Abstract
The purpose of this volunteer study was to investigate whether pretreatment with UDCA before the administration of 99mTc DISIDA affects the biliary excretion of the DISIDA, and whether it can shorten the total imaging time. Ten young, healthy volunteers (eight males, two females, mean age: 26.3 ± 2.1 years) participated in the study. Hepatobiliary scintigraphies were performed twice per volunteer within three days, for the control and the UDCA-pretreated studies. In the control study, the gallbladder (GB) was observed first in four cases and the intestine was observed first in another four cases; in contrast, in the UDCA challenge study, the GB was observed first in eight cases. The quantitative results for the factors related to the GB differed significantly between the control and challenge studies. When the subjects were pretreated with UDCA, the time duration until visualization of the GB was shortened, and the maximum activity of the GB became more intense. In conclusion, UDCA pretreatment before hepatobiliary scintigraphy can shorten the total imaging time for evaluating functional obstructions of the cystic duct and increase the specificity of the process.
Hepatobiliary scintigraphy has been used clinically to diagnose acute cholecystitis. On a typical normal scintigraphy performed with 99mTc 2,6-diisopropyl iminodiacetic acid (DISIDA) agents, the common bile duct (CBD) and gallbladder (GB) are visualized 10-30 minutes after the intravenous administration of this radiopharmaceutical agent. However, the patients suspected of having acute cholecystitis do not show any activity of the gallbladder for up to four hours after the radiopharmaceutical administration, or within 30 minutes after the administration of morphine sulfate. These findings are interpreted as being consistent with a cystic duct obstruction, and thus suggest acute cholecystitis. In spite of the high diagnostic accuracy of hepatobiliary scintigraphy, with a sensitivity of 97% and specificity of 90%, conventional imaging protocols frequently require delayed imaging for up to four hours after injection.1 Delayed imaging is logistically inconvenient, and it may not be feasible in some clinical settings. Pharmacological interventions, including morphine augmentation and CCK pretreatment, have been used in efforts to shorten the total imaging time.2,3 Unfortunately, these pharmaceutical agents have not been widely used in the clinical setting due to the problem of applicability to the patients.
Ursodeoxycholic acid (UDCA) is the 7 betaepimer of chenodeoxycholic acid, and exerts multiple hepatoprotective activities. It modifies the bile acid pool, decreasing the levels of the endogenous hydrophobic bile acids while increasing the proportion of the nontoxic hydrophilic bile acids. It also has a choleretic effect, increasing the hepatocellular bile acid excretion, as well as having cytoprotective, antiapoptotic, and immunomodulatory properties.4-6 In clinical practice, UDCA has been used to improve cholestasis.4,7 We thought these properties of UDCA could be applied to DISIDA to cause the rapid excretion of DISIDA into the hepatic duct and the fast filling of the gallbladder with a greater amount of DISIDA per unit time.
The aim of this study was to evaluate whether pretreatment with UDCA prior to the administration of 99mTc DISIDA affects the biliary excretion of the DISIDA, and whether it has the possibility of shortening the total imaging time.
We studied 10 young, healthy volunteers (eight males, two females, mean age: 26.3 ± 2.1 years). All volunteers were studied after fasting overnight for at least eight hours to prepare the appropriate conditions for hepatobiliary scintigraphy. Hepatobiliary scintigraphies were performed twice per volunteer within three days for the control and the UDCA pretreatment studies. Nobody complained of any side effects of the UDCA pretreatment until one week after the study. The ethics committee of the university hospital approved the study, and informed consent was obtained from each subject.
Hepatobiliary scintigraphy was evaluated after the intravenous injection of 370 MBq of 99mTc DISIDA. For the control study, the volunteers did not receive any pretreatment except for the overnight fast. For the UDCA pretreatment, they orally ingested two 100 mg tablets of UDCA 15 minutes before the radiopharmaceutical injection.
