This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
We wanted to compare the clinical usefulness of conventional galactography and MR contrast galactography for diagnosing patients with nipple discharge.
Materials and Methods
Both conventional galactography and MR contrast galactography were performed prospectively in 16 patients. Gadopentate dimeglumine (0.1 ml) was mixed with non-ionic contrast medium (0.9 ml) to obtain a resultant volume of 1 ml and this was used for both examinations. Following conventional galactography, MR contrast galactography was performed after direct injection of contrast media into the duct.
Results
Conventional galactography and MR contrast galactography were concordant in 13 (81%) of 16 patients; the results were normal in five, ductal dilatation was noted in four and intraductal filling defects were noted in four. The remaining three (19%) patients demonstrated discordant findings on the two examinations. While conventional galactography revealed filling defects, the MR contrast galactography results were normal in two patients. The third patient had kinks-stricture on conventional galactography and MR contrast galactography showed ductal dilatation. This suggested there were false positive results for the three patients' conventional galactography, and all the three patients with discordant results underwent surgery and the histopathologic evaluation showed fibrocystic changes.
Conclusion
MR contrast galactography may be used as an alternative imaging modality for making the diagnosis of pathologic nipple discharge. However, statistically supported studies with large pools of subjects for comparing the galactography and MR contrast galactography results are needed to confirm our findings.
Go to :

Keywords: Breast, Galactography, Nipple discharge, Magnetic resonance (MR)
Pathologic nipple discharge is defined as spontaneous secretion from a single pore of one breast. Although pathologic nipple discharge is much more frequently associated with benign breast disease, cancer is a rare but important cause of nipple discharge (
1,
2).
Galactography is a procedure that often helps to define the cause of pathologic nipple discharge, and performing preoperative galactography allows for determining the extent of the disease, identifying the central and peripheral lesions and guidance of surgical excision. Galactography also avoids incomplete and/or excessive removal of breast tissue by identifying the abnormal ductal system (
3,
4). Nevertheless, the use of X-rays and the images obtained from a compressed breast constitute the disadvantages of conventional galactography (CG).
Magnetic resonance mammography is a well-established procedure with high contrast resolution and it is frequently used for determining the characteristics of tumors of the breast; this modality has high sensitivity ranging from 94% to 99% and specificity that ranges from 20% to 80%. MR imaging can be used as an adjunctive imaging modality for identification of occult and intraductal lesions. Imaging in the orthogonal planes and the potential for differentiation of benign from malignant causes are the major advantages of the modality. Yet MR imaging is currently less available and more costly than galactography (
5-
9).
In order to overcome the problems of CG, MR galactography could be an alternative procedure for providing three dimensional images and images in the orthogonal planes. In addition, the lack of radiation seems another major advantage of this imaging modality. In the light of this information, this study was undertaken to evaluate the effectiveness of MR contrast galactography (MRCG) for making the diagnosis of 16 patients with pathologic nipple discharge and we compared the results of CG and MRCG.
MATERIALS AND METHODS
This prospective study included 16 female patients (mean age, 44 years; range, 30-71 years) with pathologic nipple discharge.
All the patients had unilateral breast discharge. Eight of 16 patients had bloody discharge and the remaining eight patients had serous or seroanginous discharge. Prior to CG and MRCG, all the patients underwent routine mammography (HFX Plus -Fischer Imaging, Denver, CO) in two planes, and the mammography was interpreted using the Breast Imaging Reporting and Data System (BI-RADS) classification (
10).
None of the patients had a palpable abnormality or a history of cancer. In 15 of 16 patients, the mammographic results were negative and they were classified as BI-RADS category 1. In one patient, a well-circumscribed, oval, regularly contoured high density mass was noted on mammography, and ultrasound revealed a well circumscribed, oval, regularly contoured hypoechoic mass that was probably a benign solid mass. This patient was classified as BI-RADS category 3.
A mixture of 0.1 ml Gd DTPA (gadopentate dimeglumine, Magnevist; Schering, Berlin, Germany ) and 0.9 ml non-ionic (Ultravist 300/100; Schering, Berlin, Germany) contrast medium was prepared to obtain a resultant volume of 1 ml for use in both the CG and MRCG. Such a mixture was prepared with taking into account that Gd DTPA acts as a weak contrast medium in X-ray examinations and non-ionic contrast medium acts like saline or water in MR examinations. This mixture was used to obtain an image of the secreting ducts and filling defects and/or other pathologies on both CG and in MRCG without a need for a second intervention. A single cannulation was done for both examinations.
The procedure and the potential complications were explained to all the patients and informed consent was obtained. A 30-gauge needle (PBN Medicals, Stenlose, Denmark) was used to cannulate the secreting ducts. The mixed contrast material was injected manually with the patient in a sitting position until the patient had a sensation of fullness or pain. First, CG was performed with mild compression and the standard craniocaudal and 90 degree true lateral films were obtained. The magnified views were acquired if needed.
MR contrast galactography was performed right after CG with using a 1.5 tesla MR unit (Somatom Vision Plus; Siemens, Erlangen, Germany) and all the patients underwent imaging in the prone position with using a dedicated breast coil. Three-dimensional gradient echo fat-saturated turboflash sequences (TR/TE: 32/4, flip angle: 20°, FOV [field of view]: 160 mm, Matrix: 256×256) were used and the multiplanar, maximum intensity projection reconstruction images were obtained for three dimensional evaluation.
All the MRCG images and CG images were interpreted independently by two experienced radiologists who were aware of the patients clinical information, including the history of nipple discharge and the findings of the physical examination. The radiographic findings on CG and MRCG were classified as normal findings (tapering to peripheral ducts without filling defects), ductal dilatation (a duct with over a 2 mm width), filling defects (multiple or unique) and a kinky ductus (bending ducts). Subsequently, a second evaluation was done by the same radiologists to reach a consensus of the results obtained on both examinations.
After the comparison of both examinations by the two radiologists, based on the results and clinical status, the patients underwent surgery and the pathologic results were also evaluated.
Go to :

