Abstract
We have determined the infusion rates of rocuronium in the elderly and young adult patients during sevoflurane and nitrous oxide anesthesia. The correlation of some anthropometric predictors with infusion rate of rocuronium was also investigated for both elderly and young adult. Participating patients were assigned to one of two groups: 1) young adult patients aged 20 to 50 years (n = 30); 2) elderly patients aged over 65 years (n = 30). The anthropometric variables such as height, weight, ratio of weight to body surface area, subscapularis and suprailiac skin folds, body surface area, body mass index and % ideal body weight were evaluated as predictors for infusion rate. The infusion rate in elderly patients was significantly less compared with that in young adult patients (p < 0.05). In elderly patients, no anthropometric predictor was related to the infusion rate of rocuronium. This suggests that the infusion rate of rocuronium for an elderly patient needs to be individualized by monitoring neuromuscular transmission to avoid excessive dose.
The infusion rate of a drug is based frequently on body weight. There is a progressive decline in lean body mass and, particularly, in muscle with aging, and blood volume and extracellular fluid also diminish with age. Hence, the central volume of distribution for highly polar compounds should be smaller, and the dosage based on body weight will result in a higher initial plasma concentrations than for the young adult.1 The decreased total body water and liver mass, which normally accompany aging, are likely explanations for the prolonged duration of action for the neuromuscular blockade compounds in the elderly.2,3 Various pharmacokinetic factors may also be involved in the delivery of a drug.
Rocuronium bromide is structural analogue (2-morpholino, 3-hydroxy, 16N-allylpyrrolidino derivative) of vecuronium with a neuromuscular blocking potency 6-7 times less that of vecuronium. This lack of potency is thought to be an important factor in determining the rapid onset of neuromuscular block.4,5 Rocuronium is a nondepolarizing muscle relaxant with an intermediate duration of action and insignificant accumulation, and it is well suited for continuous infusion.6-8 Rocuronium is eliminated primarily by the liver and to a slight degree by the kidneys. Because rocuronium does not have active metabolites,9 it may be a better choice than vecuronium for prolonged infusion.
The infusion rate of rocuronium for an adequate surgical operation was suggested to be 6.1 ± 2.0 µg/kg/min10 and 8.4 ± 1.6 µg/kg/min8 for adult and pediatric patients, respectively, during sevoflurane anesthesia, while there has been no report yet on the optional dosage for elderly patients.
The aim of this study was to determine the infusion rate of rocuronium necessary to maintain a stable and suitable level of neuromuscular blockade for surgery in young adults and the elderly patients. We also evaluated different anthropometric variables such as body weight, ratio of weight to body surface area (BSA), sum of subscapularis and suprailiac skin folds, body mass index (BMI) and percentage of ideal body weight (%IBW) as indices for the optimization of rocuronium administration to each individual patient.
After obtaining approval from the Local Ethics Committee and written informed consent, 60 patients (ASA physical status I or II) who were scheduled for elective orthopedic surgery under general anesthesia were assigned into two groups: 1) young adult patients aged 20 to 50 years (control group, n = 30); 2) elderly patients aged over 65 years (elderly group, n = 30). Exclusion criteria were body weight more or less than 20% of the ideal body weight, expected difficult intubation, pre-existing hepatic, renal and neuromuscular disease, allergic diathesis, pregnancy or breast-feeding and preoperative medication known to interact with non-depolarizing neuromuscular blocking agents.
Anthropometric variables such as height, weight, and subscapularis and suprailiac skin folds were measured before the induction of anesthesia. BSA was estimated using the formula of Du Bois and Du Bois11 (0.007184×height [cm]0.725×weight [kg]0.425) and BMI calculated as total body weight divided by the squared height.12 Calculation of the ideal body weight (IBW) was based on the formula of Devine13,14 {50 kg + 2.3×(height [inch]-60) for man and 45.5 kg + 2.3×(height [inch]-60) for woman}.
