Abstract
Behçet's disease (BD) is a chronic, relapsing, multisystem disorder, characterized by recurrent oral ulcer, genital ulcers, eye lesion, and skin lesion. The underlying pathology is nonspecificvasculitis of all vessel sizes, and severe vasculitis can result in fistula formation of neighboring tissues due to a necroticprocess. Herein, eleven cases of BD combined with fistula are presented. In the present study, various types of fistula were associated; enterocutaneous fistula in six patients, and rectovaginal fistula in two. The other three patients showed aortoduodenal fistula, urethrovaginal fistula and urethrocutaneous fistula. They were treated with a corrective operation, but the prognoses were poor due to frequent relapses.
Behçet's disease (BD) is a polymorphic and systemic disease that affects multiple organs with a variety of symptoms. It has been speculated that viral, and streptococcal infections, environmental factors, racial and familial tendency, and autoimmune mechanisms might play a role. The underlying pathology in all these lesions is nonspecific vasculitis of small and large vessels.1 Severe vasculitis induces necrosis, which can result in fistula formation between the neighboring tissues. Patients in whom medical therapy has been unsuccessful, or those who have extensive disease or complications, should be considered for surgery. In the present study, eleven patients with a fistula combined with BD, including clinical finding, treatment, and prognosis, are reviewed.
The medical records and radiological studies of the patients presenting at the Behçet's Disease Specialty Clinic of our institutions, between 1990 and 2004, and who fulfilled the criteria of both the International Study Group for Behçet's Disease2 and the revised criteria of the Behçet's Disease Research Committee of Japan,3 were retrospectively reviewed, revealing eleven patients with a combined fistula. The mean age of the patients at the time of BD diagnosis was 30.2 years, ranging from 18 to 39 years. The interval between the initial diagnosis and that of the fistula was, on an average, 4.9 years. The clinical characteristic of the BD patients with a fistula are listed in Table 1.
Total 6 patients (3 cases with enterocutaneous fistulae and 3 cases with combined enterocutnaeous and enteroenteric fistulae) were enrolled in the study. All cases developed after previous surgical manipulations with or without relation to gastrointestinal BD, and durations were variable (7 months to 2 years) between operation and fistula formation. Two cases showed no recurrence, but in 4 cases multiple recurrences were observed in both fistula types. Although mild lesions were medically observed and healed spontaneously in most conditions, there were several situations needed surgical repair thereafter.
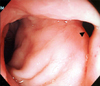
Two patients were reported with rectovaginal fistula. One developed five months after transanal endoscopic microsurgery (Fig. 1) and the other developed after hemicolectomy for obstruction. Although appropriate surgical repairs were performed in each conditions, recurrences were not controlled well.
Single case was enrolled with multiple ectopic urethral meatuses around the glans penis and penile shaft, which were healed with dressings without the need for surgical interventions (Fig. 2). The lesion had recurred several times during the last 6 years, but healed the same way each time.
In a patient an urethrovaginal fistula was observed after an ureterorenoscopy for a ureteral stone. Although multiple primary repairs were performed, but each times fistulae recurred soon thereafter. Finally complete bladder neck closure and a suprapubic cystostomy were performed.
Four years following a graft interposition of an aortic aneurysm, an aortoduodenal fistula was detected in a patient, which was thought to be a primary lesion of sudden septicemia and gastrointestinal bleeding. Re-interposition of the aortic graft and a segmental resection of the duodenum were performed, but the patient expired 48 hours postoperatively.
A fistula is an abnormal, narrow channel or tract connecting between neighboring tissues, which can develop in the presence of inflammation and infection. It may or may not be associated with an abscess, but as with an abscess, certain illnesses, such as BD and Crohn's disease, can cause fistulae to develop.4
In the present study, fistulae formations combined with BD were observed in eleven cases, including enterocutaneous, enteroenteric, rectovaginal, urethrocutaneous, urethrovaginal and aortoduodenal fistulae. Other types of fistulae have been reported in the lieterature, such as vesicovaginal,5 broncho-pulmonary arterial,6 aortoatrial,7 tracheoesophageal,8 arteriovenous9 and arterioportal fistulae.10
The exact mechanism of fistula formation in BD is unclear. In general, fistula formation is associated with poor nutrition, infection, and long term steroid use.11 In nine of our cases (case 1, 2, 3, 4, 5, 6, 8, 10, and 11), the fistulae developed after surgical processes. The fistulae were assumed to have developed due to the severe vasculitis in BD that results in an ulcer and necrosis, along with a pathergy reaction due to surgical trauma. However, the long term use of systemic corticosteroid might also have contributed to the fistulae formation.
In the present study, enterocutaneous and enteroenteric fistulae were the most common. BD is well known to often be accompanied by gastrointestinal involvement.12 The predilection sites are the terminal ileum and ileocecal area, but ulcers can develop along the entire colon. The ulcers are sometimes transmural, leading to perforations or fistula formation, or both.13 In general, an enterocutaneous fistula occurs after severe ulceration, correction operation, or even en appendectomy. Furthermore, most of these recurrent ulcers were noted at or near the anastomotic site.
A rectovaginal fistula combined with BD is very rare, with only five cases having been reported.14 Most patients included in these cases had severe vulval and anorectal ulcers.
Urinary tract involvement in BD can include glomerulonephritis, amyloidosis, cystitis, epididymitis,15 orchitis, and ulcerations affecting the scrotum, penis, vulva and vagina. Rare cases of urethrovaginal and vesicovaginal fistulae have been reported,16 but an urethrocutaneous fistula remains to be reported.
