This article has been retracted. See "Retraction: Paper “Comparison of Effect of Treatment with Etidronate and Alendronate on Lumbar Bone Mineral Density in Elderly Women with Osteoporosis” by Iwamoto J, et al. [Yonsei Med J 2005;46(6):750-758]" in Volume 60 on page 117.
Abstract
The purpose of this open-labeled prospective study was to compare the treatment effects of cyclical etidronate and alendronate on the lumbar bone mineral density (BMD), bone resorption, and back pain in elderly women with osteoporosis. Fifty postmenopausal women with osteoporosis, age ranging from 55 to 86 years (mean: 70.7 years), were randomly divided into two groups with 25 patients in each group: the cyclical etidronate group (etidronate 200 mg daily for 2 weeks every 3 months) and the alendronate group (5 mg daily). The BMD of the lumbar spine (L1-L4) measured by DXA, the urinary cross-linked N-terminal telopeptides of type I collagen (NTX) level measured by the enzyme-linked immunosorbent assay, and back pain evaluated by the face scale score were assessed at baseline, 6 months, and 12 months. There were no significant differences in baseline characteristics including age, body mass index, years since menopause, lumbar BMD, urinary NTX level, and face scale score between the two treatment groups. Etidronate treatment sustained the lumbar BMD following a reduction in the urinary NTX level and improved back pain, while alendronate treatment reduced the urinary NTX level more significantly, resulting in an increase in the lumbar BMD, and similarly improved back pain. No serious adverse events were observed in either group. This study confirmed that alendronate treatment had a greater efficacy than etidronate treatment in increasing the lumbar BMD through the reduction of bone resorption in elderly women with osteoporosis.
Osteoporosis is a common health problem in elderly women. Hormone replacement therapy is the treatment of choice for the prevention of bone loss in early postmenopausal women, while bisphosphonates are useful agents that increase bone mineral density (BMD) and subsequently prevent osteoporotic fractures in elderly women. Bisphosphonates such as etidronate and alendronate are widely used for osteoporosis treatment in Japan. The efficacy of treatment with cyclical etidronate (200 mg daily for 2 weeks every 3 months) or alendronate (5 mg daily) in increasing BMD and reducing the incidence of osteoporotic fractures in Japanese patients with osteoporosis has been clearly demonstrated.1-3 Both agents are generally accepted as safe, effective, and well-tolerated treatments in elderly women with osteoporosis.
These bisphosphonates inhibit osteoclast-mediated bone resorption, and loss of osteoclast function and apoptosis is the consequence of loss of function of one or more important signaling proteins. Etidronate can be metabolically incorporated into nonhydrolyzable analogs of ATP, and intracellular accumulation of these metabolites inhibits osteoclast function.4 A nitrogen-containing bisphosphonate like alendronate is not metabolized but can inhibit enzymes of the mevalonate pathway, thereby preventing the biosynthesis of isoprenoid compounds that are essential for the post-translational modification of small GTPases.4 Thus, the mechanism for the inhibition of bone resorption and the subsequent degree of anti-resorptive effects may differ between etidronate and alendronate.
A meta-analysis study analyzed randomized controlled trials that reported the efficacy of treatment with etidronate or alendronate for osteoporosis, and it suggested that alendronate had a greater effect on osteoporosis than etidronate.5 Etidronate and alendronate have also been reported to relieve or prevent back pain in patients with osteoporosis.3,6 Some elderly patients with disabilities and/or back pain can not take alendronate precisely because of its unique method of taking the medicine. Therefore, it is important to know how efficacious etidronate treatment is in elderly women with osteoporosis, in comparison with alendronate treatment. The relative effectiveness can be determined only by a head-to-head comparison in the same population. However, a direct comparison of the efficacy of treatment with alendronate and etidronate in Japanese patients with osteoporosis in a single study has not yet been reported. The purpose of this open-labeled prospective study was to compare the effects of etidronate and alendronate on lumbar BMD, bone resorption, and back pain in elderly women with osteoporosis.
