Abstract
Descemet's membrane detachment (DMD) is an uncommon condition with a wide range of etiologies. More than likely, the most common cause is a localized detachment occurring after cataract surgery. We report three cases of Descemet's membrane detachment that occurred after uncomplicated phacoemulsification cataract surgeries. The first patient was managed without surgical intervention, the second patient was treated using an intracameral air injection, and the last patient was treated with an intracameral perfluoropropane (C3F8) gas injection. All three patients recovered their vision following the reattachment of Descemet's membrane. The three patients were treated according to the extent of the detachment.
Descemet's membrane detachment (DMD) is an uncommon but serious complication of intraocular surgery. It was first reported in 1928 by Samuels, and since then it has been reported most often after cataract surgery. DMD has also been known to occur after other various ophthalmic procedures including: cyclodialysis, iridectomy, trabeculectomy, holmium laser sclerostomy, penetrating keratoplasty, full-thickness lamellar keratoplasty, pars plana vitrectomy and viscocanalostomy.1
The natural history of DMD has long been an area of controversy, and the appropriate timing for intervention remains unclear. Most DMDs remain small and localized to the wound, but some cases present with large, extensive detachments that result in severe corneal edema and a marked reduction in visual acuity. Traditional treatment regimens have included: observation, intracameral injections of air or viscoelastic, transcorneal suturing, and even corneal transplantation. During the past few years, intracameral injections with sulfur hexafluoride (SF6) or perfluoropropane (C3F8) gas have gained increasing acceptance as an efficient and effective treatment option for DMD.2
We report three cases of DMD that occurred after uncomplicated cataract surgery and describe their management and visual outcome.
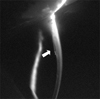
A 73-year-old man underwent uncomplicated phacoemulsification cataract surgery of his right eye under topical anesthesia with temporal corneal incision. He had no past ocular disease or trauma history. He had a medical history of diabetes and mild bronchial asthma. The patient was also taking oral medication for diabetes, but he was not taking any medication for bronchial asthma. His preoperative corrected vision was 20/40, and his intraocular pressure was 17 mmHg. On postoperative day one, his corrected visual acuity was 20/200, and his intraocular pressure was 16 mmHg. The patient's cornea was edematous with Descemet's folds. The anterior chamber was deep with cells 4+. He was instructed to use ofloxacin eye drops and 0.12% prednisolone eye drops every two hours for one week, and then four times a day thereafter. The cornea was still edematous when he visited our clinic one week later. Three weeks after surgery, his visual acuity was 20/100 and his intraocular pressure was 19 mmHg. The patient complained of a foreign body sensation and visual disturbances. The corneal edema had improved but the slit lamp exam revealed DMD at the superonasal area (Fig. 1). There was no direct trauma to the superonasal cornea during the surgery. Because the size of the DMD was small and the location was peripheral, we decided to observe the patient for a follow-up period without surgical intervention. Postoperative use of ofloxacin eye drops and 0.12% prednisolone eye drops was maintained four times a day. During the follow-up period, an intracameral air injection was not needed because the size of the DMD decreased and the patient's vision improved. Two months after the surgery, the DMD had completely reattached and the patient's corrected visual acuity had improved to 20/30. Ofloxacin eye drops and 0.12% prednisolone drops were maintained for two more weeks. Three months later, the cornea was clear, and his corrected vision was 20/20.
A 61-year-old woman underwent uncomplicated phacoemulsification cataract surgery of her left eye under topical anesthesia with temporal corneal incision. She underwent a successful cataract surgery of her right eye three months earlier in our clinic using the same method. The patient had no past medical history, and no history of any ocular trauma. Her preoperative corrected vision was 20/50 and her intraocular pressure was 12 mmHg. One day after surgery, her uncorrected visual acuity was 20/30 and her intraocular pressure was 14 mmHg. Ofloxacin eye drops and 0.12% prednisolone eye drops were prescribed for use postoperatively every two hours, as in the first patient. Two days after surgery, the patient's uncorrected visual acuity was 20/20 and the intraocular pressure was 12 mmHg, but the cornea was slightly edematous and a subendothelial opacity was observed in the center of the cornea. A tear in the Descemet's membrane was observed in the temporal area. The anterior chamber was deep with cells 1 to 2+. Five days after surgery, her visual acuity decreased to 20/25 and the temporal cornea was edematous with a large DMD (Fig. 2A). The patient complained of blurred vision and mild irritation of her left eye. The postoperative medications of ofloxacin eye drops and 0.12% prednisolone eye drops were maintained every two hours. On the next day, the patient underwent an intracameral air injection in the operating room (Fig. 2B). The patient was instructed to maintain a supine position. One day after the air injection, her uncorrected visual acuity was 20/40 and her intraocular pressure was 19 mmHg. The corneal edema had decreased significantly. The Descemet's folds remained but the endothelium was successfully reattached. One week after the air injection, her uncorrected visual acuity was 20/25. Ofloxacin and 0.12% prednisolone eye drops were reduced to four times a day. She was closely followed-up for three months and by that time the cornea had cleared completely. Her corrected vision increased to 20/20. She maintained stable vision for 10 months during follow-up.
