Abstract
Objective
The purpose of this retrospective study was to report the outcome of the endovascular treatment of eight patients with eight saccular posterior inferior cerebellar artery (PICA) aneurysms.
Materials and Methods
Over the last seven years (1999-2006), eight consecutive patients with saccular PICA aneurysms were treated by endovascular methods. Five of the aneurysms were presented with subarachnoid hemorrhaging, whereas three were discovered incidentally. Four of the aneurysms (3 ruptured and 1 incidental) were treated by intrasaccular coiling, whereas the remaining four (1 ruptured and 3 incidental) were treated by vertebral artery (VA) occlusion.
Results
Of the four aneurysms treated by intrasaccular coiling, three were completely packed with coils and one was partially packed. In three of four patients who underwent vertebral artery occlusions, follow-up digital subtraction angiographies demonstrated thrombosed aneurysms and PICA. No procedure-related morbidity occurred and no re-bleed was encountered during a follow-up examination (mean; 31 months).
Posterior inferior cerebellar artery (PICA) aneurysms are rarely encountered, ranging in incidence between 0.5 and 3.0% of all occurring intracranial aneurysms (1-3). The PICA has the most complex and variable course of the cerebellar arteries, and previous studies have differentiated the segments of the PICA based on its relationships to the medulla oblongata and cerebellum (3-6). Aneurysms may arise from all segments of the PICA, with the majority originating from the vertebral artery (VA)-PICA junction and the proximal segments. The management of PICA aneurysms is challenging, in particular for the VA-PICA junction and the proximal segment aneurysms. Surgery is difficult because of the intimate relationship of the proximal PICA to the medulla and the lower cranial nerves (7, 8). The use of endovascular treatment as an alternative treatment has been increasing since it avoids the manipulation of important posterior fossa structures (5, 6, 9-13). The opportunity arose to treat eight patients with saccular PICA aneurysms by endovascular techniques, and our results were as follows.
We obtained institutional review board approval for the retrospective analysis of this study. Over the last seven years (1999-2006), we treated 256 patients with 271 cerebral aneurysms, by endovascular methods. Of these 256 patients, eight patients (7 female, 1 male; mean age, 53 years; age range, 26-65 years) had saccular PICA aneurysms and were the target of this research. Five of the eight aneurysms were found due to rupturing and three were found incidentally. Of the three incidental discoveries of PICAs, two patients had undergone a magnetic resonance imaging due to chronic headache and revealed an PICA aneurysm. The other incidental case was a patient who had a left posterior communicating artery aneurysm clipped at another hospital three years before, and a follow-up CT-angiography revealed an unruptured aneurysm. The locations of the PICA aneurysms were the VA-PICA junction in three patients, the anteromedullary segment in two, the lateromedullary segment in two, and the telovelotonsillary segment in one. Among the eight patients, four patients (3 ruptured and 1 incidental) underwent intrasaccular coiling with the Guglielmi detachable coils. The remaining four patients (2 unruptured and 2 incidental) had aneurysms which seemed difficult to treat by intrasaccular coiling without compromising the lumen of PICA; therefore, an occlusion of the vertebral artery proximal to the origin of PICA with detachable balloons (2 patients) or with coils (2 patients) was performed. The vertebral artery occlusion site was about 2 cm proximal to the origin of PICA in order to prevent the possible occlusion of the perforator to the brain stem (14).
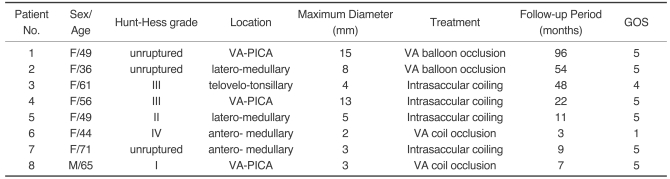
The patient characteristics are shown in Table 1. Of the four patients who underwent intrasaccular coiling, complete packing of the aneurysm with the coils was achieved in three patients (Fig. 1), whereas intentional subtotal packing was done in one case to preserve the parent artery due to a small wide neck aneurysm at the telovelotonsillary segment. The three patients who underwent VA occlusion with balloons, complete occlusion of the PICA as well as thrombosis of the aneurysm was confirmed on a follow-up digital subtraction angiography (DSA) performed between 3 and 14 months after the VA occlusion (Fig. 2). The distal segment of occluded PICA was reconstituted from the contralateral PICA and the proximal segment of occluded VA. The patients were not found to have any symptoms related to the occlusion of the PICA. In one patient who underwent a VA occlusion with coils, a follow-up CT-angiography performed three months later verified the occlusion of PICA and thrombosis of the aneurysm, however the female patient (patient 6) died of pneumonia soon after. No re-bleed occurred until she died, nor any complication related to the performed endovascular procedure. None of the patients experienced a re-bleed during a follow-up examination (mean, 31 months; range, 3-96 months).