Fifty postmenopausal women, 55-86 years of age, were recruited at our hospital between July 2002 and July 2003. All of them were diagnosed as having osteoporosis according to the Japanese criteria.7,8 According to the Japanese criteria for osteoporosis in women, patients whose BMD was < 70% of the young adult mean (YAM) or 70-80% of the YAM with a history of osteoporotic fractures were diagnosed as having osteoporosis. They were divided one by one in the order of recruiting into two groups with 25 patients in each group: the cyclical etidronate (200 mg daily for 2 weeks every 3 months) group and the alendronate (5 mg/daily) group. These doses are primary used in Japanese elderly women with osteoporosis because they are recognized as being effective doses.1-3 The duration of treatment was 12 months. Preliminary screening included medical history, physical examination, plain X-ray examination of the thoracic and lumbar spine, lumbar BMD measurement, blood and urine biochemical tests, and a questionnaire to evaluate back pain. The participants who had a past history of reflux esophagitis, gastric or duodenal ulcer, or gastrectomy were excluded. The lumbar BMD was measured, and the assessment of vertebral fractures on plain X-ray films was performed as described below. The serum calcium, phosphorus, and alkaline phosphatase (ALP) levels were measured by using standard laboratory techniques. The urinary cross-linked N-terminal telopeptides of type I collagen (NTX) level was measured by using the enzyme-linked immunosorbent assay. The assessment of the face scale score was performed as described below. None of the subjects suffered from any metabolic bone disease, and none had a history of hormone (estrogen) replacement therapy or had ever taken medication that affects bone metabolism prior to the present study. All subjects were instructed to take 800 mg of calcium daily in their food intake during the study. Informed consent was obtained from each participant. Table 1 illustrates the baseline characteristics of the study subjects. After the start of the treatment, the lumbar BMD, biochemical markers, and back pain were assessed every 6 months, and plain X-rays of the thoracic and lumbar spine were assessed at the end of 12 months of treatment. The primary endpoints of this study were the lumbar BMD, urinary NTX level, and back pain. This protocol was approved by the ethical committee of our hospital.
The BMD of the lumbar spine (L1-L4) in the antero-posterior view was measured by dual energy X-ray absorptiometry (DXA) using a Hologic QDR 1500W instrument (Bedford, MA, USA). The coefficient of variation (100×standard deviation/mean) of five measurements with repositioning within 72 hours each time was less than 1.2% in three persons.
Plain lateral X-ray films of the thoracic and lumbar spine were obtained to find evidence of vertebral fractures. A vertebral fracture was defined according to vertebral height obtained from lateral X-ray films based on the Japanese criteria.7,8 Briefly, the vertebral height was measured at the anterior (A), central (C), and posterior (P) parts of the vertebral body, and the presence of the vertebral fracture was confirmed when (1) more than a 20% reduction of vertebral height (A, C, and P) compared with the neighboring vertebrae was observed; (2) C/A or C/P was less than 0.8; or (3) A/P was less than 0.75. The assessment of vertebral fractures was performed in the T4-L4 spine.
Back pain was evaluated quantitatively by assessing the mood of patients according to the face scale. The face scale contains ten drawings of a single face, which is arranged in serial order by rows, with each face depicting a slightly different mood. Subtle changes in the eyes, eyebrows, and mouth are used to represent slightly different levels of mood. They are arranged in decreasing order of mood and numbered from 1 to 10, with 1 representing the most positive mood and 10 representing the most negative mood. As the examiner pointed to the faces, the following instructions were given to each patient: "The faces below go from no pain at the top to severe pain at the bottom. Point to the face that best shows your current level of back pain." Thus, facial expression was used as an indicator of back pain. The validity and reliability of the face scale have been demonstrated,9 although pain is a subjective symptom that is relatively difficult to evaluate.
Data were expressed as the mean ± standard deviation (SD) in tables and as the mean ± standard error (SE) in figures. Data were compared between the two groups by using the unpaired t-test. The significance of longitudinal changes in the lumbar BMD, face scale score, and serum ALP and urinary NTX levels and their longitudinal percent changes was determined by using the one-way analysis of variance (ANOVA) with repeated measurements. Furthermore, longitudinal percent changes in these parameters were compared between the two groups by using the two-way ANOVA with repeated measurements. All statistical analyses were performed using the Stat View-J5.0 program on a Macintosh computer. A significance level of p<0.05 was used for all comparisons.