RESULTS
Both examinations were performed safely, and all the patients well tolerated the procedures. During the examinations, no technical insufficiency or major complications were observed. As a minor complication, only five patients complained of mild pain for a short time during cannulation and injection.
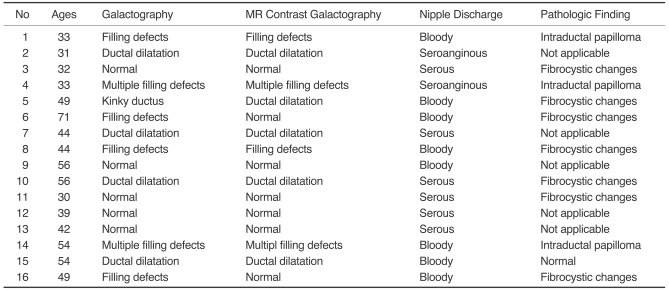
Conventional galactography demonstrated filling defects in six patients (38%), ductal dilatation in four patients (25%), kinks and stricture in one patient (6%), and no abnormal finding in five (31%). On the other hand, MRCG revealed ductal dilation in five patients (31%), normal ductal pattern in seven (44%), and filling defects in the remaining four patients (25%). On comparing the results obtained on both examinations of the 16 patients, there was a consensus for 13 patients (81%) and discordance for three patients (19%) (
Table 1). While CG revealed filling defects, the MRCG was interpreted by one of the radiologists that two of the patients within the discordant group were normal (
Fig. 1) and the other case that was reported as kinks-stricture on CG and showed ductal dilatation on the MRCG.
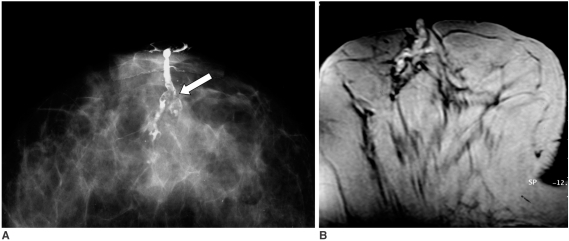 | Fig. 1
49-year-old woman with bloody discharge.
A. Conventional galactography on craniocaudal projection shows irregular filling defects (arrow). Note duct is extended due to compression.
B. MR contrast galactography on axial plane at same level shows no filling defects and pathology revealed fibrocyctic changes. Note duct is minimally heterogeneous, possibly as result of different degrees of hemorrhage mixed with contrast material.

