Abstract
The aim of this study was to investigate the factors affecting cough ability, and to compare the assisted cough methods in patients with Duchenne muscular dystrophy (DMD). A total seventy-one male patients with DMD were included in the study. The vital capacity (VC) and maximum insufflation capacity (MIC) were measured. The unassisted peak cough flow (UPCF) and three different techniques of assisted peak cough flow were evaluated. UPCF measurements were possible for all 71 subjects. But when performing the three different assisted cough techniques, peak cough flows (PCFs) could be obtained from only 51 subjects. The mean value of MICs (1801 ± 780 cc) was higher than that of VCs (1502 ± 765 cc) (p < 0.01). All three assisted cough methods showed a significantly higher value than the unassisted method (F=80.92, p < 0.01). The manual assisted PCF under MIC (MPCFmic) significantly exceeded those produced by manual assisted PCF (MPCF) or PCF under MIC (PCFmic). The positive correlation between the MIC, VC difference (MIC-VC), and the difference between PCFmic and UPCF (PCFmic-UPCF) was seen (r=0.572, p < 0.01). The preservation of pulmonary compliance is important for the development of an effective cough as well as assisting the compression and expulsive phases. Thus, the clinical importance of the inspiratory phase and pulmonary compliance in assisting a cough should be emphasized.
Duchenne muscular dystrophy (DMD) causes progressive weakness of respiratory muscles in common with other skeletal muscles.1 The weakened respiratory muscles lead to alterations of the lung volumes. The lungs can not be fully expanded up to their maximal capacity, nor can they be compressed to the point of the smallest residual volume.2 When the condition of a chronically limited range of motion in chest walls is prolonged, the compliances of the lungs and thorax tissues eventually decrease.2,3 The low compliance of the pulmonary system prevents attainment of high lung volumes and this diminishes the cough effectiveness.4
An effective cough must be preceded by the inhalation of a sufficient air volume, and strong expiratory muscles are needed for the generation of high thoracoabdominal pressures.5 Based on this cough mechanism, several conventional cough assisting methods have been utilized in order to promote the effectiveness of cough for patients with respiratory muscle weakness.6-9 The greater portion of the conventional cough assisting methods have aimed at aiding the weakened expiratory muscles. However, an efficient cough cannot be obtained by assisting only expiratory muscles in patients with a markedly decreased inspiratory capacity.10-12 Patients with a limited pre-cough volume are rarely able to cough effectively, and so the pre-cough inspiratory volume must be assisted in those patients. Therefore, several studies of volume assisted methods have been tried to emphasize the importance of the pre-cough volume.12-15 The comparison of the efficacy of cough assistances between the pre-cough volume assisted method and the manual assisted method which helps only the weakened expiratory muscles has also conducted for patients with spinal cord injury,13 chronic obstructive pulmonary disease and neuromuscular disease.15
The distensibility of pulmonary system should be maintained in order to increase the pre-cough volume by passive insufflation in patients with a reduced inspiratory capacity. This implies that the pulmonary compliance can affect the effectiveness of assisting a cough. Accordingly, the relationship between pulmonary compliance and the extent of improvement in peak cough flows (PCFs) was investigated,11 but the extent of assisted PCF in that study was not the isolated effect of pulmonary compliance (volume assistance) because passive insufflation was performed together with assisting the expiratory muscles.
In the present study, the direct comparison of PCFs between the volume assisted method and the manual assisted method in DMD patients was attempted. The correlation between the magnitude of passive insufflation, which is an indirect indicator of pulmonary compliance, and the extent of the assisted PCF was also investigated in order to emphasize the importance of pulmonary compliance and pre-cough volume in assisting a cough.
The study was conducted on seventy-one patients who were able to cooperate with the medical personnel, and they were diagnosed on the basis of a clinical history, physical findings, genetic evaluation, and laboratory studies that include muscle enzymes, electromyography, DNA analysis or muscle biopsy. The protocol of the study was approved by the hospital ethical committee.
VC and MIC were measured using a Wright spirometer (Ferraris Development & Engineering Co Ltd, Northants, UK) in the sitting position. For MIC measurement, the subject was made to take the deepest possible breath, hold it, and then air staking was consecutively delivered up to the maximum volume that could be held with a closed glottis by using a manual resuscitator via a mouth piece or oronasal interface. Then, by using the Wright spirometer, the maximally exhaled volume that were observed in at least three attempts was recorded.