Table 2 shows the longitudinal changes in the lumbar BMD, face scale score, and biochemical markers, and Table 3 and Fig. 1 show the longitudinal percent changes in the lumbar BMD, face scale score, and serum ALP and urinary NTX levels. The one-way ANOVA with repeated measurements illustrated that the lumbar BMD was sustained in the etidronate group (2.7% non-significant increase) and was increased in the alendronate group (9.3% significant increase), and also, it illustrated that the serum ALP and urinary NTX levels and face scale score decreased in both groups with no significant changes in the serum calcium and phosphorus levels. In particular, the mean reduction in the urinary NTX level at months 6 and 12 was 13.2% and 38.8%, respectively in the etidronate group and 47.0% and 49.9%, respectively in the alendronate group. The two-way ANOVA with repeated measurements illustrated that longitudinal percent changes in the lumbar BMD and urinary NTX level significantly differed between the two groups.
At the end of 12 months, a plain X-ray examination of the thoracic and lumbar spine revealed no evidence of new thoracic or lumbar vertebral fractures in any patient of either group. During the 12 months of treatment, non-vertebral osteoporotic fractures also did not occur in the hip, wrist, or shoulder of any patient.
No serious adverse events, such as gastrointestinal tract adverse symptoms caused by reflux esophagitis or gastric ulcer were observed in any of the patients. However, minor adverse effects were observed; thirst, itchy eruption, gastric pain, and diarrhea were transiently experienced in one patient in the alendronate group, and itchy eruption and gastric pain were transiently experienced in one and two patients, respectively in the etidronate group. Because these minor adverse events were mild and improved within a couple of weeks, all patients who experienced these side effects were able to continue taking the medicine.
This study showed that etidronate treatment sustained the lumbar BMD (2.7% non-significant increase) following a reduction in the urinary NTX level, while alendronate treatment reduced the urinary NTX level and increased the lumbar BMD (9.3% increase). Alendronate treatment had a greater efficacy than etidronate treatment in increasing the lumbar BMD in elderly women with osteoporosis. The percentage increase in the lumbar BMD after one year of etidronate treatment (200 mg daily for 2 weeks every 3 months) was reported to be 2.4% in Japanese patients with involutional osteoporosis.3 Our non-significant increase in the lumbar BMD might simply be due to the small sample size.
This difference in the efficacy for the lumbar BMD may be attributable to these drugs' effect on bone resorption because the reduction was greater in the alendronate group (47.0% at month 6 and 49.9% at month 12) than in the etidronate group (13.2% and 38.8%, respectively). Urinary NTX has been demonstrated to predict an increase in the lumbar BMD in response to alendronate treatment in late postmenopausal women with osteoporosis. Also, a highly significant correlation has been demonstrated between the percent decrease in the urinary NTX level at 3 or 6 months and the percent increase in the lumbar BMD after 2 years of alendronate treatment.10,11 It has also been confirmed that a daily dose of 10 mg was more effective than one of 5 mg in suppressing bone resorption and increasing the lumbar BMD in patients with osteoporosis.12 These results suggest that when bone resorption is more strongly suppressed, especially in the early period in osteoporosis treatment, there is a greater increase in BMD, which supports our results.
The average age of the participants in this study was very old. Thus, it was important to compare the efficacies of etidronate and alendronate with those of active vitamin D and calcium supplementation. However, this study lacked the active vitamin D and calcium group. In Japan, alfacalcidol (active vitamin D) had been often used in the treatment of osteoporosis before bisphosphonates, such as etidronate and alendronate were available. Orimo et al.13 reported that alfacalcidol treatment that was performed for one year under calcium supplementation (300 mg/day) sustained the lumbar BMD (only 0.65% increase from the baseline) and reduced the incidence of new vertebral fractures (75/1000 patient years for alfacalcidol group vs. 277/1000 patient years for placebo group) in Japanese postmenopausal women with osteoporosis (mean age, 71.9 years). Etidronate and alendronate treatments seem to be more efficacious than alfacalcidol treatment in increasing the lumbar BMD and preventing new vertebral fractures in Japanese elderly women with osteoporosis.