The relatively rare incidence and proximity to the brain stem complicates the surgical management of PICA aneurysms. Additionally, an unfavorable relationship of the aneurysmal sac with the parent artery, which is often the case with PICA aneurysms, cause the surgical clipping or endovascular coiling procedures to be difficult and sometimes even impossible without sacrificing the PICA. Of the eight patients with PICA aneurysms in our series of examined patients, 4 (50%) were considered to be difficult for coiling. A deliberate occlusion of VA proximal to the origin of PICA was performed to reduce blood flow and pressure from the contralateral VA to the PICA and the aneurysm. Furthermore, a follow-up DSA confirmed the shrinkage of the aneurysm and ultimately the thrombosis of both the PICA and the aneurysm. In addition, the collateral reconstitution of the distal cortical branch was identified and all four of the patients with complicated PICA aneurysms had no symptoms related to the occlusion of the PICA. A deliberate VA occlusion has been used to treat vertebrobasilar artery aneurysms in a past study, Steinberg et al. (15), with an 86.5% excellent or good result by surgically ligating the VA to treat the unclippable vertebral artery aneurysms. Although the exact location of the VA aneurysm was not specified, the investigators observed that a unilateral VA occlusion could be an important therapeutic option for the treatment of a VA aneurysm. Groden et al. (16) also treated eight patients with fusiform or dissecting VA aneurysms by balloon occlusion of the VA. Their results indicated that one patient had an ischemic infarct at the region involved in the procedure. Occlusion of the VA for the treatment of a proximal PICA aneurysm arguably has some advantages compared to the occlusion of the PICA or the PICA and the aneurysm together. Namely, it could allow some time for the collaterals to the important perforators and cortical branches to be developed by decreasing the pressure and flow to the PICA. However, one important drawback is that it takes a long time for the aneurysms to be thrombosed, thus a substantial risk of rupture while waiting for the aneurysm to be thrombosed exists. Although three out of four aneurysms in our series showed complete thrombosis between 3 to 14 months after VA occlusion, Peluso at al. (17) reported that four PICA aneurysms treated by proximal VA occlusion did not thrombose during follow-up examination (up to 84 months later). Even so, the four aneurysms did not bleed during follow-up examinations, which is consistent with our findings. The potential risk of rupture should be kept in mind when the ruptured aneurysm is dissecting in nature, since the dissecting aneurysm has been known to have a higher risk for re-bleed (18). Maimon et al. (13) treated six patients with an isolated dissecting aneurysm of the PICA by occluding the aneurysm and PICA. Considering the high re-bleed rate and the associated high mortality rate, it seems reasonable to exclude the dissecting aneurysm as an early treatment of choice, however should remain as a possible subsequent treatment. Of the four patients, who underwent a VA occlusion in our series of patients, the discovery of an aneurysm in three of the patients was incidental. Although we were not completely sure that those aneurysms were not dissecting in nature, the saccular shape of aneurysms and the clinical history reduced the likelihood that the aneurysms were dissecting. Given the benign nature of the aneurysms found incidentally, we chose to treat them by minimally invasive techniques.
In our series, four patients underwent coil embolization of the aneurysmal sac with preservation of the parent artery. In three patients, the complete occlusion of the aneurysm neck was achieved. All three patients had a favorable aneurysm shape, which allowed for the uneventful coiling of the aneurysmal sac. In one patient who had a small aneurysm, at the telovelotonsillary segment, intentional subtotal packing with coils was performed, which preserved the PICA. Although this segment of the PICA is known to have no important perforators and could be sacrificed with little clinical consequences, the patient's neurologic status was so grave that we opted to treat the aneurysm less aggressively. Consistently, several other published studies have reported the successful intrasaccular coiling of a PICA aneurysm (5, 6, 9, 11, 12).
A PICA aneurysm could be missed if the whole segment of the PICA is not thoroughly visualized and examined on DSA. In our series, we failed to identify a small lateral medullary segment aneurysm, although, after a retrospective review, the aneurysm was briefly seen on the contralateral VA injection DSA. A repeat angiography, including both VA injections was performed two weeks later along with an ipsilateral VA injection which was non-dominant, to obtain two orthogonal views to show the aneurysm. A non-contrast enhanced CT showed the dilation of the lateral ventricle and some blood clots in the cisterna magna. The importance of both vertebral artery injections has been emphasized when an intraventricular clot and hydrocephalus is identified (3, 19). Blood in the cerebellopontine angle cistern, cisterna magna, and intracerebellar hemorrhage have been noted to be associated with the rupture of a PICA aneurysm.
In conclusion, our series of eight cases demonstrated the safety, feasibility and efficacy of the endovascular management of saccular PICA aneurysms.
References
1. Locksley HB. Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg. 1966; 25:219–239. PMID: 5911370.
2. Hudgins RJ, Day AL, Quisling RG, Rhoton AL Jr, Sypert GW, Garcia-Bengochea F. Aneurysms of the posterior inferior cerebellar artery. A clinical and anatomical analysis. J Neurosurg. 1983; 58:381–387. PMID: 6827323.
3. Lewis SB, Chang DJ, Peace DA, Lafrentz PJ, Day AL. Distal posterior inferior cerebellar artery aneurysms: clinical features and management. J Neurosurg. 2002; 97:756–766. PMID: 12405360.

