Abstract
Etidronate is an oral bisphosphonate compound that is known to reduce bone resorption through the inhibition of osteoclastic activity. The efficacy of etidronate for involutional (postmenopausal and senile) and glucocorticoid-induced osteoporosis, as well as that for other skeletal diseases, was reviewed in Japanese patients. Cyclical etidronate treatment (200 mg or 400 mg/day for 2 weeks about every 3 months) increases the lumbar bone mineral density (BMD) in patients with involutional osteoporosis and prevents incident vertebral fractures in patients with glucocorticoid-induced osteoporosis. The losses of the lumbar BMD in patients with liver cirrhosis and the metacarpal BMD in hemiplegic patients after stroke are prevented, and the lumbar BMD is possibly increased, preventing fragile fractures in adult patients with osteogenesis imperfecta type I. Furthermore, proximal bone resorption around the femoral stem is reduced and some complications may be prevented in patients who undergo cementless total hip arthroplasty. Oral etidronate treatment may also help to transiently relieve metastatic cancer bone pain followed by a decrease in abnormally raised bone resorption in patients with painful bone metastases from primary cancer sites, such as the lung, breast and prostate. Thus, oral etidronate treatment is suggested to be efficacious for osteoporosis, as well as other skeletal diseases associated with increased bone resorption, in Japanese patients. Randomized controlled trials needed to be conducted on a large number of patients to confirm these effects.
Etidronate is an oral bisphosphonate compound that is known to reduce bone resorption through the inhibition of osteoclastic activity, and has been widely used for the treatment of osteoporosis. According to the results of a meta-analysis of randomized controlled trials in foreign countries to test the efficacy of etidronate treatment for osteoporosis in postmenopausal women,1 etidronate treatment reduced vertebral fractures (relative risk [RR]: 0.60), but had no effect on non-vertebral fractures (RR: 1.00). Etidronate, relative to a control, increased the bone mineral density (BMD) by 4.27% in the lumbar spine, 2.19% in the femoral neck, and 0.97% in the total body after 3 years of treatment. Thus, the efficacy of etidronate treatment for vertebral fractures and in increasing the lumbar and femoral neck BMD in postmenopausal women with osteoporosis has been established. However, the skeletal effects of etidronate in postmenopausal women with osteoporosis have been demonstrated to be less than those of nitrogen-containing bisphosphonates.2
With regard to glucocorticoid-induced osteoporosis (GIO), a randomized controlled trial in foreign countries3 showed that etidronate treatment reduced vertebral fractures (RR: 0.57), but this effect was not statistically significant. Recently, however, a meta-regression analysis of the effect of bisphosphonates for GIO4 showed no significant difference in the efficacy of etidronate and nitrogen-containing bisphosphonates with respect to the lumbar BMD. Thus, unlike the case for osteoporosis in postmenopausal women, the efficacy of etidronate for GIO with respect to the BMD has been confirmed to be similar to that of nitrogen-containing bisphosphonates.
In Japan, etidronate has been used, not only for osteoporosis, but also for other skeletal diseases associated with increased bone resorption. In this paper, the efficacy of etidronate treatment for involutional (postmenopausal and senile) and glucocorticoid-induced osteoporosis, as well as that for other skeletal diseases, was reviewed in Japanese patients.
It is known that both early and late postmenopausal Japanese women usually show a high bone turnover.5 Thus, anti-resorptive agents, such as bisphosphonates, are expected to be efficacious for osteoporosis in elderly women. Fujita et al.6 evaluated the therapeutic effects of cyclical etidronate treatment on the lumbar BMD and the incidence of vertebral fractures in 414 patients with involutional osteoporosis in a controlled double-blind trial using 1α-hydroxyvitamin D3 (alfacalcidol) as a control. Cyclical etidronate treatment (200 mg and 400 mg/day for 2 weeks every 12 weeks) for 48 weeks increased the lumbar BMD by 2.4% and 3.4%, respectively, in patients with involutional osteoporosis, while it was sustained by alfacalcidol (1 µg/day, 0.5% decrease). Cyclical etidronate treatment significantly increased the lumbar BMD compared with alfacalcidol by decreasing the serum alkaline phosphatase and osteocalcin and urinary hydroxyproline/creatinine and calcium/creatinine levels. The incidences of vertebral fractures during the 48 weeks after initiation of treatment were 6.9% and 5.4% for 200 mg and 400 mg cyclical etidronate, respectively, and 15.5% for alfacalcidol, with a significant difference between the 400 mg cyclical etidronate and alfacalcidol treatments. These results suggest that cyclical etidronate treatment may be effective for increasing the lumbar BMD and preventing vertebral fractures in patients with involutional osteoporosis.