The femoral neck as well as the spine is a clinically important site in the treatment of osteoporosis. Therefore, not only should the lumbar BMD have been assessed but the femoral neck BMD should have been also. Patients should assume the supine position with the knee and hip joints flexed at 90° during the lumbar BMD measurement and with the knee and hip joints extended during the femoral neck BMD measurement. In patients with round back and/or osteoarthritis of the knee, who were unable to assume the proper position especially during the femoral neck BMD measurement, the measurement was not assessed precisely. Thus, the femoral neck BMD could not be assessed in this study.
Spinal osteoporosis causes back pain, possibly resulting in disabilities in elderly women. The relief of back pain by intervention is important in the elderly to improve their activity of daily living. Since back pain that is associated with spinal osteoporosis may be linked to increased bone resorption, drugs affecting bone metabolism such as bisphosphonates, which are anti-resorptive agents, may be useful for pain control in elderly women with osteoporosis. In this study, both treatments with either etidronate or alendronate reduced back pain in elderly women with osteoporosis.
Nevitt et al.6 have reported that long-term alendronate treatment is associated with significantly lower risk of patients having days of bed rest and limited activity due to back pain in elderly osteoporotic women, which suggests that alendronate treatment in elderly osteoporotic patients is efficacious in reducing the burden of limitation of activity and restriction to bed caused by back pain. According to the results, alendronate treatment may have the potential not only to prevent but also to reduce back pain that is associated with spinal osteoporosis.
Several reports have demonstrated the effects of bisphosphonates on bone pain in patients with bone resorption-related diseases. Short-term treatment with alendronate improved pain, disability, and standing and walking capacities in patients with avascular necrosis of the hip, due to the inhibition of the resorptive action of mature osteoclasts, an increase in apoptosis of osteoclasts, and probably a decrease in apoptosis of osteoblasts and osteocytes.14 Intravenous pamidronate seems to be a valuable treatment for back pain, as well as in rehabilitating elderly patients who are suffering from chronic and refractory back pain caused by osteoporotic vertebral fractures,15 and also reduces skeletal pain and biochemical markers of bone resorption in patients with skeletal metastases.16-18 Furthermore, risedronate decreases bone pain in patients with Paget's disease of bone.19 These results support our view that anti-resorptive agents such as bisphosphonates may have the potential to relieve back pain that is probably associated with osteoporosis partly through the suppression of bone resorption.
However, despite the smaller reduction in the urinary NTX level, etidronate treatment, nevertheless, did improve back pain, similar to alendronate treatment. Thus, other mechanisms might be involved in the reduction of back (bone) pain through etidronate treatment in this study. Available evidence suggests that etidronate treatment decreases pain by suppressing the production of interleukin (IL)-6, IL-12, and prostaglandin E2.20,21 Although etidronate treatment was reported to transiently reduce metastatic cancer bone pain in patients with painful bone metastases from primary cancer sites, a possible explanation for this relief of metastatic cancer bone pain achieved by etidronate treatment is speculated to be the combined effects of the suppression of bone resorption and a reduction in the production of interleukins and prostaglandins.17 It is speculated that etidronate might partially reduce back pain by reducing the production of prostaglandins and cytokines,22 which might be produced by microfractures resulting from increased bone resorption in the trabeculae of the spine.
In this study, the increase in the lumbar BMD and the reduction in the urinary NTX levels were greater in the alendronate group than in the etidronate group. It was also reported that without any significant change in the serum 1,25-dihydroxyvitamin D3 levels as compared with active control (alfacalcidol) in patients with osteoporosis, bisphosphonates such as alendronate decreased serum osteocalcin levels and increased the serum PTH levels from the baseline.1 Thus, comparisons of other serum chemistry markers such as osteocalcin, parathyroid hormone (PTH), 25-hydroxyvitmain D3, and 1,25-dihydroxyvitmain D3 would also be of interest. Further studies are needed to clarify the differences in these serum chemistry markers between the etidronate and alendronate treatments.