Fistulae seem to be an operative challenge for the surgeon, as they tend to be associated with significant scarring and insufficient surrounding tissues to allow for a tension-free closure. For this reason, interposition of the tissue for good vascular supply is necessary to facilitate healing. There have been case reports illustrating the advantage of interposing healthy tissue, like omentum or a dermofat graft, between the layers.16
Vascular death is most often caused by aneurysm formation and the inflammation occurring in the media and adventitia of large arterial lesions is characteristic of vasculo-BD. It has been postulated that active arteritis occurs initially, followed by destruction of the media and fibrosis in the affected arteries. An aortoenteric fistula is an uncommon, but life-threatening cause of gastrointestinal blood loss, which is often rapid, leading to death by exsanguinations.17 Our patient expired in the immediate postoperative period.
Most fistulae are corrected by operation, but anti-TNFα antibody treatment has recently challenged.18 The fistula has a tendency to recur, and reoperation of the fistula in BD seems to be the cause of the vicious cycle of frequent recurrences.
BD is accompanied by various types of fistula formation. The fistula formations in BD are closely related to the underlying vasculitis with various inflammatory cytokines as the pathogenesis of BD and the mucocutaneous hyperreactivity (Pathergy reaction) to trauma which is quite unique phenomena.
In the endemic area of BD, we must consider about the possibility of postoperative fistula formation in the BD patients and the differential diagnosis of BD when wound healing is impaired or a fistula formed after surgery.
Figures and Tables
References
1. Smith GE, Kime LR, Pitcher JL. The colitis in Behçet's diseases: a separate entity? Colonoscopic findings and literature review. Dig Dis. 1973. 18:987–1000.
2. International Study Group for Behçet's disease: Criteria for diagnosis of Behçet's disease. Lancet. 1990. 335:1078–1080.
3. Nakae K, Masaki F, Hashimoto T, Inaba G, Mochizuki M, Sakane T. Wechsler B, Godeau P, editors. Recent epidemiological features of Behçet's disease in Japan. Behçet's disease. 1993. Amsterdam: Excerpta Medica;145–151.
4. Singh B, McC Mortensen NJ, Jewell DP, George B. Perianal Crohn's disease. Br J Surg. 2004. 91:801–814.
5. Monteiro H, Nogueira R, de Carvalho H. Behçet's syndrome and vesicovaginal fistula: an unusual complication. J Urol. 1995. 153:407–408.
6. Nishi K, Myou S, Ooka T, Taitou H, Fujimura M, Matsuda T. A case of Behçet's disease presenting with Hughes-Stovin syndrome. Nihon Kyobu Shikkan Gakkai Zasshi. 1993. 31:379–384.
7. Melua A, Campbell N, McCluskey D, MacGowan SW. Aorto-atrial fistula without aneurysm formation in Behçet's disease. Heart. 1998. 80:200–201.
8. Asaoka M, Sakai Y, Kimura J, Ichihara T, Seki A, Ishii M. A case of tracheoesophageal fistula in Behçet's disease repaired with pericardial patch and gastric roll. Nippon Kyobu Geka Gakkai Zasshi. 1990. 38:1549–1553.
9. Wechsler B, Le Thi Huong Du LT, de Gennes C, Bletry O, Piette JC, Mathieu A, et al. Arterial manifestations of Behçet's disease. 12 cases. Rev Med Interne. 1989. 10:303–311.
10. Cekirge S, Gulsun M, Oto A, Dogan R, Balkanci F, Besim A. Endovascular treatment of an unusual arterioportal fistula caused by the rupture of a giant hepatic artery aneurysm into the superior mesenteric vein in Beh祴 disease. J Vasc Interv Radiol. 2000. 11:465–467.
11. Regan JP, Salky BA. Laparoscopic treatment of enteric fistulas. Surg Endosc. 2004. 18:252–254.
12. Kasahara Y, Tanaka S, Nishino M, Umemura H, Shiraha S, Kuyama T. Intestinal involvement in Behçet's disease: review of 136 surgical cases in the Japanese literature. Dis Colon Rectum. 1981. 24:103–106.
13. Lee KS, Kim SJ, Lee BC, Yoon DS, Lee WJ, Chi HS. Surgical treatment of intestinal Behçet's disease. Yonsei Med J. 1997. 38:455–460.
14. Teh LS, Green KA, O'Sullivan MM, Morris JS, Williams BD. Behçet's syndrome: severe proctitis with rectovaginal fistula formation. Ann Rheum Dis. 1989. 48:779–780.
15. Cho YH, Jung J, Lee KH, Bang D, Lee ES, Lee S. Clinical features of patients with Behçet's disease and epididymitis. J Urol. 2003. 170:1231–1233.
16. Seo IY, Park KW, Chung HJ, Rim JS. Behçet's disease with urethrovaginal fistula and stress urinary incontinence. Korean J Urol. 2001. 42:1336–1339.
17. Kobayashi M, Matsushita M, Nishikimi N, Sakurai T, Miyauchi M, Nimura Y. Aortic stump closure with a titanium permanent clamp: a useful emergency method. J Vasc Surg. 1998. 27:772–775.
18. Travis SP, Czajkowski M, McGovern DP, Watson RG, Bell AL. Treatment of intestinal Behçet's syndrome with chimeric tumour necrosis factor antibody. Gut. 2001. 49:725–728.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download