PCFs were measured by having the subject cough as forcibly as possible through a peak flow meter (Health Scan Products Inc, Cedar Grove, NJ). The PCFs were measured under four different performances.11,12 (i) Unassisted PCF (UPCF): The subject was made to take the deepest possible breath, and then the subject gave a strongest possible coughing. (ii) Manual assisted PCF (MPCF): The subject took the deepest possible breath, and then the subject was made to cough with manual pressure being applied to the abdominal area at the time of coughing. (iii) PCF under MIC (PCFmic): The subject was made to take the deepest possible breath, hold it, and then air stacking was consecutively delivered up to the maximum volume that could be held with a closed glottis by using a manual resuscitator via a mouth piece or oronasal interface. The subject then was made to give the strongest possible coughing. (iv) Manual assisted PCF under MIC (MPCFmic): After the subject was made to take the deepest possible breath, hold it, and then air stacking was consecutively delivered up to the maximum volume that could be held with a closed glottis by using a manual resuscitator via a mouth piece or oronasal interface, the subject was made to give the strongest possible coughing as an abdominal thrust was timed to coughing. Each of the four maneuvers was conducted at least three trials, and the highest value was obtained from each maneuver.
As for the assessment of subjects' abilities and limitations, grade 1 through 8 were used as categories as suggested by Swinyard and others.16
The data was analyzed using SPSS 11.0 software for Windows program (SPSS Inc, Chicago, IL, USA). Paired samples t-test was involved in comparing vital capacity and MIC, and repeated measure analysis of variance was used for the comparisons between UPCF and the three different techniques. If repeated measure analysis of variance detected significance, a post hoc comparison test was performed by using a least significant difference (LSD). The correlation between the degree of pulmonary compliance and the difference between MIC and unassisted PCFs was made by coefficients of correlation. A p value less than 0.01 was regarded as being statistically significant.
All 71 subjects were males and the mean age was 14.0 ± 5.4 years old. The mean age at the time of diagnosis was 6.8 ± 2.5 years old and the subjects became dependent on a wheelchair at 10.3 ± 1.8 years old. The mean height and weight were 143.4 ± 15.3 cm and 37.6 ± 14.5 kg, respectively. The mean Swinyard functional grade was 6.7 ± 1.0. Among the 71 patients, 2 patients were ranked as second grade, 1 patient fifth, 17 patients sixth, 41 patients seventh and 10 patients were eighth grade.
UPCF measurements were possible for all 71 subjects. But when performing the three different assisted cough techniques, PCFs could be obtained from only 51 subjects. UPCF of all 71 subjects was 203.9 ± 65.4 liters/min. As for the 51 subjects who underwent all four different maneuvers, UPCF was 217.7 ± 65.9 liters/min, MPCF was 250.6 ± 66.2 liters/min, PCFmic was 257.8 ± 65.8 liters/min, and MPCFmic was 285.8 ± 75.9 liters/min, respectively. No statistically significant difference was observed between MPCF and PCFmic (F=80.92, p < 0.01). However, two assisted cough techniques showed a significantly higher value compared to the UPCF (F=80.92, p < 0.01). The MPCFmic value significantly exceeded those value produced by MPCF or PCFmic (F=80.92, p < 0.01) (Table 1).
In the 51 subjects who underwent all four maneuvers, the difference between MIC and VC (MIC-VC) was 438.4 ± 277.1 cc, while the difference between PCFmic and UPCF (PCFmic-UPCF) was 43.2 ± 25.9 liters/min. A positive correlation was observed between the MIC-VC and the PCFmic - UPCF (r=0.572, p < 0.01) (Fig. 1). In other words, the larger the MIC, VC difference, the greater was the extent of the assisted PCF.
A cough is an essential protective reflex that keeps debris out of airways and clears excessive secretions during respiratory tract infections, and it thereby prevents airway or pulmonary diseases such as pneumonia, atelectasis and acute respiratory failure.19 Normal cough consists of a 3-step process of the inspiratory phase, compression phase and the expulsive phase.5 Yet for patients with neuromuscular disease, often the inspiratory muscles are not only too weak to provide a deep inspiration but the weak expiratory muscles may also fail to generate sufficient pressure against a closed glottis to create functional cough flows. Therefore, an assisted cough should be required for effectively clearing of airway secretions in patients with neuromuscular disease. To assist a cough, several methods for aiding expiratory muscles to generate the high thoracoabdominal pressures, such as respiratory muscle training,6,7 functional electrical stimulation of abdominal muscles8,9 and conventional assisted cough with abdominal thrust9,13,15 have been proposed for patients with respiratory muscle weakness.