Patients were premedicated with glycopyrrolate 0.2 mg and midazolam 2.0 mg that was given intramuscularly 30 min before surgery. Each patient was given a standard general anesthetic consisting of fentanyl, thiopental sodium, 50% nitrous oxide and 3% sevoflurane in oxygen. The neuromuscular blockade was monitored using an accelerograph TOF-Watch® (Organon, Teknica B.V., Boxtel, the Netherlands). The patient's arm used for neuromuscular monitoring was fixed to an arm board. The ulnar nerve was stimulated transcutaneously at the wrist via reference electrodes. After calibration, supramaximal stimuli of 0.2 ms duration in a single twitch mode at 1 Hz were used until the end of the study. The software that the computer used to record the responses was TOF-Watch®. Another anesthesiologist behind a screen, who positively could not see the patient, observed only the TOF-Watch® and then he or she adjusted the infusion rate of rocuronium. Non-invasive blood pressure was measured on an arm, and the arm was not used for the evaluation of neuromuscular transmission. Fluids were given via an intravenous cannula inserted proximal to the area of nerve stimulation.
An ED95 dosage (0.3 mg/kg) of rocuronium was administered via a forearm vein and then tracheal intubation was performed when the maximal depression of the twitch response was reached. When the height of the single twitch recovered up to 15% of the control twitch recorded before induction of the neuromuscular block, the continuous infusion of rocuronium was initiated. The continuous infusion rate was determined when the single twitch response was maintained at 10 ± 5% for more than 10 minutes and forty minutes after 1.5-2.0% sevoflurane was reached.10 Mechanical ventilation was adjusted to maintain the end-tidal carbon dioxide partial pressure between 30 and 35 mmHg. Body temperature was monitored continuously in the upper esophagus and at the thenar eminence of the same arm used for neuromuscular monitoring. Core temperature and skin temperature were maintained at greater than 36.0℃ and 32.0℃, respectively.
Data were expressed as means ± standard deviation. The anthropometric variables and infusion rates of the two groups were compared by t-test and a p-value < 0.05 was considered statistically significant. The linear regression analysis was used to test the relations between the anthropometric variables and the infusion rate. To determine the correlation, individual values of each anthropometric parameter were also plotted against the infusion rate provided. Data were analyzed using SPSS for Windows software (SPSS 11.0, Chicago, IL, USA).
There were no significant differences between the young adult and the elderly patients for the anthropometric variables like height, weight, BSA, BMI, %IBW, ratio of body weight to BSA and the sum of subscapularis and suprailiac skin folds. The infusion rate of rocuronium (2.9 ± 1.0 µg/kg/min) in elderly patients was significantly less than that of young adults (4.2 ± 1.6 µg/kg/min) (p < 0.05, Table 1).
The infusion rate of rocuronium in young adults correlated with the sum of subscapularis and suprailiac skin folds (r2 = 0.23, p = 0.007, Fig. 1). However, the elderly did not show any correlation with the anthropometric variables.
The present study demonstrated that the infusion rate of rocuronium in the elderly under sevoflurane anesthesia was about 69% less compared to that in the young adults.
This is consistent with earlier findings for vecuronium in other study. The vecuronium infusion rate was 70% less in the elderly than that in the young adults.15 The most reasonable explanation for the decrease of the infusion rate in the elderly would be a decrease in drug elimination capacity noted with aging. In addition, pharmacokinetic changes in the elderly such as reduction in the total body water and liver mass may result in a prolonged effect of rocuronium.3,16
The continuous infusion of a neuromuscular blocking agent stabilizes the blood concentration of the drug maintains the degree of neuromuscular relaxation constant.17 When the infusion dosage is adjusted to the appropriate individualized demand for each patient, it is possible to avoid excessive neuromuscular relaxation by reducing the total drug requirement. A more rapid recovery from the neuromuscular relaxation by using a proper antagonist within a short time after the infusion termination is a decided advantage.18 However, neuromuscular monitoring is a necessity because interindividual differences do exist.19 Infusion rates based on weight may provide a relatively excessive dosage to the elderly because of their pharmacokinetic differences. If other anthropometric besides body weight can predict infusion rate, they can be clinically useful indices.