The efficacy of combined treatment with cyclical etidronate and vitamin D3 or vitamin K2 in postmenopausal women with osteoporosis has also been reported. It has been established in Japan that treatment with alfacalcidol slightly reduces bone turnover, sustains the lumbar BMD and prevents vertebral fractures in postmenopausal women with osteoporosis,7 while menatetrenone (vitamin K2) enhances γ-carboxylation of bone glutamic acid residues and secretion of osteocalcin, sustains the lumbar BMD and prevents osteoporotic fractures in patients with osteoporosis.8 Shiota et al.9 showed in a randomized controlled study conducted on 40 postmenopausal women with osteoporosis that 2 years of treatment with cyclical etidronate (200 mg/day for 2 weeks every 12 weeks) plus alfacalcidol (0.5 µg/day) and calcium lactate (2g/day) was more effective in increasing the lumbar BMD and preventing vertebral fractures than treatment with alfacalcidol and calcium lactate alone. Iwamoto et al.10 showed in an open-labeled randomized study conducted on 40 postmenopausal women with osteoporosis that one year of combined treatment with cyclical etidronate (200 mg/day for 2 weeks every 3 months) and alfacalcidol (1 µg/day) was more useful than treatment with cyclical etidronate alone for increasing the lumbar BMD, due to a more marked reduction in the level of urinary cross-linked N-terminal telopeptide of type I collagen (NTX). Iwamoto et al.11 also showed in a prospective study conducted on 100 postmenopausal women with osteoporosis that 2 years of combined treatment with cyclical etidronate (200 mg/day for 2 weeks every 3 months) and menatetrenone (45 mg/day) might be more efficacious in the prevention of incident vertebral fractures than the single treatment with cyclical etidronate. These results suggest the efficacy of the combined treatment of cyclical etidronate with active vitamin D3 or vitamin K2 in increasing the lumbar BMD or preventing vertebral fractures, respectively, in postmenopausal women with osteoporosis.
Osteoclastic activation and the destruction of cartilage and bone are observed in patients with rheumatoid arthritis (RA). Hasegawa et al.12 examined the efficacy of 72 weeks of treatment with cyclical etidronate (400 mg/day for 2 weeks every 12 weeks) for osteoporosis, bone resorption, inflammation and joint destruction in 63 patients with RA. Cyclical etidronate treatment reduced the urinary deoxypyridinoline and serum interleukin-6 levels and inhibited progression of the Larsen damage score for fingers, as based on radiographic images, suggesting that etidronate treatment is effective in inhibiting bone resorption and joint destruction in patients with RA.
Glucocorticoids exert effects on calcium metabolism, leading to accelerated osteoporosis and an increased incidence of fractures. Sambrook13 suggests that glucocorticoids affect bone through multiple pathways, influencing both bone formation and bone resorption. In particular, postmenopausal women receiving glucocorticoid are at the greatest risk of rapid bone loss and consequently, fractures, and should be actively considered for prophylactic treatment. With early therapy, the bone loss associated with glucocorticoid treatment can be effectively prevented or reversed. Based upon available evidence, the drug of choice for such prophylaxis has been a bisphosphonate, followed by a vitamin D metabolite or hormone replacement.
Several studies have shown the efficacy of etidronate treatment for GIO in Japan. Tanaka and Oshima14 investigated the efficacy of 2 years of treatment with cyclical etidronate (200 mg/day for 2 weeks every 3 months) in preventing the vertebral fractures caused by GIO in 103 patients with collagen diseases, including rheumatoid arthritis, and showed that this treatment significantly reduced the risk of vertebral fractures (Odd's ratio 0.02). They also showed a therapeutic effect of cyclical etidronate on GIO, focusing on the incidence of new vertebral fractures, in 136 patients with collagen diseases other than rheumatoid arthritis.15 The incidence of vertebral fractures during the 2-year study period was significantly reduced in the etidronate treatment groups (11% vs. 31% in the non-treatment group), suggesting the efficacy of cyclical etidronate treatment in preventing vertebral fractures in patients with GIO.