A 74-year-old woman was referred to our clinic for DMD of the left eye. She underwent uncomplicated phacoemulsification cataract surgery with a temporal corneal incision at a local eye clinic one week before referral to our clinic. She had received cataract surgery in her right eye four years earlier at another clinic. She had no remarkable medical history or ocular trauma history. She had an intracameral air injection at the local clinic four days after the surgery on her left eye due to the DMD. On examination in our clinic, her uncorrected visual acuity was counting fingers at 30 cm in her left eye, and her intraocular pressure was 17 mmHg. Slit lamp examination showed extensive DMD with only a small portion of attached endothelium in the center of the cornea (Fig. 3A). The next day, an intracameral gas injection of 14% C3F8 was performed on the left eye in the operating room. The interface fluid between the Descemet's membrane and the stroma was removed using an ab externo stab incision of the corneal stroma in mid-periphery (Fig. 3B). The patient was instructed to maintain a supine position. One day after the gas injection, her uncorrected visual acuity was counting fingers at 30 cm, and her intraocular pressure was 10 mmHg. Only a small area of detachment remained in the inferior cornea. The patient was hospitalized for close follow-up. Two days after the gas injection, her uncorrected visual acuity was 20/400, her intraocular pressure was 15 mmHg, and a small area of detachment was still visible. The postoperative medications of ofloxacin eye drops and 0.12% prednisolone eye drops were maintained every two hours. Three days after the gas injection, the detachment had resolved completely, but the intraocular pressure was elevated to 52 mmHg. The gas in the anterior chamber had increased and some gas could also be observed in the posterior chamber, resulting in an iris bombe. To reduce intraocular pressure after mannitolization, we prescribed Timolol (Timoptic XE®) eye drops once daily, atropine 1% eye drops three times daily, and oral acetazolamide 500 mg divided into four doses. Four days following the gas injection, her intraocular pressure was 7 mmHg, and the gas bubble was still visible in the anterior chamber. The Descemet's membrane remained well-attached. Eight days after the gas injection, her corrected vision was 20/30 and her intraocular pressure was 6 mmHg. Two weeks after the gas injection, the attached Descemet's membrane appeared stable and the size of the gas bubble had decreased to 25% of the vertical chamber height. One month following the procedure, the patient's corrected visual acuity remained stable at 20/30, and the intraocular pressure was 13 mmHg. The gas bubble in the anterior chamber decreased significantly, to only a small bubble in the superior portion.
In this article, we report three cases of DMD that were managed with different treatment methods. In the first case, the DMD was not located adjacent to the incision wound, while in the second patient, a typical large DMD following cataract surgery could be observed. The unusual superonasal location of the DMD in the first case leads us to suspect endothelial trauma during cataract surgery, although we do not recall touching the endothelium with surgical instruments in that area. Phacoemulsification energy also may have caused the unpredicted damage. In the second patient, any of the reported mechanisms of DMD listed below could have occurred, although we were not aware of any inadvertent event during surgery. The third patient had radial deep stromal opacities in the contralateral eye which were believed to be scars from previous DMD. Since this patient seemed to have a predisposition to Descemet's membrane separation and because the air injection performed in the other clinic was not successful, we carried out an intracameral C3F8 gas injection and a paracentesis of fluid. Both appeared to aid in the reattachment of the DMD.