4. Lister JR, Rhoton AL Jr, Matushima T, Peace DA. Microsurgical anatomy of the posterior inferior cerebellar artery. Neurosurgery. 1982; 10:170–199. PMID: 7070615.

5. Bradac GB, Bergui M. Endovascular treatment of the posterior inferior cerebellar artery aneurysms. Neuroradiology. 2004; 46:1006–1011. PMID: 15580490.

6. Mukonoweshuro W, Laitt RD, Hughes DG. Endovascular treatment of PICA aneurysms. Neuroradiology. 2003; 45:188–192. PMID: 12684724.

7. Horiuchi T, Tanaka Y, Hongo K, Nitta J, Kusano Y, Kobayashi S. Characteristics of distal posteroinferior cerebellar artery aneurysms. Neurosurgery. 2003; 53:589–596. PMID: 12943575.

8. Matsushima T, Matsukado K, Natori Y, Inamura T, Hitotsumatsu T, Fukui M. Surgery on a saccular vertebral artery-posterior inferior cerebellar artery aneurysm via the transcondylar fossa (supracondylar transjugular tubercle) approach or the transcondylar approach: surgical results and indications for using two different lateral skull base approaches. J Neurosurg. 2001; 95:268–274. PMID: 11780897.

9. Sandalcioglu IE, Wanke I, Schoch B, Gasser T, Regel JP, Doerfler A, et al. Endovascularly or surgically treated vertebral artery and posterior inferior cerebellar artery aneurysms: clinical analysis and results. Zentralbl Neurochir. 2005; 66:9–16. PMID: 15744623.