Sato et al.16 conducted a 3-year randomized study on 102 patients with connective tissue disease, who had taken more than 7.5 mg of prednisolone daily, for at least 90 days, to test the efficacy of cyclical etidronate treatment for GIO. Three years of treatment with cyclical etidronate (200 mg/day for 2 weeks every 3 months) plus 3 g calcium lactate and 0.75 µg alfacalcidol daily significantly increased the lumbar BMD by 4.8% compared to treatment with calcium lactate and alfacalcidol alone (only 0.4% increase), and prevented vertebral fractures. These results suggest that cyclical etidronate may be beneficial in increasing the lumbar BMD and preventing vertebral fractures in patients with GIO.
A few small studies have shown a preventative effect of etidronate against bone loss in patients receiving high-dose glucocorticoid. Fujita et al.17 showed that 3 months of treatment with etidronate (200 mg/day only for 2 weeks) reduced bone resorption and the natural progression of osteoporosis associated with aging or menopause in patients with nephritis. Nakayamada et al.18 also assessed the efficacy of 12 months of treatment with cyclical etidronate (200 mg/day for 2 weeks every 3 months) and alfacalcidol (1 µg/day) in preventing glucocorticoid-induced bone loss in patients with autoimmune diseases, who had started high-dose glucocorticoid therapy. The percentage change in the lumbar BMD during a 12-month period was -4.5% in the etidronate plus alfacalcidol group and -10.3% in the alfacalcidol alone group, with a significant difference between the two groups. The respective changes in the femoral neck BMD were + 2.3% and -2.5%, with a significant difference between the two groups. These results suggest that cyclical etidronate may have the potential to prevent the high-dose glucocorticoid-induced bone loss in patients with systemic autoimmune diseases.
A few studies have demonstrated the efficacy of etidronate treatment in osteoporosis induced by disability such as hemiplegia after a stroke. A significant reduction in the BMD was observed in the hemiplegic extremities of chronic stroke patients, which correlated with the degrees of paralysis and vitamin D deficiency due to malnutrition. Sato et al.19 showed in a randomized placebo-controlled 56-week study conducted on 98 hemiplegic patients following stroke that 56 weeks of cyclical etidronate treatment (400 mg/day for 2 weeks every 14 weeks) did not only retard the immobilization-induced loss of the metacarpal BMD by decreasing the serum pyridinoline cross-linked carboxyterminal telopeptide of type I collagen (1CTP) level, but also decreased the serum parathyroid hormone level and improved hypercalcemia, which was followed by an increased serum 1,25-dihydroxyvitamin D level. These results suggest that cyclical etidronate treatment may retard the BMD loss in hemiplegic stroke patients as it decreases the serum calcium level through the inhibition of bone resorption and causes a subsequent increase in the serum 1,25-dihydroxyvitamin D level.
Ikai et al.20 showed in a prospective study conduced on 81 postmenopausal women with hemiplegia after cerebrovascular accident that 3 months of treatment with etidronate (200 mg or 400 mg/day for only 2 weeks) and rehabilitation retarded the loss of the femoral neck BMD on the paralytic side (4.0% decrease in the treatment group vs. 9.6% decrease in the control group) by reducing the urinary pyridinoline and deoxypyridinoline levels from those at the baseline, especially in patients with low activities of daily living, as evaluated by using the FIM™ instrument. These results suggest that treatment with etidronate and increasing the activities of daily living may be helpful to reduce bone loss in hemiplegic disabled patients.
It is known that stopping training in terms of decreased physical activity may result in a loss of bone gain in exercise-trained subjects. Iwamoto et al.21 reported that bone gain through exercise was lost after cessation of exercise in postmenopausal women with osteoporosis; one or two years of brisk walking exercise increased the lumbar BMD from that of the baseline, but one-year cessation of exercise after one year of exercise resulted in its loss. However, cyclical etidronate treatment (200 mg/day for 2 weeks every 3 months) for two years just after cessation of 2 years of walking exercise prevented this loss in postmenopausal women with osteoporosis. These results suggest the efficacy of cyclical etidtonate in preventing the bone loss caused by decreased physical activity in exercise-trained postmenopausal women with osteoporosis.
