Abstract
Asthma is commonly described as an atopic disease in childhood, but some cases of this disorder do not fit this description. The aim of this study was to evaluate the frequency of atopy, asthma, and sensitization to house dust mites in children with allergic symptoms. This study was performed at the Severance Hospital of Yonsei University with patients who visited the allergy clinic for evaluation of nonspecific upper respiratory symptoms, typical symptoms of asthma, or a general health workup. The patients were divided into three age groups: 0-3 years (group 1), 4-7 years (group 2), and 8-12 years (group 3). Of the 1,244 children examined, 844 (67.8%) were atopic and 400 (32.2%) were non-atopic. The frequency of atopy and asthma increased with age. Asthma was diagnosed in the same proportion (64%) of atopic and non-atopic children. As risk factors for asthma symptoms, the positive values of house dust mite (HDM) sensitivity were significantly increased in groups 1, 2, and 3 to 53.5%, 68.9%, and 80.2%, respectively. A significant difference between the percentage of asthmatics sensitized to HDM and that of asthmatics not sensitized to HDM was found only in group 3. In conclusion, asthma is related to atopy with increasing age, and house dust mite sensitization seems to be an important determinant of asthma in older children in Korea.
Go to : 
Asthma is one of the most common disorders in children. The prevalence of childhood asthma has been on the rise over the last decade.1 Although some studies noted that the prevalence of asthma has stabilized,2 the incidence is increasing in several Westernized Asian countries. Among Korean adolescents, the overall lifetime prevalence of wheeze was 12.8% in 2000 and the prevalence of asthma symptoms has increased each year from 1995 to 2000.3
Asthma is commonly recognized as an atopic disease.4 There is considerable evidence for the strong relationship between allergic sensitization and atopic disorders such as asthma, eczema, and rhinitis.5 However, the role of atopy can be overestimated, because environmental factors such as respiratory infections and exposure to allergens can cause asthma symptoms, particularly during the first year of life.6
Identification of factors that could predict the development of asthma in children is useful for early intervention, because atopic disorders usually manifest for the first time in childhood and often lead to chronic disease that may continue into adulthood.7 Studies have been carried out in different communities, and they have confirmed that sensitization to indoor allergens, especially to house dust mites (HDM), is a major risk factor for asthma.8,9 We previously reported on the correlation between specific IgE of inhalant allergens such as HDM and pulmonary function in children with asthma.10
The aim of this study was to evaluate the frequency of atopy, asthma, and sensitization to house dust mite in children who visited an allergy clinic.
Go to : 
In a cross-sectional retrospective survey lasting 26 months (November 2001-December 2003), we studied 1244 children who came to our allergy clinic in Seoul for a general health workup or with physician-referred or self-reported symptoms of atopic disease. We included in the study children for whom a diagnosis of asthma, allergic rhinoconjunctivitis, or atopic dermatitis was confirmed by a pediatric allergologist. We divided the patients into three age groups: 0-3 years (group 1), 4-7 years (group 2), and 8-12 years (group 3).
The diagnosis of asthma was made on the basis of American Thoracic Society (ATS) criteria.11
The children with asthma reported having typical wheezing or episodic shortness of breath and had a positive response to any question concerned with the following asthma-related symptoms: chest tightness, difficulty in breathing, occasional or persistent wheeze, breathlessness or cough after exposure to cold air or exercise, chest noise while breathing, chronic cough persisting for more than3 weeks, or nocturnal symptoms that disturb sleep.12 Children who could not answer any of the questions confidently were excluded from the asthma group.
Atopy was defined by one or more positive specific IgE test of eight common allergens in Korea or total serum IgE level > 100 IU/mL. Allergic rhino-conjunctivitis was diagnosed if sneezing, nasal obstruction, watery rhinorrhea, nasal itching, conjunctival hyperemia or photophobia appeared after exposure to a particular allergen and was unrelated to infection. Atopic dermatitis was defined as a pruritic, chronic or chronically relapsing dermatitis with typical features and distribution according to Hanifin and assessed with the Scorad index.13
Specific IgE test was performed on house dust mites (HDM) (Dermatophagoides pteronyssinus (Der p.), D. farinae (Der f.)), ragweed, Alternaria, egg, cow's milk, cockroach, and timothy using the CAP system FEIA (Pharmacia Diagnostics, Uppsala, Sweden). A specific IgE value greater than 0.35 kUA/L was considered positive.
All data analysis was performed using the statistical analysis program SPSS. A chi-square test was used to analyze the difference between proportions. A p-value < 0.05 was considered significant. The odds ratio (OR) was calculated to evaluate the independent effect of atopy on the development of asthma. The odds ratio was considered significant when a 95% confidence interval excluded unity.
Go to : 
In the 1244 children examined, 844 (67.8%) were atopic and 400 (32.2%) were non-atopic. Asthma was diagnosed in 542 (64%) atopic children and in 250 (64%) non-atopic children. In the overall population studied, there was no significant difference between atopic and non-atopic asthmatics.
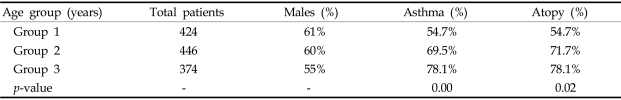
The frequencies of atopy in age groups 1, 2, and 3 were 54.7%, 72%, and 78%, respectively, and the frequencies of asthma were 54.7%, 69.5%, and 78.1%, respectively. The frequency of atopy and asthma increased with age (Table 1, p < 0.05).