A gamma camera (Millennium MG, GE, Milwaukee, Wisconsin, USA) equipped with a low-energy, high-resolution, parallel hole collimator and with a 20% window centered over the 140 KeV photopeak was used. The hepatobiliary scintigraphy was performed for 60 minutes in a dynamic mode (10 sec×60 frames, 60 sec×50 frames). The data were collected in a 128×128 matrix.
Two nuclear physicians observed the hepatobiliary scintigraphies. The time points when the gall bladder, common bile duct, and intestine were visualized for the first time, the grading of bowel activity, and the earliest organ visualized between the GB and the intestine were decided by consensus. The bowel activity in the scintigraphy was subjectively divided into 0 (no activity), 1 (mild), 2 (moderate), and 3 (intense), and the retained hepatic uptake ratio was calculated as the total hepatic uptake excepting gall bladder in the last image divided by the maximal total count of images. This ratio was used to evaluate the degree of excretory potential attributable to UDCA.
To correct the background activity, the region of interest (ROI) was drawn in the heart. Using subtraction software, the corrected maximum activities of the GB and the superior portion of the right hepatic lobe for one hour were calculated.
All data were expressed as mean ± SD. A paired t-test was used for the comparison of the two studies for each volunteer. A p<0.05 was considered statistically significant.
The results of the visual evaluation of the control and UDCA pretreatment hepatobiliary scintigraphies in the volunteers show the changes in the scintigraphic patterns. In the control study, in two cases the intestine was not observed, in four cases the GB was observed first, and in the remaining four cases, the GB was observed after the visualization of the intestine. In the UDCA challenge study, the GB was observed first in eight cases. In two cases, the GB was visualized later. Additionally, in the comparison of the time intervals, in the cases when the intestine was visualized first, the control studies took 10.3 ± 2.6 minutes, but the UDCA pretreatment shortened the intervals to 3.0 ± 1.4 minutes.
Fig. 1 is a case in which the GB was visualized later than the intestine in the control study, but was visualized first in the UDCA challenge study.
Fig. 2 shows the convergence of the observation times of the GB in the eight cases where the GB was observed first in the UDCA pretreatment hepatobiliary scintigraphies.
Comparisons of the quantitative results for several factors are shown in Table 1. Of all the factors, the factors related to the GB differed significantly between the control and challenge studies. The retained hepatic uptake ratio was also significantly lower in the UDCA pretreatment cases (p=0.001). When the UDCA pretreatment was applied, the time duration until visualization of the GB was shortened, and the maximum activity of the GB became more intense (Fig. 3).
The results of the volunteer study indicate that the UDCA accelerates the hepatocyte excretion of the 99mTc DISIDA as well as the bile into the biliary tree, and 99mTc DISIDA results in an earlier and more intense visualization of the GB in hepatobiliary scintigraphy.
As mentioned above, morphine augmentation and CCK pretreatment have been used for pharmacological interventions applied to hepatobiliary scintigraphy. However, the difficulty in accessing these pharmaceutical agents limits their clinical use. UDCA has been used in patients with cholestasis and in people with indigestion, and the dose (200 mg) of the UDCA used in this study is considered relatively low. Therefore, if UDCA pretreatment for hepatobiliary scintigraphy were to have the possibility of shortening the total study time and enhancing the diagnostic accuracy, and if UDCA were thought to be safe and to have little limitations on its use, then this protocol would be widely used. Therefore, the results of our study give important and objective information for providing a new pharmacological intervention. Recently, although the interventional protocol (repeated oral administration every 12 h for 48-72 h) of UDCA was different, there was a report that pretreatment with UDCA significantly improves the specificity of hepatobiliary scintigraphy in ruling out extrahepatic biliary atresia as a cause of prolonged neonatal jaundice.8
There are many indications for hepatobiliary scintigraphy. Practically, however, hepatobiliary scintigraphy has been mainly used to diagnose acute cholecystitis in adults and to rule out biliary atresia in neonates. Due to the characteristics of the patients examined in hepatobiliary studies, there is difficulty in investigating comparisons with other protocols in the cases of patients with suspected acute cholecystitis. In our department, we are using the method of UDCA pretreatment when performing hepatobiliary scintigraphy. This intervention helps us complete the clinical study earlier, and minimizes inconvenience for the patient.