It is known that liver cirrhosis induces osteopenia.22 An experimental study demonstrated that liver-cirrhosis-induced osteopenia may be attributable primarily to decreased bone formation.23 However, the efficacy of treatment with the anti-resorptive agent, etidronate, for osteopenia has been reported in patients with liver cirrhosis. Shiomi et al.24 showed in a randomized controlled 3-year study conducted on 50 women with cirrhosis caused by viral hepatitis infection that the lumbar BMD was sustained (0.6% decrease) in the etidronate treatment (200 mg/day for 2 weeks every 12 weeks) group, but decreased by 5.2% in the non-treatment group. However, no significant differences in changes in the serum osteocalcin and 1CTP levels were observed between the two groups. These results suggest that cyclical etidronate may have the potential to prevent liver- cirrhosis-induced bone loss. However, urinary bone resorption markers were not assessed in this study. Thus, further studies are needed to clarify the mechanism of liver-cirrhosis-induced osteopenia and confirm the effect of etidronate treatment on bone resorption in osteopenic patients with liver cirrhosis.
OI is a heterogeneous group of genetic disorders that affect the integrity of connective tissue. The hallmark of OI is bone fragility, although other manifestations, including osteoporosis, dentigenesis imperfecta, blue sclerae, easy bruising, joint laxity and scoliosis, are also common among OI patients. Although OI is a heritable disorder of bone formation, resulting in bone fragility, the activity of cancellous bone remodeling, bone resorption and/or bone turnover are also increased.25,26 The BMD usually remains low in adults with OI; however, very few studies have been reported on the treatment of osteopenia in adults with OI.
A case report has described the efficacy of etidronate treatment in a 36-year-old man with OI type I, who frequently experienced fragile fractures of the long bones of the upper and lower extremities and back pain caused by thoracic fragile vertebral fractures.27 Combined treatment with cyclical etidronate (200 mg/day for 2 weeks every 3 months) and alfacalcidol (1 µg/day, daily) increased the lumbar BMD by 3.9% after 18 months, reduced the back pain due to thoracic vertebral fractures and prevented new fragile vertebral and non-vertebral fractures. This report provided evidence that treatment with cyclical etidronate and alfacalcidol may potentially be useful for adult patients with OI type I.
Proximal bone resorption around the femoral stem is one of the major complications of cementless THA, which possibly results in late stem loosening and femoral fractures. Yamaguchi et al.28 showed in a randomized controlled study conducted on 42 patients with osteoarthritis of the hip joint secondary to acetabular dysplasia that 12 months of treatment with cyclical etidronate (400 mg/day for 2 weeks every 14 weeks) reduced the BMD loss in the proximal femur after cementless THA by decreasing the serum bone-specific alkaline phosphatase (BAP) and urinary NTX levels, suggesting that etidronate treatment may reduce proximal bone resorption around the femoral stem and help prevent some of the complications in patients undergoing cementless THA.
Bisphosphonates may have some anti-atherogenic actions. Koshiyama et al.29 prospectively examined the effect of cyclical etidronate treatment on the carotid arterial intima-media thickness in 57 patients with type 2 diabetes associated with osteopenia. One year of treatment with cyclical etidronate treatment (200 mg/day for 2 weeks every 3 months) decreased the intima-media thickness by 0.038 mm, which was significantly different from the change (0.023 mm increase) in the 57 control subjects, suggesting an anti-atherogenic action of etidronate at least in type 2 diabetes. However, the exact mechanisms by which etidronate exerts its anti-atherogenic effect remain uncertain.
Bone is a common site of metastasis in patients with advanced cancer. Bone metastasis frequently causes, not only skeletal destruction and pathological fractures, but also pain, and is commonly observed in patients with breast, prostate or lung cancer. In general, metastatic breast and lung cancers are osteolytic and prostate cancers are osteosclerotic. Bone metastasis is a cause of morbidity and mortality in patients with cancer, and is associated with a poor prognosis. Pain control is a crucial factor in determining the quality of life of patients during the last months of their lives. Since both osteolytic and mixed (osteolytic/osteosclerotic) types of bone metastases appear to show increased bone remodeling activity (bone resorption),30,31 drugs affecting bone metabolism, such as anti-resorptive agents, bisphosphonates may be effective for pain control in patients with osteolytic and mixed types of bone metastasis.