As for the initial infusion rate, the infusion rate of rocuronium in elderly patients should be reduced since the infusion rate needed to produce adequate surgical relaxation in the elderly was significantly less than that used in the young adult. The infusion rate in the elderly must be individualized for the special requirement of each patient, and this means starting at a lower infusion rate for the elderly.
It has been suggested in several studies that the volatile anesthetics elicit strengthening of the neuromuscular relaxation.8,10,17,20-22 In particular, when compared with the intravenous anesthetic, propofol, the use of a volatile anesthetic decreases the infusion rate of rocuronium by 40%.10 The infusion rate of rocuronium in this study was lower than those reported in the previous studies4,7,8,17,21,22 presumably due to the neuromuscular blocking effect of sevoflurane. Although the exact mechanism of neuromuscular relaxation by a volatile anesthetic has not been elucidated, an interaction between a volatile anesthetic and a neuromuscular blocking agent is known to enhance the inhibition of the muscular contraction and to move a neuromuscular blocking agent dosage-response curve to the left (the decrease of ED50, ED95).17
In young adults, the sum of subscapularis and suprailiac skin folds is the best predictor for the infusion rate of rocuronium. Therefore, the infusion rate of rocuronium should logically be based on the sum of subscapularis and suprailiac skin folds. Using the sum of subscapularis and suprailiac skin folds to determine the infusion rate is a safe method even in the obese patients because the prolongation of the muscle relaxant effect is avoided since an overdose is prevented.23 The elderly did not show any correlation with standard anthropometric variables.
The skin fold measurement predicts the body density and is used to calculate the body mass percentage. The skin folds can be measured at several regions such as thigh, abdomen, triceps, biceps, chest, subscapularis and suprailiac regions. Among these, only the subscapularis and suprailiac skin folds were measured in our study because it was not necessary to measure the skin folds on several regions, since a significant result was obtained from previous studies for vecuronium by applying the sum of subscapularis and suprailiac skin folds.24
The continuous infusion rate of rocuronium based on the 10% twitch height with accelerography under sevoflurane anesthesia for the elderly over 65 years old was 2.9 ± 1.0 µg/kg/min. Unlike young adults, there were no significant anthropometric predictors to determine the infusion rate of rocuronium in the elderly. From these results it was concluded that the infusion rate of rocuronium in the elderly should be reduced and an adequate infusion rate has to be individualized by the use of a neuromuscular monitor.
Figures and Tables
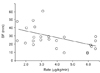 | Fig. 1Sum of subscapular skin folds and suprailiac skin folds plotted against the infusion rate of rocuronium for the young patients group. The infusion rate of rocuronium for young adults correlated with the sum of subscapularis and suprailiac skin folds (linear regression: SF = 44.64 + [-0.47] (rate, r2 = 0.23, p = 0.007). SF, sum of subscapular skin folds and suprailiac skin folds. |
Table 1
Characteristics of Patients, Anthropometric Variables and Infusion Rate

Note, Values are as means ± SD or number.
*p < 0.05 when compared with young patients
Young, > 20 year-old and < 50 year-old patients; Elderly, > 65 year-old patients.
BSA, body surface area; BMI, body mass index; %IBW, body weight in percent of ideal body weight; Sub SF, subscapularis skin fold; Si SF, suprailiac skin fold.
References
1. Kopman AF. McLesky CH, editor. Effects of muscle relaxants and reversal agents. Geriatric anesthesiology. 1997. Baltimore: Williams & Wilkins;299–309.
2. Matteo RS, Ornstein E, Schwart AE, Ostapkovich N, Stone JG. Pharmacokinetics and pharmacodynamics of rocuronium (Org 9426) in elderly surgical patients. Anesth Analg. 1993. 77:1193–1197.
3. Bevan DR, Fiset P, Balendran P, Law-Min JC, Ratcliffe A, Donati F. Pharmacodynamic behaviour of rocuronium in the elderly. Can J Anaesth. 1993. 40:127–132.
4. Sparr HJ, Khuenl-Brady KS, Erickson LI. Pharmacodynamics and pharmacokinetics of rocuronium following continuous infusion in patients during intravenous anaesthesia. Eur J Anaesthesiol Suppl. 1994. 9:63–65.