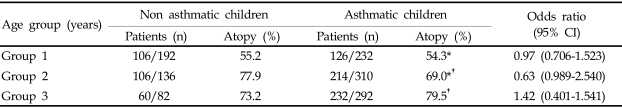
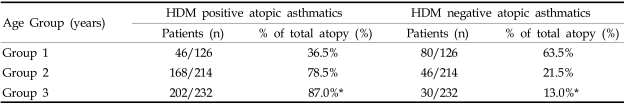
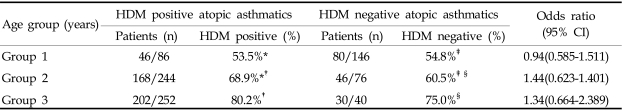
In the asthmatic children of groups 1, 2, and 3, the frequencies of atopy were 54.3% (126 of 232 asthmatic children), 69.0%, and 79.5%, respectively, and atopy increased significantly with age (group 1 vs. group 2χ2 = 12.6; group 2 vs. group 3χ2 = 8.9). However, there was no significant association between asthma and atopy in all three groups (Table 2). The percentage of asthmatic children who were HDM-positive increased significantly, especially in group 3 (group 1 vs. group 2χ2 = 6.9; group 2 vs. group 3χ2 = 8.4). As risk factors for asthma symptoms, the positive values of house dust mite (HDM) were significantly increased in age groups 1, 2, and 3 to 53.5% (46 of 86 HDM positive children), 68.9%, and 80.2%, respectively. However, a significant difference between the percentage of asthmatics sensitized to HDM and that of asthmatics not sensitized to HDM was found only in group 3 (Table 4, 87% vs. 13%χ2 = 56.3). The percentages of HDM-negative asthmatic patients was not significant between groups (Table 3; group 1 vs. group 2χ2 = .5; group 2 vs. group 3χ2 = 2.52).
Go to : 
The prevalence of atopy and asthma are increasing in all populations around the world. Higher prevalence rates are reported in more Westernized countries, with wheezing occurring in over 30% of infants in the first year of life,14 atopy in 40% of children,15 and physician-diagnosed asthma in over 20% of children. Therefore, it is important to evaluate the risk factors for asthma and the sensitization period after exposure to allergens. It is reported that the sensitization occurs early in atopic children with asthma established before 7 years of age, without any significant changes after this age.16 But atopy combines with other environmental factors to predispose children to asthma. Before the seventh year of age, the development of asthma depends mainly on factors other than atopy, such as viral respiratory illnesses.17 The majority of infants with wheezing have transient conditions such as diminished airway function at birth. Non-atopic asthmatics produce IgE directed against unknown antigens of viral origin,18 a molecular response in which IL-5 could play a key role.19 Also, in younger children, other factors like food are important in stimulation of allergic symptoms. Han et al.20 reported that, clinically, food sensitization is important in Korean infants and younger children with moderate to severe atopic dermatitis.
We evaluated infants and children who had symptoms of atopic disease to clarify the relationship between atopy and asthma. Although many reports describe a relationship between atopy and asthma, we evaluated this connection further in our country with a large data set. In Korea, the majority of adults and children with allergy are highly sensitized to Der p. and Der f. (house dust mites), and the sensitizing antigens can be causal allergens of asthma. In our study, atopy to some allergens such as HDM may be more important than atopy to other allergens in predisposing children to asthma. Early sensitization to mite allergen might lead to asthma and persistent wheeze, especially in high-risk subgroups defined by maternal atopy.21,22 Continuing exposure to mite allergens causes airway inflammation that leads to the development of asthma in childhood,23 and several studies have shown that there is a strong relationship between exposure to house dust mite allergens and the prevalence and severity of asthma.22,24-26 House dust mite allergens may be more potent than other allergens, because they are ubiquitous or because the airborne particles are small and are easily respired. Our data showed a significant correlation between atopic asthma and risk of developing HDM sensitization, especially for children over 8 years. Several cross-sectional studies in older children indicate that specific sensitization to house dust mites is related to dust mite allergen concentrations in mattress dust.27,28 Cole et al.29 investigated the relationship of dust mite allergen exposure during early life to allergic sensitivity and asthma at 6 to 7 years of age, using a relatively large birth cohort. Although HDM sensitization often occurs in early childhood and is dependent on the level of exposure,30-32 the incidence of sensitization to inhalant allergen increases with age during the first decade of life. Sporik et al.22 reported that after age 2, the children who later became allergic developed IgG, IgG4, and IgE antibodies to Der p. in parallel with the symptoms. Because the correlation between atopic asthma and HDM sensitization was not as strong in the younger age groups, we should consider other factors in younger children. Sarah et al.33 reported that aeroallergens like house dust mites play little role in the development of wheeze in the first 4 years of life. They concluded that early childhood asthma relied on other genetic and environmental factors such as maternal atopic history and smoking.
As sensitization to HDM depends on exposure to such allergens, it is important to attempt to reduce exposure before the sensitization occurs in early childhood. Lee34 reported that environmental control of house dust mites is effective in relieving symptoms and reducing peak expiratory flow rate in asthmatic children. We need longer-term follow-up studies to investigate whether the development of asthma can also be prevented by environmental control of HDM. Furthermore, asthma itself is a heterogeneous disease with many different genetic and environmental determinants, and we should consider other factors such as family history and smoking in future studies.
Go to : 
References
1. Kay AB. Advances in immunology: allergy and allergic diseases. N Engl J Med. 2001; 344:30–37. PMID: 11136958.
2. Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002; 110:315–322. PMID: 12165584.

3. Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, et al. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004; 34:1556–1562. PMID: 15479270.

4. Miraglia Del Giudice M, Pedulla M, Piacentini GL, Capristo C, Brunese FP, Decimo F, et al. Atopy and house dust mite sensitization as risk factors for asthma in children. Allergy. 2002; 57:169–172. PMID: 11929423.

5. Peat JK, Toelle BG, Gray EJ, Haby MM, Belousova E, Mellis CM, et al. Prevalence and severity of childhood asthma and allergic sensitisation in seven climatic regions of New South Wales. Med J Aust. 1995; 163:22–26. PMID: 7609683.

6. Martinez FD, Helms PJ. Types of asthma and wheezing. Eur Respir J Suppl. 1998; 27:3S–8S. PMID: 9699776.
7. Ohshima Y, Yamada A, Hiraoka M, Katamura K, Ito S, Hirao T, et al. Early sensitization to house dust mite is a major risk factor for subsequent development of bronchial asthma in Japanese infants with atopic dermatitis: results of a 4-year followup study. Ann Allergy Asthma Immunol. 2002; 89:265–270. PMID: 12269646.

8. Peat JK, Tovey E, Toelle BG, Haby MM, Gray EJ, Mahmic A, et al. House dust mite allergens a major risk factor for childhood asthma in Australia. Am J Respir Crit Care Med. 1996; 153:141–146. PMID: 8542107.

9. Platts-Mills TA, Rakes G, Heymann PW. The relevance of allergen exposure to the development of asthma in childhood. J Allergy Clin Immunol. 2000; 105(2 Pt 2):S503–S508. PMID: 10669532.

10. Choi SY, Sohn MH, Yum HY, Kwon BC, Kim KE. Correlation between inhalant allergen-specific IgE and pulmonary function in children with asthma. Pediatr Pulmonol. 2005; 39:150–155. PMID: 15633201.

11. American Thoracic Society. Medical Section of the American Lung Association. Guidelines for the evaluation of impairment/disability in patients with asthma. Am Rev Respir Dis. 1993; 147:1056–1061. PMID: 8466106.
12. Verdiani P, Di Carlos S, Baronti A. Different prevalence and degree of nonspecific bronchial hyperreactivity between seasonal and perennial rhinitis. J Allergy Clin Immunol. 1990; 86(4 Pt 1):576–582. PMID: 2229817.

13. Hanifin JM. Ellis EF, Adkinson NF, Yonginger JW, Buss WW, editors. Atopic dermatitis. Allergy. Principles and practice. 1993. St. Louis: Mosby;p. 1581.

14. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. The Group Health Medical Associates. Asthma and wheezing in the first six years of life. N Engl J Med. 1995; 332:133–138. PMID: 7800004.

15. Zhao T, Wang HJ, Chen Y, Xiao M, Duo L, Liu G, et al. Prevalence of childhood asthma, allergic rhinitis and eczema in Urumqi and Beijing. J Paediatr Child Health. 2000; 36:128–133. PMID: 10760010.

16. Kaleyias J, Papaioannou D, Manoussakis M, Syrigou E, Tapratzi P, Saxoni-Papageorgiou P. Skin-prick test findings in atopic asthmatic children: a follow-up study from childhood to puberty. Pediatr Allergy Immunol. 2002; 13:368–374. PMID: 12431197.