Oral bisphosphonates have not been used routinely in the treatment of cancer bone metastasis because of their low bioavailability. However, oral bisphosphonates may be helpful to relieve the pain caused by bone metastasis, if skeletal events, including bone pain, are mild without hypercalcemia. In Japan, the efficacy of oral bisphosphonates for the pain caused by cancer bone metastasis has not been established. The short-term effect of oral etidronate treatment on the mild metastatic cancer bone pain was examined in patients with lung, breast or prostate cancer (unpublished data). Twenty-three patients with lung, breast or prostate cancer were recruited: 13 with pain caused by bone metastasis from the primary cancer site; lung (n=6), breast (n=3) or prostate (n=4) (bone metastasis [M] group), and 10 with primary cancer of the lung (n=4), breast (n=4) or prostate (n=2), with no such evidence of skeletal-related events (non-bone-metastasis [non-M] group). The type of bone metastasis was osteolytic in patients with breast or lung cancer, and mixed (osteolytic/osteosclerotic) in patients with prostate cancer. None of the patients in the M group either needed morphine for pain relief or had hypercalcemia. During the study, the subjects continued taking nonsteroidal anti-inflammatory drugs as before the study. The levels of serum BAP and urinary NTX were significantly higher in the M group than in the non-M group (Table 1). Treatment with oral etidronate (400 mg/day for 2 weeks) in the M group patients reduced bone pain (evaluated by the face scale score, which is arranged in decreasing order of mood, and numbered from 1-10, with 1 representing the most positive mood [painless] and 10 representing the most negative mood [painful]) and was followed by a decrease in the urinary NTX level over 3 months (Fig. 1 and Table 2). The lack of significant changes in the serum BAP levels may be explained by the slower response of serum BAP to bisphosphonates than that of urinary NTX.32 It was surmised that a reduction in the serum BAP level would be observed after at least 3 months of etidronate treatment. These results suggested that patients with painful bone metastases from primary cancer sites, such as the lung, breast and prostate, had a higher bone turnover than those with no evidence of skeletal events, and that oral etidronate treatment might be helpful relieve metastatic cancer bone pain followed by a decrease in abnormally raised bone resorption. However, because this study was not a randomized placebo-controlled trial, our conclusion on the efficacy of oral etidronate treatment for metastatic cancer bone pain might, therefore, be weak, so further studies will be needed to confirm our results.
The efficacy of oral etidronate treatment for osteoporosis, as well as other skeletal diseases, associated with increased bone resorption has been demonstrated in Japan. Cyclical etidronate treatment increases the lumbar BMD in patients with involutional osteoporosis and reduces the vertebral fractures in patients with GIO. There is some evidence indicating the efficacy of cyclical etidronate for the BMD loss in patients with liver cirrhosis, bone fragility in adult patients with osteogenesis imperfecta type I, and proximal bone resorption around the femoral stem in patients undegoing cementless THA. Oral etidronate treatment may also transiently relieve the metastatic cancer bone pain in patients with painful bone metastases from primary cancer sites, such as the lung, breast and prostate. Randomized controlled studies conducted on a large number of patients will be needed to confirm these effects.
Figures and Tables
Fig. 1
Changes in Face Scale Score with Treatment in M Group. Data are expressed as mean±SD. The significance of the longitudinal changes in face scale score was determined by one-way ANOVA with repeated measurements. Data comparison among the time points was performed by paired t-test. One-way ANOVA with repeated measurement showed that face scale score significantly decreased (p < 0.001). Paired t-test showed that face scale score at weeks and 2 and 12 was significantly lower than that at week 0 (p < 0.001 and p < 0.01, respectively), but there was no significant difference in face scale score between weeks 2 and 12. *p < 0.01 vs week 0, **p < 0.001 vs week 0.