|
Table 1
Findings of Conventional Galactography and MR Contrast Galactography
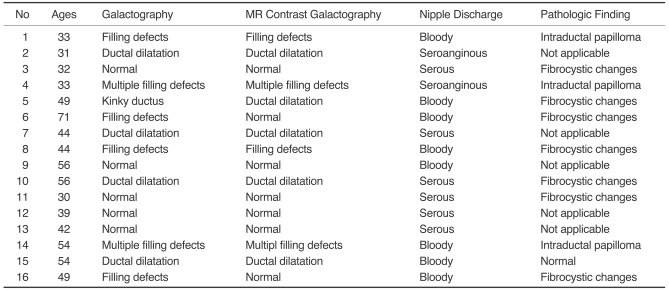

Surgery was performed on 11 of the 16 cases. The surgeon was informed preoperatively about the results of both examinations. Histological review demonstrated fibrocystic changes in seven patients, intraductal papilloma in three and normal findings in one patient. All the patients with papillomas that were postoperatively confirmed via the pathological evaluation results were in the group of patients with concordant results, and both CG and MRCG revealed filling defects (
Figs. 2,
3).
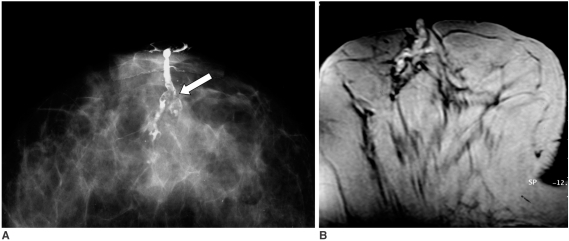
 | Fig. 2
54-year-old woman with bloody discharge.
A. Conventional galactography on craniocaudal projection demonstrates dilated ducts and filling defects (arrows).
B. MR contrast galactography on axial plane shows hyperintense dilated ducts and hypointense multiple filling defects (arrows). Pathology revealed intraductal papillomas.

|
 | Fig. 3
33-year-old woman with bloody discharge.
A, B. Both conventional galactography (A) and MR contrast galactography (B) reveal filling defects (arrows) and pathology results were reported as intraductal papillomas.

|
All three patients with discordant results underwent surgery and the histopathologic evaluation showed fibrocystic changes.
Go to :