17. Wright AL, Taussig LM, Ray CG, Harrison HR, Holberg CJ. The Tucson Children's Respiratory Study. II. Lower respiratory tract illness in the first year of life. Am J Epidemiol. 1989; 129:1232–1246. PMID: 2729259.
18. Welliver RC, Wong DT, Sun M, Middleton E Jr, Vaughan RS, Ogra PL. The development of respiratory syncytial virus-specific IgE and the release of histamine in nasopharyngeal secretions after infection. N Engl J Med. 1981; 305:841–846. PMID: 6168908.

19. Humbert M, Menz G, Ying S, Corrigan CJ, Robinson DS, Durham SR, et al. The immunopathology of extrinsic (atopic) and intrinsic (non-atopic) asthma: more similarities than differences. Immunol Today. 1999; 20:528–533. PMID: 10529782.

20. Han DK, Kim MK, Yoo JE, Choi SY, Kwon BC, Sohn MH, et al. Food sensitization in infants and young children with atopic dermatitis. Yonsei Med J. 2004; 45:803–809. PMID: 15515189.

21. Brussee JE, Smit HA, van Strien RT, Corver K, Kerkhof M, Wijga AH, et al. Allergen exposure in infancy and the development of sensitization, wheeze, and asthma at 4 years. J Allergy Clin Immunol. 2005; 115:946–952. PMID: 15867850.

22. Sporik R, Holgate ST, Platts-Mills TA, Cogswell JJ. Exposure to house-dust mite allergen (Der p I) and the development of asthma in childhood. A prospective study. N Engl J Med. 1990; 323:502–507. PMID: 2377175.
23. Platts-Mills TA, Vervloet D, Thomas WR, Aalberse RC, Chapman MD. Indoor allergens and asthma: report of the third international workshop. J Allergy Clin Immunol. 1997; 100:S2–S24. PMID: 9438476.
24. Charpin D, Birnbaum J, Haddi E, Genard G, Lanteaume A, Toumi M, et al. Altitude and allergy to house-dust mites. A paradigm of the influence of environmental exposure on allergic sensitization. Am Rev Respir Dis. 1991; 143:983–986. PMID: 2024854.

25. Sporik R, Chapman MD, Platts-Mills TA. House dust mite exposure as a cause of asthma. Clin Exp Allergy. 1992; 22:897–906. PMID: 1464045.

26. Verhoeff AP, Van Strien RT, Van Wijnen JH, Brunekreef B. House dust mite allergen (Der p I) and respiratory symptoms in children: a case-control study. Clin Exp Allergy. 1994; 24:1061–1069. PMID: 7874605.
27. Peat JK, Tovey E, Gray EJ, Mellis CM, Woolcock AJ. Asthma severity and morbidity in a population sample of Sydney school children: Part II-Importance of house dust mite allergens. Aust N Z J Med. 1994; 24:270–276. PMID: 7980209.
28. Wickman M, Nordvall SL, Pershagen G, Sundell J, Schwartz B. House dust mite sensitization in children and residential characteristics in a temperate region. J Allergy Clin Immunol. 1991; 88:89–95. PMID: 2071788.

29. Cole Johnson C, Ownby DR, Havstad SL, Peterson EL. Family history, dust mite exposure in early childhood, and risk for pediatric atopy and asthma. J Allergy Clin Immunol. 2004; 114:105–110. PMID: 15241351.

30. Kuehr J, Frischer T, Meinert R, Barth R, Forster J, Schraub S, et al. Mite allergen exposure is a risk for the incidence of specific sensitization. J Allergy Clin Immunol. 1994; 94:44–52. PMID: 8027498.

31. Lau S, Illi S, Sommerfeld C, Niggemann B, Bergmann R, von Mutius E, et al. Multicentre Allergy Study Group. Early exposure to house-dust mite and cat allergens and development of childhood asthma: a cohort study. Lancet. 2000; 356:1392–1397. PMID: 11052581.

32. Ohshima Y, Yamada A, Hiraoka M, Katamura K, Ito S, Hirao T, et al. Early sensitization to house dust mite is a major risk factor for subsequent development of bronchial asthma in Japanese infants with atopic dermatitis: results of a 4-year followup study. Ann Allergy Asthma Immunol. 2002; 89:265–270. PMID: 12269646.

33. Polk S, Sunyer J, Munoz-Ortiz L, Barnes M, Torrent M, Figueroa C, et al. A prospective study of Fel d1 and Der p1 exposure in infancy and childhood wheezing. Am J Respir Crit Care Med. 2004; 170:273–278. PMID: 15117746.

34. Lee IS. Effect of bedding control on amount of house dust mite allergens, asthma symptom, and peak expiratory flow rate. Yonsei Med J. 2003; 44:313–322. PMID: 12728474.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download