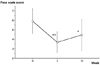
Table 1
Characteristics of Study Subjects and Levels of Biochemical Markers and Face Scale Score at Baseline

Table 2
Changes in Levels of Biochemical Markers with Treatment in M Group

Data are expressed as mean ± SD.
The significance of the longitudinal changes in biochemical markers was determined by one-way ANOVA with repeated measurements.
BAP, bone-specific alkaline phosphatase; NTX, cross-linked N-telopeptides of type I collagen.
ns, not significant; M group, bone metastasis group.
ACKNOWLEDGEMENTS
We thank Drs. K Kobayashi, M Kawamura and M Watanabe (Department of Surgery, Keio University School of Medicine) and Dr. K Asano (Department of Internal Medicine, Keio University School of Medicine) for providing subjects. We also thank Mr. T Fujino (Sumitomo Pharmaceuticals, Tokyo, Japan) for his help in the preparation of the manuscript.
References
1. Cranney A, Welch V, Adachi JD, Guyatt G, Krolicki N, Griffith L, et al. Etidronate for treating and preventing postmenopausal osteoporosis. Cochrane Database Syst Rev. 200. 4:CD003376.
2. Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C. Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev. 2002. 23:570–578.
3. Adachi JD, Bensen WG, Brown J, Hanley D, Hodsman A, Josse R, et al. Intermittent etidronate therapy to prevent corticosteroid-induced osteoporosis. N Engl J Med. 1997. 337:382–387.
4. Amin S, Lavalley MP, Simms RW, Felson DT. The comparative efficacy of drug therapies used for the management of corticosteroid-induced osteoporosis: a meta-regression. J Bone Miner Res. 2002. 17:1512–1526.
5. Yoshimura N, Hashimoto T, Sakata K, Morioka S, Kasamatsu T, Cooper C. Biochemical markers of bone turnover and bone loss at the lumbar spine and femoral neck: the Taiji study. Calcif Tissue Int. 1999. 65:198–202.
6. Fujita T, Orimo H, Inoue T, Kushida K, Sakurai M, Morita R, et al. Double-blind multicenter comparative study with alfacalcidol of etidronate disodium (EHDP) in involutional osteoporosis. Clin Eval. 1993. 21:261–302.
7. Orimo H, Shiraki M, Hayashi Y, Hoshino T, Onaya T, Miyazaki S, et al. Effects of 1α-hydroxyvitamin D3 on lumbar bone mineral density and vertebral fractures in patients with postmenopausal osteoporosis. Calcif Tissue Int. 1994. 54:370–376.
8. Shiraki M, Shiraki Y, Aoki C, Miura M. Vitamin K2 (menatetrenone) effectively prevents fractures and sustains lumbar bone mineral density in osteoporosis. J Bone Miner Res. 2000. 15:515–521.
9. Shiota E, Tsuchiya K, Yamaoka K, Kawano O. Effect of intermittent cyclical treatment with etidronate disodium (HEBP) and calcium plus alphacalcidol in postmenopausal osteoporosis. J Orthop Sci. 2001. 6:133–136.
10. Iwamoto J, Takeda T, Ichimura S, Matsu K, Uzawa M. Effects of cyclical etidronate with alfacalcidol on lumbar bone mineral density, bone resorption, and back pain in postmenopausal women with osteoporosis. J Orthop Sci. 2003. 8:532–537.
11. Iwamoto J, Takeda T, Ichimura S. Combined treatment with vitamin K2 and bisphosphonate in postmenopausal women with osteoporosis. Yonsei Med J. 2003. 44:751–756.
12. Hasegawa J, Nagashima M, Yamamoto M, Nishijima T, Katsumata H, Yoshino S. Bone resorption and inflammatory inhibition efficacy of intermittent cyclical etidronate therapy in rheumatoid arthritis. J Rheumatol. 2003. 30:474–479.
13. Sambrook PN. Steroid-induced osteoporosis. Ann Acad Med Singapore. 2002. 31:48–53.
14. Tanaka I, Oshima K. Prevention of vertebral fractures with therapeutic agents in corticosteroid-induced osteoporosis. Osteoporosis Japan. 2002. 10:244–247.
15. Tanaka I, Oshima K. Effects of menatetrenone, a vitamin K analog, on prevention of vertebral fracture in corticosteroid-induced osteoporosis. J Bone Miner Res. 2001. 16:531.
