, preserved pylorus, or gastric antrum in contributing to healing after a pancreaticojejunostomy. The remaining stomach and the lesser omentum may alternately protect the anterior pancreaticojejunostomy site.
In our study, the incidence of pancreatic fistula was not different between the control and octreotide groups. However, in the patients treated with octreotide, the pylorus preserving pancreaticoduodenectomy was the most favorable prognosis factor. This suggests that the prophylactic use of octreotide was not a favorable prognosis factor. We recommend the selective prophylactic use of octreotide in high-risk patients with a soft pancreas and a small pancreatic duct (under 3 mm). In addition, the indication of octreotide for prophylaxis of a pancreatic fistula should be adjusted by individual institutions based on their mortality and morbidity rates.
References
1. Trede M, Schwall G. The complications of pancreatectomy. Ann Surg. 1988. 207:39–47.
2. Yeo CJ. Management of complications following pancreaticoduodenectomy. Surg Clin North Am. 1995. 75:913–924.
3. Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992. 127:945–949. discussion 949-50.
4. Brodsky JT, Turnbull AD. Arterial hemorrhage after pancreatoduodenectomy. The 'sentinel bleed'. Arch Surg. 1991. 126:1037–1040.
5. Rumstadt B, Schwab M, Korth P, Samman M, Trede M. Hemorrhage after pancreatoduodenectomy. Ann Surg. 1998. 227:236–241.
6. Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995. 222:580–588. discussion 588-92.
7. Chou FF, Sheen-Chen SM, Chen YS, Chen MC, Chen CL. Postoperative morbidity and mortality of pancreaticoduodenectomy for periampullary cancer. Eur J Surg. 1996. 162:477–481.
8. Tran K, Van Eijck C, Di Carlo V, Hop WC, Zerbi A, Balzano G, et al. Occlusion of the pancreatic duct versus pancreaticojejunostomy: a prospective randomized trial. Ann Surg. 2002. 236:422–428.
9. Marcus SG, Cohen H, Ranson JH. Optimal management of the pancreatic remnant after pancreaticoduodenectomy. Ann Surg. 1995. 221:635–648.
10. Buchler M, Friess H, Klempa I, Hermanek P, Sulkowski U, Becker H, et al. Role of octreotide in the prevention of postoperative complications following pancreatic resection. Am J Surg. 1992. 163:125–131.
11. Friess H, Beger HG, Sulkowski U, Becker H, Hofbauer B, Dennler HJ, et al. Randomized controlled multicentre study of the prevention of complications by octreotide in patients undergoing surgery for chronic pancreatitis. Br J Surg. 1995. 82:1270–1273.
12. Pederzoli P, Bassi C, Falconi M, Camboni MG. Efficacy of octreotide in the prevention of complications of elective pancreatic surgery. Italian Study Group. Br J Surg. 1994. 81:265–269.
13. Montorsi M, Zago M, Mosca F, Capussotti L, Zotti E, Ribotta G, et al. Efficacy of octreotide in the prevention of pancreatic fistula after elective pancreatic resections: a prospective, controlled, randomized clinical trial. Surgery. 1995. 117:26–31.
14. Lowy AM, Lee JE, Pisters PW, Davidson BS, Fenoglio CJ, Stanford P, et al. Prospective, randomized trial of octreotide to prevent pancreatic fistula after pancreaticoduodenectomy for malignant disease. Ann Surg. 1997. 226:632–641.
15. Yeo CJ, Cameron JL, Lillemoe KD, Sauter PK, Coleman J, Sohn TA, et al. Does prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreaticoduodenectomy? Results of a prospective randomized placebo-controlled trial. Ann Surg. 2000. 232:419–429.
16. Rosenberg L, MacNeil P, Turcotte L. Economic evaluation of the use of octreotide for prevention of complications following pancreatic resection. J Gastrointest Surg. 1999. 3:225–232.
17. Stojadinovic A, Brooks A, Hoos A, Jaques DP, Conlon KC, Brennan MF. An evidence-based approach to the surgical management of resectable pancreatic adenocarcinoma. J Am Coll Surg. 2003. 196:954–964.
18. Li-Ling J, Irving M. Somatostatin and octreotide in the prevention of postoperative pancreatic complications and the treatment of enterocutaneous pancreatic fistulas: a systematic review of randomized controlled trials. Br J Surg. 2001. 88:190–199.
19. Kohler E, Beglinger C, Dettwiler S, Whitehouse I, Gyr K. Effect of a new somatostatin analogue on pancreatic function in healthy volunteers. Pancreas. 1986. 1:154–159.
20. Berberat PO, Friess H, Uhl W, Buchler MW. The role of octreotide in the prevention of complications following pancreatic resection. Digestion. 1999. 60:Suppl 2. 15–22.
21. Bottger TC, Junginger T. Factors influencing morbidity and mortality after pancreaticoduodenectomy: critical analysis of 221 resections. World J Surg. 1999. 23:164–172.
22. Berberat PO, Friess H, Kleeff J, Uhl W, Buchler MW. Prevention and treatment of complications in pancreatic cancer surgery. Dig Surg. 1999. 16:327–336.
23. Shyr YM, Su CH, Wu CW, Lui WY. Does drainage fluid amylase reflect pancreatic leakage after pancreaticoduodenectomy? World J Surg. 2003. 27:606–610.
24. Hashimoto N, Ohyanagi H. Pancreatic juice output and amylase level in the drainage fluid after pancreatoduodenectomy in relation to leakage. Hepatogastroenterology. 2002. 49:553–555.
25. Fujino Y, Suzuki Y, Ajiki T, Tanioka Y, Ku Y, Kuroda Y. Risk factors influencing pancreatic leakage and the mortality after pancreaticoduodenectomy in a medium-volume hospital. Hepatogastroenterology. 2002. 49:1124–1129.
26. Howard JM. Pancreatojejunostomy: leakage is a preventable complication of the Whipple resection. J Am Coll Surg. 1997. 184:454–457.
27. Hamanaka Y, Nishihara K, Hamasaki T, Kawabata A, Yamamoto S, Tsurumi M, et al. Pancreatic juice output after pancreatoduodenectomy in relation to pancreatic consistency, duct size, and leakage. Surgery. 1996. 119:281–287.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download