DISCUSSION
The proper evaluation and management of nipple discharge are controversial. While many surgeons advocate subareolar duct excision without using a diagnostic tool, others prefer galactography as the choice of imaging.
Conventional galactography plays an essential role for diagnosing nipple discharge because of its high sensitivity for detecting intraductal lesions; it allows diagnosis of the underlying condition, it defines the extent of disease, identifies central and peripheral lesions and it guides surgical excision. Yet it has major disadvantages such as a relatively high false positive rate, an unknown negative predictive value and an inability to differentiate between malignant and benign lesions (
4,
11,
12). Besides, compression of the breast may lead to misjudging the exact location of lesions while the patients are lying supine on the operating table. Expose to X-rays is another shortcoming of the modality. To overcome these problems, we developed a new method of galactography using magnetic resonance with contrast material imaging in the orthogonal planes.
Several studies that evaluated MR imaging as a diagnostic tool for breast imaging reported that MRI has high sensitivity for detecting breast cancer. There are multiple reports in the literature on MR imaging depicting mammographically and clinically occult breast carcinoma and DCIS (ductal carcinona in situ) (
5-
9). On the basis of this knowledge, MR imaging seems to have the potential for detecting intraductal disease and it might be useful for evaluating nipple discharge. There are several different techniques that have been reported on for diagnosing nipple discharge with MR imaging (
13-
18).
Orel et al. (
13) performed contrast material enhanced MR imaging for 23 patients with pathologic nipple discharge. In their study, for 11 of 15 patients who underwent excisional biopsy, the histopathologic correlation with the MR imaging findings was reported to be 73%, but galactography was performed for only two patients, with a negative finding in one and no success in the other. Thus, any comparison of MR imaging and galactography was not possible.
MR galactography without using intraductal contrast material is another technique and it does have the same advantages and similar shortcomings of MR imaging, but performing MR galactography seems feasible in women for whom galactography cannot be achieved because of dye allergy, an inability to cannulate the duct or patient preference, as was stated by Rovno et al. (
14).
To the best of our knowledge, there are no studies in the literature that have compared CG and MRCG. Only Yoshimoto et al. (
15) have performed MR contrast galactography combined with MR imaging after galactography was performed in a patient, and the contrast material was injected both intravenously and into the discharging duct. While only intraductal spreading carcinoma was shown on the galactography, all the portions of the entire discharging duct were shown and the surrounding area was enhanced with Gd-DTPA on MR galactography. It was mentioned that MR galactography may be used to supplement CG, and especially for evaluating the extent of disease.
In recent years, Kanemaki et al. (
16) have reported MR ductography with using a microscopic coil for the assessment of intraductal lesions without using intraductal contrast material and cannulation. In that study, the MR ductography of 10 of 15 patients was followed by CG for making comparison. Intraductal tumors were seen on the conventional ductography in seven of 10 patients, and MR ductography detected all the tumors shown by CG. A similar study by Bhattarai has recently described the features of intraductal papillomas on MR ductography with using a microscopic coil. The papillomas appeared in most of their cases as well-circumscribed masses with early enhancement and delayed washout that was associated with a dilated duct, and predominantly showed high signal intensity on T1 and T2-weighted images (
16,
17). In both studies, comparison of the results with those of CG was not done for all the patients. Based on the results of these two studies, it seems that cannulation and use of contrast material may be the weakness of our present study. However, in the centers that lack a microscopic coil, MRCG with using a conventional breast coil can be an alternative imaging modality to CG. Thus, the comparison of all the patients with CG might be considered as an advantage of our study over these two previous studies.
MR ductography (hydrography) with using heavily T2-weighted imaging and fat suppression is another possible noninvasive modality that does not require cannulation, but this technique cannot reveal abnormalities when the ducts are not dilated (
18). Although cannulation seems to be a disadvantage in our study, when the ducts are not dilated, cannulation and filling the ducts with contrast material can be a benefit of the modality.
In the present study, CG and MRCG were compared using a mixture of non-ionic contrast material with MR contrast material, which provided imaging by both modalities with using a single cannulation. The safety of a mixture of gadolinium and nonionic contrast material may be questionable. Brown et al. (
19) reported that Magnevist can be mixed with either ionic or non-ionic contrast agents before MR imaging without any release of free gadolinium ions, and this may provide additional helpful information before MR imaging. Similarly, neither the iodinated contrast materials nor the other materials such as saline, lidocaine or epinephrine would result in the release of free gadolinium ion in the solution. Therefore, achieving MRCG with using a mixture of GD-DTPA with saline as mentioned above seems safe and harmless for patients with pathologic nipple discharge. In the light of this information, combining GD-DTPA with saline and performing only MRCG with a saline mixture might be a choice and this could offer many advantages. Imaging in three planes of all the portions of the discharging duct ensures obtaining additional information before surgery and protection from X-rays and the possible dye allergy that is due to non-ionic contrast material.
In our study, within the discordant group, the two patients with bloody discharge might have been misdiagnosed as having filling defects on CG, and these filling defects were obscured by the high contrast on MRCG; they were reported as normal because of a little hematoma that was associated with hemorrhage in the subacute phase or because of the high protein content in the ductus. The other patient was reported as having kinks on CG and ductal dilatation on MRCG, which might be the advantage of performing MR imaging in three planes as the lesion was misinterpreted on the CG in two planes.
The histopathological examination results were reported as fibrocystic changes in all cases in the discordant group (3 patients). CG revealed intraductal filling defects in two cases and kinks-stricture in one patient. On the other hand, normal findings were observed at MRCG in two of the three patients and ductal dilatation was found in the latter one. As intraductal papilloma was not reported for any patient on the histopathological examinations, the MRCG findings were thought to be true positives and the CG outcomes were false positives, and especially for the cases in which intraductal filling defects were observed.
In the present study, reaching consensus for 13 of 16 patients by using both modalities might hold promise for the future use of MRCG. However, limitations still exist such as the high cost and inaccessibility of MR imaging for all patients and medical centers. The inability to scan implanted patients who have implanted devices that are non-compatible with MR and the susceptibility for motion artifacts are the other possible limitations of MR imaging.
In conclusion, the results of this preliminary study suggest that MRCG seems a useful, safe procedure that can be employed as an alternative imaging modality for pathologic nipple discharge. However, statistically supported prospective studies with large populations in which CG, MRCG and MR galactography are compared are needed in the future.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download