In summary, UDCA-pretreated 99mTc DISIDA scintigraphy showed a unified tendency of the excretory pattern, in which the liver, GB, and intestine were observed sequentially. The UDCA allowed the DISIDA to enter the GB easily, and the GB was filled with a greater amount of DISIDA as compared with the control study (Table 1). Although a large-scale clinical application is needed for a precise conclusion, one dose (200 mg) of UDCA pretreatment for hepatobiliary scintigraphy is considered to increase excretion of 99mTc DISIDA from liver to GB, and to shorten the total imaging time for evaluating functional obstructions of the cystic duct. These results might improve the specificity of hepatobiliary scintigraphy in patients with suspected acute cholecystitis.
Figures and Tables
 | Fig. 1Hepatobiliary scintigraphies of a volunteer untreated with UDCA (A) and pretreated with UDCA (B). After pretreatment with UDCA, the GB (arrow) is visualized first, then the intestine. |
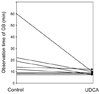 | Fig. 2Comparison of the time to visualization of the GB. The observation times of the GB converged without significant individual differences in eight cases of the UDCA pretreated hepatobiliary scintigraphies. |
 | Fig. 3Hepatobiliary scintigraphies from a volunteer with untreated UDCA (A) and pretreated UDCA (B). After pretreatment with UDCA, the maximum activity of the GB is more intense than that in the control study. |
Table 1
Comparison of the Quantitative Results of Several Factors Analyzed from the Scintigraphic Findings

Data were expressed as mean±SD, and a p<0.05 was considered statistically significant.
TGB, TCBD, and Tintestine: times until observation in the GB, CBD and intestine; TmaxLiver: time until maximal activity of the liver; AmaxGB and AmaxLiver: maximal activities of the GB and liver over one hour; ERliver: excretory ratio of liver over one hour
ACKNOWLEDGEMENT
Authors thanks for the efforts of Chun Ho Lee, Jong Cheol Kim, and Nam Ju Lee, the technologists of department of nuclear medicine, in Wonkwang University Hospital for technical assistance to acquire gamma camera images.
References
1. Shea JA, Berlin JA, Escarce JJ, Clarke JR, Kinosian BP, Cabana MD, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med. 1994. 154:2573–2581.
2. Choy D, Shi EC, McLean RG, Hoschl R, Murray IP, Ham JM. Cholescintigraphy in acute cholecystitis: use of intravenous morphine. Radiology. 1984. 151:203–207.
3. Fink-Bennett D. Augmented cholescintigraphy: its role in detecting acute and chronic disorders of the hepatobiliary tree. Semin Nucl Med. 1991. 21:128–139.
4. Angulo P. Use of ursodeoxycholic acid in patients with liver disease. Curr Gastroenterol Rep. 2002. 4:37–44.
5. Van de Meeberg PC, van Erpecum KJ, van Berge-Henegouwen GP. Therapy with ursodeoxycholic acid in cholestatic liver disease. Scand J Gastroenterol Suppl. 1993. 200:15–20.
6. Arrese M, Pizarro M, Solis N, Koenig C, Accatino L. Enhanced biliary excretion of canalicular membrane enzymes in ethynylestradiol-induced cholestasis. Effects of ursodeoxycholic acid administration. Biochem Pharmacol. 1995. 50:1223–1232.
7. Poupon R, Poupon RE. Ursodeoxycholic acid therapy of chronic cholestatic conditions in adults and children. Pharmacol Ther. 1995. 66:1–15.
8. Poddar U, Bhattacharya A, Thapa BR, Mittal BR, Singh K. Ursodeoxycholic acid-augmented hepatobiliary scintigraphy in the evaluation of neonatal jaundice. J Nucl Med. 2004. 45:1488–1492.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download