Abstract
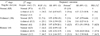
We performed this study to evaluate uterine artery Doppler velocimetry (UADV) measurement of unilateral or bilateral abnormalities as a predictor of complications in pregnancy during the mid-second trimester (20-24 weeks). We enrolled 1,090 pregnant women who had undergone UADV twice: once between the 20th and 24th week (1st stage) and again between the 28th and 32nd week (2nd stage) of pregnancy, and then delivered at Yonsei Medical Center. UADV was performed bilaterally. Follow-up UADV was performed between the 28th and 32nd week, and the frequencies of pregnancy-induced hypertension (PIH), fetal growth restriction (FGR), and preterm delivery (before 34 weeks of gestation) were determined. Chi-squared and t-tests were used where appropriate, with p < .05 considered significant. According to the results of UADV performed between 20-24 weeks of gestation, 825 women (75.7%) were included in the normal group, 196 (18.0%) in the unilateral abnormality group, and 69 (6.3%) in the bilateral abnormality group. The incidences of FGR were 8.0%, 10.2%, and 26.1%, and the incidences of PIH were 0.1%, 3.6%, and 14.5%, respectively. The incidence of PIH was significantly lower in the normal group. The incidences of preterm delivery were 2.2%, 5.6%, and 8.7%, respectively. PIH developed in 46.7% of patients with bilateral abnormal findings in both the 1st and 2nd stage tests, and developed in none of the patients with normal findings in both tests. Abnormal results found by UADV performed between the 20-24th weeks of pregnancy, such as high S/D ratios regardless of placental location and the presence of an early diastolic notch, were associated with significant increases in the incidences of intrauterine growth restriction (IUGR) and PIH. This was true for both bilateral and unilateral abnormalities. Abnormal findings in bilateral UADV during the second trimester especially warrant close follow up for the detection of subsequent development of pregnancy complications.
Preeclampsia, intrauterine growth restriction (IUGR), and preterm delivery are major causes of maternal or perinatal morbidity and mortality during the latter half of pregnancy.1,2 The exact pathophysiology underlying these conditions remains unknown. However, preeclampsia and fetal growth restriction have been reliably associated with failures in the trophoblastic invasion of spiral arteries, and Doppler studies have shown that impedance of flow in the uterine arteries is increased under these conditions.3-5 Furthermore, it has also been reported that spontaneous idiopathic preterm delivery is related to modifications associated with uterine artery Doppler velocimetry, due to impaired trophoblastic invasion of the placental bed.6 Currently, ultrasonographic Doppler velocimetry is used in the obstetric field as a noninvasive method for evaluating placental circulation, and many studies have been carried out using this technology to predict pregnancy complications.6-12 In this study, we evaluated the incidence of pregnancy complications and correlated those incidences with the unilaterality or bilaterality of abnormal findings in midtrimester uterine artery Doppler velocimetry. We also assessed the utility of follow-up Doppler velocimetry studies undertaken between the 28th and 32nd weeks of gestation. The correlation between midtrimester and third trimester Doppler studies was also assessed.
Between January 1996 and May 2002, a total of 1,090 women were enrolled in this study. They received prenatal care at the Department of Obstetrics and Gynecology, Severance Hospital, Yonsei University Medical Center, Seoul, Korea. All patients had experienced regular menstrual cycles and had precisely recorded the dates of their last menstrual periods. All subjects had twice undergone bilateral color Doppler ultrasonography of their uterine arteries, once between the 20th and 24th weeks (first stage), and once between the 28th and 32nd weeks (second stage) of gestation. Exclusion criteria included: multiple pregnancies, fetal anomalies, chromosomal abnormalities, and maternal medical illnesses such as cardiovascular disease, renal disease or diabetes mellitus. Additionally, we excluded women with known IUGR, pregnancy-induced hypertension, or clinical evidence of preterm labor before Doppler velocimetry was performed. Because of the retrospective design of this study, informed consent was not prospectively obtained from the patients who underwent uterine artery Doppler velocimetry. The hospital review board for retrospective examination on the clinical usefulness of uterine artery Doppler velocimetry approved this study.