5. Hunter JM. Rocuronium: The newest aminosteroid neuromuscular blocking drug. Br J Anaesth. 1996. 76:481–483.
6. McCoy EP, Mirakhur RK, Maddineni VR, Wierda JM, Proost JH. Pharmacokinetics of rocuronium after bolus and continuous infusion during halothane anaesthesia. Br J Anaesth. 1996. 76:29–33.
7. McCoy EP, Mirakhur RK, Maddineni VR, Loan PB, Connolly F. Administration of rocuronium (Org 9426) by continuous infusion and its reversability with anticholinesterases. Anaesthesia. 1994. 49:940–945.
8. Woloszczuk-Gebicka B, Lapcznski T, Wierzejski W. The influence of halothane, isoflurane and sevoflurane on rocuronium infusion in children. Acta Anaesthesiol Scand. 2001. 45:73–77.
9. Wierda JM, Kleef UW, Lambalk LM, Kloppenburg WD, Agoston S. The pharmacodynamics and pharmacokinetics of Org 9426, a new non-depolarizing neuromuscular blocking agent, in patients anaesthetized with nitrous oxide, halothane and fentanyl. Can J Anaesth. 1991. 38:430–435.
10. Bock M, Klippel K, Nitsche B, Bach A, Martin E, Motsch J. Rocuronium potency and recovery characteristics during steady-state desflurane, sevoflurane, isoflurane or propofol anaesthesia. Br J Anaesth. 2000. 84:43–47.
11. Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. Nutrition. 1989. 5:303–311.
12. Matz R. Calculating body mass index. Ann Intern Med. 1993. 118:232.
13. Pai MP, Paloucek FP. The origin of the "ideal" body weight equations. Ann Pharmacother. 2000. 34:1066–1069.
14. Devine BJ. Gentamicin therapy. Drug Intell Clin Pharm. 1974. 8:650–655.
15. Rupp SM, Castagnoli KP, Fisher DM, Miller RD. Pancuronium and vecuronium pharmacokinetics and pharmacodynamics in younger and elderly adults. Anesthesiology. 1987. 67:45–49.
16. De Almeida MC, Latorre F, Gervais HW, Kleeman PP. The effects of age on onset and recovery from atracurium, rocuronium and vecuronium blockade. Anaesthesist. 1996. 45:903–906.
17. Shanks CA. Pharmacokinetics of the nondepolarizing neuromuscular relaxants applied to calculation of bolus and infusion dosage regimens. Anesthesiology. 1986. 64:72–86.
18. Martineau RJ, St-Jean B, Kitts JB, Curran MC, Lindsay P, Hull KA, et al. Cumulation and reversal with prolonged infusions of atracurium and vecuronium. Can J Anaesth. 1992. 39:670–676.
19. Wulf H, Ledowski T, Linstedt U, Proppe D, Sitzlack D. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998. 45:526–532.
20. Kansanaho M, Olkkola KT, Wierda JM. Dose-response and concentration-response relation of rocuronium infusion during propofol-nitrous oxide and isofluranenitrous oxide anaesthesia. Eur J Anaesth. 1997. 14:488–494.
21. Sutcliffe DG, Murphy CM, Maslow A, Uppington J, Shorten GD. A comparison of antagonism of rocuronium-induced neuromuscular blockade during sevoflurane and isoflurane anaesthesia. Anaesthesia. 2000. 55:960–964.
22. Shanks CA, Fragen RJ, Ling D. Continuous intravenous infusion of rocuronium (ORG 9426) in patients receiving balanced, enflurane, or isoflurane anesthesia. Anesthesiology. 1993. 78:649–651.
23. Puhringer FK, Khuenl-Brady KS, Mitterschiffthaler G. Rocuronium bromide: time-course of action in underweight, normal weight, overweight and obese patients. Eur J Anaesthesiol Suppl. 1995. 11:107–110.
24. Kirkegaard-Nielsen H, Helbo-Hansen HS, Toft P, Severinsen IK. Anthropometric variables as predictors for duration of action of vecuronium-induced neuromuscular block. Anesth Analg. 1994. 79:1003–1006.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download