DMDs are usually small and localized to the corneal wound, with minimal or no effect on corneal clarity and vision. However, larger detachments can cause severe corneal edema and visual disturbance, and they often require surgical intervention to prevent permanent corneal decomposition and a potential corneal transplant.2-4
Mackool and Holtz classified DMDs into a planar type, with the Descemet's membrane separated less than 1 mm from the corneal stroma, and a non-planar type, with a separation of greater than 1 mm. These two types can be further divided by whether the detachments are limited to the peripheral cornea, or if they involve both the peripheral and central cornea. They reported that planar detachments are more likely to resolve spontaneously, and non-planar detachments should be repaired early.5,6 The first case in our report showed planar type DMD, and the second and third cases were non-planar type DMD. Assia et al divided DMDs into detachments with or without scrolling. Detachments without scrolling are more likely to resolve spontaneously.1,5
Several mechanisms have been proposed as the possible causal mechanism for DMD: shallow chambers, complicated or repeated operations, inadvertent insertion of instruments between the corneal stroma and Descemet's membrane, anterior and shelved incisions, and the use of dull blades.5-7 Engaging the Descemet's membrane during intraocular lens implantation or with the irrigation/aspiration device (when mistaken as an anterior capsular remnant) can also lead to extensive DMD. Some have reported that inadvertent injection of viscoelastic material by inserting the cannula between Descemet's membrane and the corneal stroma may be the most common cause of Descemet's membrane detachment with the current surgical techniques.8
We understood that DMD could also be associated with the characteristics of the viscoelastic material used. We used Viscoat® in Cases 1 and 2. Cohesive viscoelastic material such as Healon® can be completely removed from the anterior chamber by aspiration. It takes a greater effort to remove dispersive substances such as Viscoat® from the anterior chamber, and complete removal is difficult to achieve. The inspiration/aspiration device may be closer to the corneal endothelium, causing the Descemet's membrane to separate from the stroma.9-11 Although this association is hardly conclusive due to the small number of cases in our experience, we believe that this is an interesting possibility that merits further investigation.
Bilateral cases of DMD have been reported during or after otherwise uneventful surgery.1 In our third case, the patient had endothelial scarring, presumed to be from old DMD in the right eye, which had undergone cataract surgery four years earlier. From this, we are led to suspect that some eyes may have a predisposition to DMD. The characteristics of patients who are at increased risk of DMD may be another topic that needs further study.
In summary, we reported three cases of DMD that received different treatments according to the severity of their conditions, and found favorable results. The time for intervention and the type of surgery used remain controversial. In addition, despite several recent reports in favor of early intracameral gas injection, it would be advisable to make intervention and treatment decisions on a case by case basis.
Figures and Tables
References
1. Marcon AS, Rapuano CJ, Jones MR, Laibson PR, Cohen EJ. Descemet's membrane detachment after cataract surgery: management and outcome. Ophthalmology. 2002. 109:2325–2330.
2. Kim T, Hasan SA. A new technique for repairing descemet's membrane detachments using intracameral gas injection. Arch Ophthalmol. 2002. 120:181–183.
3. Zeiter HJ, Zeiter JT. Descemet's membrane separation during five hundred forty-four intraocular lens implantations. 1975-1982. J Am Intraocul Implant Soc. 1983. 9:36–39.
4. Makley TA Jr, Keates RH. Detachment of Descemet's membrane with insertion of an intraocular lens. Ophthalmic Surg. 1980. 11:492–494.
5. Mackool RJ, Holtz SJ. Descemet's membrane detachment. Arch Ophthalmol. 1977. 95:459–463.
6. Iradier MT, Moreno E, Aranguez C, Cuevas J, Garcia Feijoo J, Garcia Sanchez J. Late spontaneous resolution of a massive detachment of Descemet's membrane after phacoemulsification. J Cataract Refract Surg. 2002. 28:1071–1073.
7. Anderson CJ. Gonioscopy in no-stitch cataract incisions. J Cataract Refract Surg. 1993. 19:620–621.
8. Mulhern M, Barry P, Condon P. A case of Descemet's membrane detachment during phacoemulsificaton surgery. Br J Ophthalmol. 1996. 80:185–186.
9. Maar N, Graebe A, Schild G, Stur M, Amon M. Influence of viscoelastic substances used in cataract surgery on corneal metabolism and endothelial morphology: comparison of Healon and Viscoat. J Cataract Refract Surg. 2001. 27:1756–1761.
10. Behndig A, Lundberg B. Transient corneal edema after phacoemulsification: comparison of 3 viscoelastic regimens. J Cataract Refract Surg. 2002. 28:1551–1556.
11. Kim EK, Cristol SM, Kang SJ, Edelhauser HF, Kim HL, Lee JB. Viscoelastic protection from endothelial damage by air bubbles. J Cataract Refract Surg. 2002. 28:1047–1053.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download