There were not cases of drop-out through the trial due to side effects, personal excuse or noncompliance in our 50 subjects. Although some side effects were observed in both groups, they were mild, and did not result in a single drop-out. This high compliance might mainly de to the fact (1) that we adequately explained the reason why bisphosphonate treatment was needed based on the results of thoracic and lumbar spine radiographs and BMD and bone turnover marker measurements; (2) that we encouraged participants to continue the trial even though some side effects were observed, if they were tolerable; and (3) we excluded the participants who had the past history of reflux esophagitis, gastric or duodenal ulcer, or gastrectomy. Thus, the results of this study may be applicable only to patients without a past history of problems in the esophagus, stomach, or duodenum.
There were some notable limitations to the study. First, this study was not a double-blind trial but an open-labeled one. Therefore, some results might possibly be biased. Second, the number of the study subjects was relatively small and was not large enough to highlight the results. Third, because pain is a subjective symptom, there was difficulty in evaluating back pain using the face scale score. Moreover, the change in the face scale score should have been compared between the bisphosphonate groups and the placebo group to verify the effect of bisphosphonates on back pain. Information on limited activities of daily living due to back pain other than the face scale score can be helpful in evaluating the pain relief effect of bisphosphonates. Double-blind randomized placebo-controlled studies that are conducted on a sufficient number of subjects are needed to confirm the results of this study.
In conclusion, this study showed that in elderly women with osteoporosis, etidronate treatment sustained the lumbar BMD following a reduction in the urinary NTX level and improved back pain, while alendronate treatment reduced the urinary NTX level more significantly, resulting in an increase in the lumbar BMD, and similarly improved back pain. The greater efficacy of alendronate treatment compared to etidronate treatment in increasing the lumbar BMD by reducing bone resorption was confirmed by a head-to-head comparison in Japanese elderly women with osteoporosis.
Figures and Tables
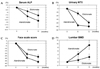 | Fig. 1Percent changes in lumbar BMD, face scale score, and biochemical markers. Data are expressed as mean ± SE. One-way analysis of variance (ANOVA) with repeated measurements was used to determine significance of longitudinal percent change in parameters. BMD, bone mineral density; ALP, alkaline phosphatase; NTX, cross-linked N-terminal telopeptides of type I collagen. |
Table 2
Changes in Lumbar BMD, Face Scale Score, and Biochemical Markers

Data are expressed as mean ± SD.
One-way analysis of variance (ANOVA) with repeated measurements was used to determine significance of longitudinal change in parameters. Two-way ANOVA with repeated measurements was used to compare longitudinal changes in parameters between two groups.
BMD, bone mineral density; ALP, alkaline phosphatase; NTX, cross-linked N-terminal telopeptides of type I collagen.
References
1. Shiraki M, Kushida K, Fukunaga M, Kishimoto H, Taga M, Nakamura T, et al. A double-masked multicenter comparative study between alendronate and alfacalcidol in Japanese patients with osteoporosis. Osteoporos Int. 1999. 10:183–192.
2. Kushida K, Shiraki M, Nakamura T, Kishimoto H, Morii H, Yamamoto K, et al. The efficacy of alendronate in reducing the risk for vertebral fracture in Japanese patients with osteoporosis: a randomized, double-blind, active-controlled, double-dummy trial. Current Therapeutic Research. 2002. 63(9):606–620.
3. Fujita T, Orimo H, Inoue T, Kaneda K, Sakurai M, Morita R, et al. Double-blind multicenter comparative study with alfacalcidol of etidronate disodium (EHDP) in involutional osteoporosis (in Japanese). Clin Eval. 1993. 21:261–302.
4. Rogers MJ, Frith JC, Luckman SP, Coxon FR, Benford HL, Monkkonen J, et al. Molecular mechanism of action of bisphosphonate. Bone. 1999. 24:5 Suppl. 73S–79S.