All uterine artery waveforms were obtained using an Ultramark-9 or HDI (Advanced Technology Laboratory, Bothell, WA) attached to a 3.5-MHz curvilinear transducer, with color and pulsed Doppler abilities. We used a modification of the method described by Thaler et al.13 to measure the uterine artery Doppler waveforms.
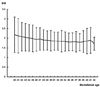
The examinations were performed on patients in a semi-recumbent position after 5 minutes of rest, and the transducers were placed in a longitudinal plane along the inguinal area. The exact locations of data collection are described in a previous report.14 The wall filter and sample gate were set at 100 MHz and 2 mm, respectively. The quality of the flow velocity waveforms was maximized by using the smallest possible angle of insonation, and accepting only those waveforms with sharp and definite outlines. After a consecutive series of 5 or more uniform waveforms had been obtained, the last waveform image was frozen and analysis was performed. The S/D ratio was measured at peak systolic and end-diastolic flows. The diastolic notch was defined as the slower velocity just after systolic flow, but before maximum diastolic flow. Abnormal S/D levels were set at a minimum of 2 standard deviations above the mean normal values of uterine Doppler waveforms in each gestational week previously obtained at our institute (Fig. 1). High S/D ratios in either the right or left Doppler waveform or an early diastolic notch were considered abnormal results. The results of the Doppler measurements were not taken into consideration for obstetric management. The outcomes of the pregnancies were evaluated by review of the hospital records after delivery. The evaluation variables were: the presence of IUGR (< 10th percentile on the fetal growth curve at our institute), delivery before 34 weeks' gestation, and preeclampsia. Preeclampsia was defined as a blood pressure in excess of 140/90 mmHg, as measured on two occasions 6 hours apart, with proteinuria of 1+ measured with a dipstick in 2 samples obtained 6 hours apart, or > 300 mg in a 24-hour urine collection.15 Statistics were analyzed with the Statistical Analysis System (SAS, version 6.07; SAS Institute, Inc, Cary, NC, USA). Chi-squared and t-tests were used where appropriate and p < .05 was considered statistically significant.
A total of 1,090 unselected women with singleton pregnancies were enrolled in this study. Median age at delivery was 31.2 (range 18-42) years. This was considered a low-risk population with 104 (9.5%) patients exhibiting fetal growth restriction, 18 (1.7%) exhibiting preeclampsia, and 35 (3.2%) delivering prior to 34 weeks' gestation. The incidence of preeclampsia, IUGR, and delivery before 34 weeks' gestation was significantly higher in those with unilateral or bilateral abnormalities of uterine artery Doppler velocimetry revealed during the 20-24 weeks (first stage) of gestation, than did those with normal values. Within the abnormal group, the incidence was higher in those with bilateral abnormalities than unilateral abnormalities. (Table 1) Similar results were obtained with Doppler velocimetries performed between 28-32 weeks (second stage). The incidence of preeclampsia was 48% in those with bilateral abnormal Doppler velocimetry (Table 1). Of those with normal Doppler results in the first stage, 97.1% showed normal values in the second stage studies. In the second stage studies, persistent abnormal findings were revealed in those with unilateral abnormalities (37.6%) and those with bilateral abnormalities (17.8%). The incidence of pregnancy complications was not determined to be significantly higher among those with abnormal first stage results and normal second stage results. However, the incidence of complications was significantly higher among those with abnormal first stage results and persistent unilateral or bilateral abnormalities in second stage studies Of those who exhibited bilateral Doppler abnormalities in the first stage, 21.7% showed persistent bilateral abnormalities in the second stage. In the persistently abnormal group, 46.7% had IUGR, 33.3% delivered prior to the 34th week of gestation, and 46.7% exhibited preeclampsia (Table 2). The relative risks of each pregnancy complication, according to the results of first and second stage uterine artery Doppler velocimetry, are presented in Table 2. Generally, persistent abnormal findings in the Doppler measurements were associated with higher relative risks of each pregnancy complication, with the exception of the risk for delivery before 34 weeks' gestation, which was not significantly correlated in subjects with unilateral abnormalities in second stage studies. The indices of diagnostic performance of first stage uterine artery Doppler velocimetry are shown in Table 3.