Nobody can cough effectively with small pre-cough volume, so the pre-cough volume must be assisted in these debilitated cases. However, the majority of cough assisting methods have been focused to assist on an expulsive phase. Normal individuals inhale an air volume of 85 to 90% of their inspiratory capacity to obtain sufficient PCFs,19 but in DMD patients, the weakened inspiratory muscles prevents them from inhaling sufficient air volume on their own.11 If their weakened inspiratory muscles cannot fully inflate the lungs for a long time, the unstretched tissues become stiffened and the breathing muscles undergo fibrotic changes, leading to the reduction of chest wall compliance. Additionally, microatelectasis spreads in lung parenchyme, and consequently decreasing the lung compliance.3,7 Thus, the contractures of the lungs and thorax tissues result in limiting the lung volume attained prior to coughing during the inspiratory phase, and this becomes a problem when an assisted cough is needed.10 However, their ability to cough can be improved by compulsorily stacking additional pre-cough volume after self-inspiration during the inspiratory phase.10-12,20
MIC is the maximum volume of air that can be insufflated into the lungs, and it is an indirect indicator of pulmonary compliance.10 In our results, MIC was measured to be higher than VC. Such findings could suggest that an additional increase in pre-cough volume during the inspiratory phase could enhance the ability to assist cough,11 proving that the PCFmic is higher than the UPCF in this study.
The difference between MIC and VC was found to be positively correlated to the difference between assisted PCF and UPCF in a previous study.11 However, in that study, the manual assisted method and volume assisted method were simultaneously carried out in measuring assisted PCF, and the consequence of this was that their results have limits in reflecting the exact correlation between the impact of passive insufflation and the extent of assisted PCF. We found that the MIC, VC difference and the difference between PCFmic and UPCF showed a significantly positive correlation. This finding reflects that the more the pulmonary compliance is maintained, the better PCF can be augmented by increasing insufflation volume during the pre-cough stage. In other words, if lung expansion with passive insufflation is performed regularly, the pulmonary compliance will be maintained as range-of motion exercises are traditionally used for the prevention of upper and lower limb contractures.10,21
A volume assisted method, although it only assists cough during the inspiratory phase, can afford to effectively assist the expiratory muscles. In other words, a large inspiratory reserve volume significantly improves the expiratory muscle function with optimization of the length-tension relationship, and the large inspiratory reserve volume also increases the elastic recoil of the lung with the consequence that greater expiratory pressures and flows can be generated.22,23 In addition, regular lung expansion by air stacking helps prevent atelectasis and it allows for efficient gas exchange by providing the advantage of fuller ventilation of the lungs.
An impairment of cough from a dysfunction of the respiratory muscles becomes inevitable in DMD patients. Hence, to effectively assist the weakened respiratory muscles in these patients, and to prevent respiratory complications, the factors affecting the ability to cough must be correctly evaluated. As shown in our current study, the maintenance of pulmonary compliance can help significantly for increasing the effectiveness of coughing in the event of profuse airway secretions.
In conclusion, not only helping the weakened expiratory muscles but also increasing pre-cough volume should be emphasized to optimally assist a cough in DMD patients, and our study has shown that pulmonary compliance plays a crucial role in increasing an assisted PCF.
Figures and Tables
Fig. 1
Relationship between the MIC, VC difference (MIC-VC), and the difference between PCFmic and UPCF (PCFmic-UPCF). The MIC-VC correlated significantly with the PCFmic-UPCF (r=0.572; p < 0.01). MIC, maximum insufflation capacity; VC, vital capacity; PCFmic, peak cough flow under maximum insufflation capacity; UPCF, unassisted peak cough flow.
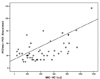
Table 1
Comparisons between UPCF and Each Assisted PCF (n=51)
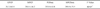
Data are expressed as mean ± SD (liters/min).
UPCF, unassisted peak cough flow; PCF, peak cough flow; MPCF, manual assisted peak cough flow; PCFmic, peak cough flow under maximum insufflation capacity; MPCFmic, manual assisted peak cough flow under maximum insufflation capacity.
*p < 0.01.