5. Cranny A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C. Meta-analyses of therapies for postmenopausal osteoporosis. IX Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev. 2002. 23:570–578.
6. Nevitt MC, Thompson DE, Black DM, Rubin SR, Ensrud K, Yates AJ, et al. Effect of alendronate on limited-activity days and bed-disability days caused by back pain in postmenopausal women with existing vertebral fractures. Arch Intern Med. 2000. 160:77–85.
7. Orimo H, Sugioka Y, Fukunaga M, Muto Y, Hotokebuchi T, Gorai I, et al. Diagnostic criteria of primary osteoporosis. J Bone Miner Metab. 1998. 16:139–150.
8. Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, et al. Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab. 2001. 19:331–337.
9. Lorish CD, Maisiak R. The face scale: a brief, nonverbal method for assessing patient mood. Arthritis Rheum. 1986. 29:906–909.
10. Garnero P, Shih WJ, Gineyts E, Karpf DB, Delmas PD. Comparison of new biochemical markers of bone turnover in late postmenopausal osteoporotic women in response to alendronate treatment. J Clin Endocrinol Metab. 1994. 79:1693–1700.
11. Greenspan SL, Parker RA, Ferguson L, Rosen NH, Maitland-Ramsey L, Karpf DB. Early changes in biochemical markers of bone turnover predict the long-term response to alendronate therapy in representative elderly women: a randomized clinical trial. J Bone Miner Res. 1998. 13:1431–1438.
12. Tonino RP, Meunier PJ, Emkey R, Rodriguez-Portales JA, Menkes CJ, Wasnich RD, et al. Skeletal benefits of alendronate: 7-year treatment of postmenopausal osteoporotic women. Phase III Osteoporosis Treatment Study Group. J Clin Endocrinol Metab. 2000. 85:3109–3115.
13. Orimo H, Shiraki M, Hayashi Y, Hoshino T, Onaya T, Mayazaki S, et al. Effects of 1α-hydroxyvitamin D3 on lumbar bone mineral density and vertebral fractures in patients with osteoporosis. Calcif Tissue Int. 1994. 54:370–376.
14. Agarwala S, Sule A, Pai BU, Joshi VR. Alendronate in the treatment of avascular necrosis of the hip. Rheumatology (Oxford). 2002. 41:346–347.
15. Gangji V, Appelboom T. Analgesic effect of intravenous pamidronate on chronic back pain due to osteoporotic vertebral fractures. Clin Rheumatol. 1999. 18:266–267.
16. Glover D, Lipton A, Keller A, Miller AA, Browing S, Fram RJ, et al. Intravenous pamidronate disodium treatment of bone metastases in patients with breast cancer. A dose-seeking study. Cancer. 1994. 74:2949–2955.
17. Iwamoto J, Takeda T, Ichimura S. Transient relief of metastatic cancer bone pain by oral administration of etidronate. J Bone Miner Metab. 2002. 20:228–234.
18. Hortobagyi GN, Terhiault RL, Porter L, Blayney D, Lipton A, Sinoff C, et al. Efficacy of pamidronate in reducing skeletal complications in patients with breast cancer and lytic bone metastases. N Engl J Med. 1996. 335:1785–1791.
19. Siris E, Chines AA, Altman RD, Brown JP, Johnston CC Jr, Lang R, et al. Risedronate in the treatment of Paget's disease of bone: an open label, multicenter study. J Bone Miner Res. 1998. 13:1032–1038.
20. Nishikaku F, Nakayama T, Nakatsuka M. Analgesic property of bisphosphonate, etidronate in animal models. Jpn Pharmacol Ther. 1998. 26:457–463. (in Japanese).
21. Tanaka T, Nakayama T, Katsumata T. Etidronate, therapeutic agent for osteoporosis possessing analgesic effect. Bio Clinica. 2001. 16:57–61. (in Japanese).
22. Pappagallo M, Breuer B, Schneider A, Sperber K. Treatment of chronic mechanical spinal pain with intravenous pamidronate: a review of medical records. J Pain Symptom Manage. 2003. 26:678–683.