A high S/D ratio or the persistence of an early diastolic notch reflects increased peripheral vascular resistance. In a previous study, we suggested that an assessment of the uterine artery S/D ratio, coupled with an evaluation for an early diastolic notch, would be a clinically useful test for fetal well-being.14 Because vascular resistance varies with placental location, our institute had previously used the mean value of the bilateral S/D ratios to report the effects of placental location on the presence of early diastolic notches.16 Placental location is one of the key factors determining the velocity waveform. The uterine artery proximal to the placenta shows lower resistance than does the non-placental uterine artery. This phenomenon has been attributed to the fact that the placental uterine artery perfuses the subplacental myometrium, and therefore reflects placental perfusion, whereas the non-placental uterine artery mainly perfuses the non-placental myometrium, and thus may exhibit increased peripheral resistance. This asymmetry in uteroplacental circulation is primarily explained by a significant increase in the S/D ratio values of the nonplacental uterine artery. However, the placenta usually receives its blood supply from both uterine arteries to differing degrees. In this study, the clinical utility of both unilateral and bilateral abnormalities of uterine artery Doppler waveforms was assessed (disregarding placental location) as a predictor of poor pregnancy outcomes among a low-risk population. Uterine artery Doppler waveforms were defined as any S/D ratio 2 or more standard deviations above the mean value previously obtained at our institute, or the presence of an early diastolic notch. Furthermore, we also attempted to ascertain whether the sensitivity and positive predictive values of conventional Doppler velocimetry could be improved through this test.
We found that those patients with unilateral abnormalities, regardless of the study time, developed pregnancy complications at significantly higher frequencies than those without abnormalities, and that this tendency was even more pronounced in second stage studies. This indicates that even though an abnormal Doppler waveform velocity exists on only one side, the persistence of this unilateral abnormality indicates a greater risk of pregnancy complications. It can also be assumed that if a persistent abnormality occurs on the side in which the placental bed is located, a poor pregnancy outcome is especially likely. Of patients with first stage bilateral abnormalities, 37.6% also had abnormal second stage Doppler results. This group had a significantly higher risk of IUGR, PIH and delivery prior to the 34th week of gestation, as compared to those who persistently showed normal study results.
We also assessed the diagnostic performance of second stage uterine artery Doppler velocimetry (performed during the 28th-32nd weeks) for predicting poor pregnancy outcomes. First, with respect to the relationship between the two tests, 97.1% of those with normal first stage results also showed normal second stage results with no elevated incidence of pregnancy complications. The negative predictive value of first stage Doppler velocimetry was very high (92-99.9%) and correlates well with previously reported values.14-17 This indicates that, in such cases, intensive prenatal surveillance is largely unnecessary, and can safely be avoided. On the other hand, its relatively low sensitivity and positive predictive values regarding IUGR and delivery prior to the 34th week of gestation (sensitivities: 36.5% and 48.6%, PPV: 14.3% and 6.4%) preclude its usage as a screening test. Diagnostic performance improved, however, when second stage studies were performed on the abnormal first stage group. The coupling of the two tests resulted in higher sensitivities (50.0%, 70.6%) and PPV (31.7%, 20.0%) (data not presented). This finding suggests that serially performed uterine artery Doppler velocimetry is effective in detecting high-risk groups, thus improving pregnancy outcomes in this group via intensive prenatal surveillance. Several previous studies reported the utility of uterine artery Doppler velocimetry performed after midtrimester in predicting preterm delivery. Our study also showed that the relative risk was higher in the abnormal group than in the normal group. However, considering several important contributing factors, such as PIH, this result was not statistically significant. In this study, the sensitivity of first stage uterine artery Doppler studies for PIH was 94.4%. This high value is probably due to the generally low prevalence of PIH in the low-risk population, and the broad criteria for abnormal Doppler studies, such as the inclusion of one-sided abnormalities without regard to placental location, or the presence of an early diastolic notch. A low PPV limits its usefulness as a screening test, but PPV incidence increased to 25% when follow-up studies were performed on the initially abnormal group (data not shown).