16. Sato S, Ohosone Y, Suwa A, Yasuoka H, Nojima T, Fujii T, et al. Effect of intermittent cyclical etidronate therapy on corticosteroid induced osteoporosis in Japanese patients with connective tissue disease: 3 year follow up. J Rheumatol. 2003. 30:2673–2679.
17. Fujita T, Satomura A, Hidaka M, Ohsawa I, Endo M, Ohi H. Acute alteration in bone mineral density and biochemical markers for bone metabolism in nephritic patients receiving high-dose glucocorticoid and oncecycle etidronate therapy. Calcif Tissue Int. 2000. 66:195–199.
18. Nakayamada S, Okada Y, Saito K, Tanaka Y. Etidronate prevents high dose glucocorticoid induced bone loss in premenopausal individuals with systemic autoimmune diseases. J Rheumatol. 2004. 31:163–166.
19. Sato Y, Asoh T, Kaji M, Oizumi K. Beneficial effect of intermittent cyclical etidtronate therapy in hemiplegic patients following an acute stroke. J Bone Miner Res. 2000. 15:2487–2494.
20. Ikai T, Uematsu M, Eun SS, Kimura C, Hasegawa C, Miyano S. Prevention of secondary osteoporosis postmenopause in hemiplegia. Am J Phys Med Rehabil. 2001. 80:169–174.
21. Iwamoto J, Takeda T, Ichimura S. Beneficial effect of etidronate on bone loss after cessation of exercise in postmenopausal osteoporotic women. Am J Phys Med Rehabil. 2002. 81:452–457.
22. Masaki K, Shiomi S, Kuroki T, Tanaka T, Monna T, Ochi H. Longitudinal changes of bone mineral content with age in patients with cirrhosis of the liver. J Gastroenterol. 1998. 33:236–240.
23. Tanaka S, Tsurukami H, Sakai A, Okimoto N, Ikeda S, Otomo H, et al. Effects of 1,25(OH)2D3 on turnover, mineralization, and strength of bone in growing rats with liver cirrhosis induced by administration of carbon tetrachloride. Bone. 2003. 32:275–283.
24. Shiomi S, Nishiguchi S, Kurooka H, Tamori A, Habu D, Takeda T, et al. Cyclical etidronate for treatment of osteopenia in patients with cirrhosis of the liver. Hepatol Res. 2002. 22:102–106.
25. Rauch F, Travers R, Parfitt AM, Glorieux FH. Static and dynamic bone histomorphometry in children with osteogenesis imperfecta. Bone. 2000. 26:581–589.
26. Brenner RE, Vetter U, Bollen AM, Morike M, Eyre DR. Bone resorption assessed by immunoassay of urinary cross-linked collagen peptides in patients with osteogenesis imperfecta. J Bone Miner Res. 1994. 9:993–997.
27. Iwamoto J, Takeda T, Ichimura S, Matsu K, Uzawa M. Effects of cyclical etidronate with alfacalcidol on lumbar bone mineral density, bone resorption, and back pain in postmenopausal women with osteoporosis. J Orthop Sci. 2003. 8:532–537.
28. Yamaguchi K, Masuhara K, Yamasaki S, Nakai T, Fuji T. Cyclical therapy with etidronate has a therapeutic effect against local osteoporosis after cementless total hip arthroplasty. Bone. 2003. 33:144–149.
29. Koshiyama H, Nakamura Y, Tanaka S, Minamikawa J. Decrease in carotid intima-media thickness after 1-year therapy with etidronate for osteopania associated with type 2 Diabetes. J Clin Endocrinol Metab. 2000. 85:2793–2796.
30. Galasko CS. Mechanisms of bone destruction in the development of skeletal metastasis. Nature. 1976. 263:507–508.
31. Paterson AHG, Kanis JA, Powles TJ, McCloskey E, Hanson J, Ashley S. Role of bisphosphonates in prevention and treatment of bone metastases from breast cancer. Can J Oncol. 1995. 5:54–57.
32. Braga de Castro Machado A, Hannon R, Eastell R. Monitoring alendronate therapy for osteoporosis. J Bone Miner Res. 1999. 14:602–608.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download