†Both the values of MPCF and PCFmic, which were similar, were higher than that of UPCF but lower than that of MPCFmic.
References
1. Inkley SR, Oldenburg FC, Vignos PJ. Pulmonary function in Duchenne muscular dystrophy related to stage of disease. Am J Med. 1974. 56:297–306.
2. Estenne A, Heilporn A, Delhez L, Yernalt JC, Troyer A. Chest wall stiffness in patients with chronic respiratory muscle weakness. Am Rev Respir Dis. 1983. 128:1002–1007.
3. Estenne M, Gevenois PA, Kinnear W, Soudon P, Heilporn A, De Troyer A. Lung volume restriction in patients with chronic respiratory muscle weakness: the role of microatelectasis. Thorax. 1993. 48:698–701.
4. Suarez AA, Pessolano FA, Monteiro SG, Ferreyra G, Capria ME, Mesa L, et al. Peak flow and peak cough flow in the evaluation of expiratory muscle weakness and bulbar impairment in patients with neuromuscular disease. Am J Phys Med Rehabil. 2002. 81:506–511.
5. Scanlan C, Myslinski MJ. Scanlan CL, Wilkins RL, Stoller JK, editors. Bronchial hygiene therapy. Egan's Fundamentals of Respiratory Care. 1999. 7th ed. St. Louis: Mosby;792–793.
6. Biering-Sorensen F, Knudsen JL, Schmidt A, Bundgaard A, Christensen I. Effect of respiratory training with a mouth-nose-mask in tetraplegics. Paraplegia. 1991. 29:113–119.
7. Estenne M, Knoop C, Vanvaerenbergh J, Heilporn A, De Troyer A. The effect of pectoralis muscle training in tetraplegic subjects. Am Rev Respir Dis. 1989. 139:1218–1222.
8. Linder SH. Functional electrical stimulation to enhance cough in quadriplegia. Chest. 1993. 103:166–169.
9. Jaeger RJ, Turba RM, Yakony GM, Roth EJ. Cough in spinal cord injured patients: comparison of three methods to produce cough. Arch Phys Med Rehabil. 1993. 74:1358–1361.
10. Kang SW, Bach JR. Disorders of ventilation: weakness, stiffness, and mobilization. Chest. 2000. 117:301–303.
11. Kang SW, Bach JR. Maximum insufflation capacity: vital capacity and cough flows in neuromuscular disease. Am J Phys Med Rehabil. 2000. 79:222–227.
12. Kang SW, Bach JR. Maximum insufflation capacity. Chest. 2000. 118:61–65.
13. Kirby NA, Barnerias MJ, Siebens AA. An evaluation of assisted cough in quadriparetic patients. Arch phys Med Rehabil. 1966. 47:705–710.
14. Bach JR. Mechanical insufflation-exsufflation. Comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest. 1993. 104:1553–1562.
15. Sivasothy P, Brown L, Smith IE, Shneerson JM. Effect of maunally assisted cough and mechanical insufflation on cough flow of normal subjects, patients with chronic obstructive pulmonary disease (COPD), and patients with respiratory muscle weakness. Thorax. 2001. 56:438–444.
16. Swinyard CA, Deaver GG. Gradients of functional ability of importance in rehabilitation of patients with progressive muscular and neuromuscular diseases. Arch Phys Med Rehabil. 1957. 38:574–579.
17. Morris JF. Spirometry in the evaluation of pulmonary function. West J Med. 1976. 125:110–118.
18. DaCosta JL. Pulmonary function studies in healthy Chinese adults in Singapore. Am Rev Respir Dis. 1971. 104:128–131.
19. Leith DE. Brain JD, Proctor D, Reid L, editors. Cough. Lung Biology in Health and Disease. 1977. New York: Marcel Dekker;545–592.
20. Chatwin M, Ross E, Hart N, Nickol AH, Polkey MI, Simonds AK. Cough augmentation with mechanical insufflation/exsufflation in patients with neuromuscular weakness. Eur Respir J. 2003. 21:502–508.
21. Tzeng AC, Bach JR. Prevention of pulmonary morbidity for patients with neuromuscular disease. Chest. 2000. 118:1390–1396.
22. McCool FD, Leith DE. Pathophysiology of cough. Clin Chest Med. 1987. 8:189–195.
23. Hadjikoutis S, Wiles CM, Eccles R. Cough in motor neuron disease: a review of mechanisms. QJM. 1999. 92:487–494.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download