In conclusion, abnormal results of uterine artery Doppler velocimetry performed during the 20th-24th week of gestation, such as high S/D ratios regardless of placental location or the presence of an early diastolic notch, are significantly correlated with the incidence of both IUGR and PIH. This is the case with respect to both bilateral and unilateral abnormalities. Therefore, as mentioned previously, unnecessary prenatal surveillance can safely be eschewed in patients with bilaterally normal Doppler studies. In the case of those patients with unilateral abnormal findings, follow-up Doppler studies are recommended. If abnormalities persist, these patients should be considered high-risk and monitored closely throughout the remaining pregnancy. In the future, further research should focus on combining uterine artery Doppler velocimetry with other studies that can be performed during the 1st trimester to predict trophoblastic dysfunction and placental insufficiency. If this can be accomplished, the positive predictive value of this test will be greatly enhanced.
Figures and Tables
Fig. 1
Mean and 2 standard deviations above the mean, calculated at our institute, of uterine Doppler wave forms in each gestational week.
References
1. Committee on Practice Bulletins--Gynecology, American College of Obstetricians and Gynecologists, Washington, DC 20090-6920, USA. Intrauterine growth restriction. Clinical management guidelines for obstetrician-gynecologists. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2001. 72:85–96.
2. Gladstone IM, Katz VL. The morbidity of the 34- to 35-week gestation: should we reexamine the paradigm? Am J Perinatol. 2004. 21:9–13.
3. Meekins JW, Pijnenborg R, Hanssens M, McFayden IR, van Assche A. A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol. 1994. 101:669–674.
4. Browne JC, Veall N. The maternal placental blood flow in normotensive and hypertensive women. J Obstet Gynecol Br Emp. 1953. 60:141–147.
5. Campbell S, Diaz-Recasens J, Griffin DR, Cohen-Overbeek TE, Pearce JM, Wilson K, et al. New Doppler technique for assessing uteroplacental blood flow. Lancet. 1983. 1:675–677.
6. Strigini FA, Lencioni G, De Luca G, Lombardo M, Bianchi F, Genazzani AR. Uterine artery velocimetry and spontaneous preterm delivery. Obstet Gynecol. 1995. 85:374–377.
7. Albaiges G, Missfelder-Lobos H, Lees C, Parra M, Nicolaides KH. One-stage screening for pregnancy complications by color Doppler assessment of the uterine arteries at 23 weeks' gestation. Obstet Gynecol. 2000. 96:559–564.
8. Phupong V, Dejthevaporn T, Tanawattanacharoen S, Manotaya S, Tannirandorn Y, Charoenvidhya D. Predicting the risk of preeclampsia and small for gestational age infants by uterine artery Doppler in low-risk women. Arch Gynecol Obstet. 2003. 268:158–161.
9. Benedetto C, Valensise H, Marozio L, Giarola M, Massobrio M, Romanini C. A two-stage screening test for pregnancy-induced hypertension and preeclampsia. Obstet Gynecol. 1998. 92:1005–1011.
10. Campbell S, Pearce JM, Hackett G, Cohen-Overbeek T, Hernandez C. Qualitative assessment of uteroplacental blood flow: early screening test for high-risk pregnancies. Obstet Gynecol. 1986. 68:649–653.
11. Jacobson SL, Imhof R, Manning N, Mannion V, Little D, Rey E, et al. The value of Doppler assessment of the uteroplacental circulation in predicting preeclampsia or intrauterine growth retardation. Am J Obstet Gynecol. 1990. 162:110–114.
12. Chung JE, Cho JS, Han SS, Park YW, Kim JW. Uterine artery Doppler velocimetry in the prediction of adverse obstetric outcomes in unexplained MSAFP elevations. Yonsei Med J. 2000. 41:17–21.
13. Thaler I, Weiner Z, Itskovitz J. Systolic or diastolic notch in uterine artery blood flow velocity waveforms in hypertensive pregnant patients: relationship to outcome. Obstet Gynecol. 1992. 80:277–282.
14. Park YW, Cho JS, Kim HS, Kim JS, Song CH. The clinical implications of early diastolic notch in third trimester Doppler wave form analysis of the uterine artery. J Ultrasound Med. 1996. 15:47–51.
15. Davey DA, MacGillivray I. The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol. 1988. 158:892–898.
16. Park YW, Cho JS, Han SS, Kim JW. Clinical significance of early diastolic notch of uterine artery Doppler velocimetry in relation to placental location. Korean J Obstet Gynecol. 1999. 42:2486–2491.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download