10. Lubicz B, Leclerc X, Gauvrit JY, Lejeune J, Pruvo JP. Endovascular treatment of peripheral cerebellar artery aneurysms. AJNR Am J Neuroradiol. 2003; 24:1208–1213. PMID: 12812956.
11. Mericle RA, Reig AS, Burry MV, Eskioglu E, Firment CS, Santra S. Endovascular surgery for proximal posterior inferior cerebellar artery aneurysms: an analysis of Glasgow Outcome Score by Hunt-Hess grades. Neurosurgery. 2006; 58:619–625. PMID: 16575325.

12. Ogilvy CS, Hoh BL, Singer RJ, Putman CM. Clinical and radiographic outcome in the management of posterior circulation aneurysms by use of direct surgical or endovascular techniques. Neurosurgery. 2002; 51:14–22. PMID: 12182412.

13. Maimon S, Saraf-Lavi E, Rappaport ZH, Bachar G. Endovascular treatment of isolated dissecting aneurysm of the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2006; 27:527–532. PMID: 16551989.
14. Grand W, Budny JL, Gibbons KJ, Sternau LL, Hopkins LN. Microvascular surgical anatomy of the vertebrobasilar junction. Neurosurgery. 1997; 40:1219–1225. PMID: 9179895.

15. Steinberg GK, Drake CG, Peerless SJ. Deliberate basilar or vertebral artery occlusion in the treatment of intracranial aneurysms. Immediate results and long-term outcome in 201 patients. J Neurosurg. 1993; 79:161–173. PMID: 8331396.
16. Groden C, Regelsberger J, Neumaier-Probst E, Grzyska U, Herrmann HD, Zeumer H. Operative or endovascular treatment of ruptured intracranial vertebral artery aneurysms? Neuroradiology. 2000; 42:685–691. PMID: 11071445.

17. Peluso JP, van Rooij WJ, Sluzewski M, Beute GN, Majoie CB. Posterior inferior cerebellar artery aneurysms: incidence, clinical presentation, and outcome of endovascular treatment. AJNR Am J Neuroradiol. 2008; 29:86–90. PMID: 17928380.

18. Yamamura I, Tani E, Yokota M, Nakano A, Fukami M, Kaba K, et al. Endovascular treatment of ruptured dissecting aneurysms aimed at occlusion of the dissected site by using Guglielmi detachable coils. J Neurosurg. 1999; 90:853–856. PMID: 10223450.
19. Kallmes DF, Lanzino G, Dix JE, Dion JE, Do H, Woodcock RJ, et al. Patterns of hemorrhage with ruptured posterior inferior cerebellar artery aneurysms: CT findings in 44 cases. AJR Am J Roentgenol. 1997; 169:1169–1171. PMID: 9308484.

Fig. 1
Complete packing of aneurysm.
A. Oblique projection of right vertebral digital subtraction angiography displaying small aneurysm at anterior medullary segment of posterior inferior cerebellar artery and microcatheter tip within aneurysm.
B. Complete packing of aneurysm was achieved with preservation of posterior inferior cerebellar artery.

Fig. 2
Vertebral artery occlusion for aneurysm management.
A. Sagittal T1-weighted MR image shows incidental aneurysm proximal to right lateral portion of medulla.
B. Right vertebral digital subtraction angiography shows saccular aneurysm at lateral medullary segment of posterior inferior cerebellar artery.
C. Left vertebral injection obtained immediately after proximal occlusion of right vertebral artery, in vicinity of posterior inferior cerebellar artery with detachable balloon reveals opacified right vertebral artery and posterior inferior cerebellar artery from left vertebral artery.
D. Follow-up digital subtraction angiography obtained 10 months after treatment shows slight decrease in size of aneurysm.
E. Follow-up digital subtraction angiography 14 months after treatment reveals complete thrombosis of posterior inferior cerebellar artery and aneurysm.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download