Abstract
The authors report two cases with distension of the obturator internus bursa identified on MR images, and describe the location and characteristic features of obturator internus bursitis; the "boomerang"-shaped fluid distension between the obturator internus tendon and the posterior grooved surface of the ischium.
About 20 types of bursae have been described around the hip and pelvic areas, with variable extents and prevalences (1). Although the locations and MR imaging features of a number of bursae, i.e., bursae of the iliopsoas (or iliopectineal bursa), trochanteric, and ischial (or ischio-gluteal bursa) have been well described (2-5), those of the obturator internus bursa have not been previously described. Here, the authors describe the locations and characteristic features of obturator internus bursa (Fig. 1).
A 28-year-old man presented with swelling and redness on the right inguinal and buttock area of two weeks duration. He also complained of intermittent fever and weakness in the right leg. Initial laboratory findings showed elevated ESR (66 mm/hr) and CRP (15.4 mg/dl) levels. MRI was performed to identify the infection focus and guide treatment planning, and showed a thin-walled fluid collection between the obturator internus tendon and the posterior surface of the ischium (Fig. 2A). The hip joint appeared normal. However, diffuse enhancement of soft tissue was noted in the right inguinal area, the lesser pelvis, and along the sciatic nerve. Diffuse pelvic infection with reactive bursitis of an obturator internus bursa was diagnosed based on clinical and MR imaging features. After eight days on antibiotics, his laboratory findings returned to the normal range, and follow-up MR 12 days later showed complete disappearance of the fluid pocket and of the soft tissue enhancement in the right pelvic area (Fig. 2B). He has since been asymptomatic.
A 33-year-old man was presented with a right buttock pain of two days duration, and had been febrile for two days, though this had been well controlled by antipyretics. A physical examination revealed tenderness, swelling, and local heating on the posterior region of the right buttock and paresthesia on the posterolateral aspect of his right leg. Pyriformis and Patrick tests were positive, and laboratory findings showed elevated ESR (27 mm/hr) and CRP (12.6 mg/dl) with mild leukocytosis (10,600/UI). MRI was performed under the impression of septic arthritis of the hip, and revealed a boomerang-shaped fluid collection over the posterior surface of the ischium, and diffuse enhancement of the obturator internus tendon and inferior gemellus muscle (Figs. 3A, B). An accompanying multidetector CT (MDCT) scan showed calcification along the obturator internus tendon (Fig. 3C). His symptoms also completely resolved after 21 days of antibiotic treatment.
A bursa is a sac lined with synovial cells that typically forms in an area of tendon friction. Recently, the MR imaging features of a number of uncommon bursae, such as, obturator externus bursa, subgluteus medius bursa, and subgluteus minimus bursa, have been described (4, 6).
The obturator internus muscle originates widely from the margin of the obturator foramen, obturator membrane, iliac bone, and the base of the ischial spine, and covers most of the lateral pelvic wall (7). It then passes through the lesser sciatic foramen, and finally, its fibers converge to form a tendon that inserts into the medial aspect of the greater trochanter of the femur, together with the tendons of the superior and inferior gemelli muscles (1). In more detail, the obturator internus tendon makes a right-angled bend over the grooved surface of the ischium, between the ischial spine and tuberosity, and then passes horizontally across the posterior to the hip joint before it inserts into the greater trochanter. Moreover, the obturator internus bursa is located between the obturator internus tendon and the grooved surface of the ischium (1).
A number of pathologic conditions involving the obturator internus muscle, tendon, or bursa have been described in the orthopedic literature (8-10), although no imaging findings of obturator internus bursitis have been described. In fact, Swezey (8) commented that obturator internus bursitis has been overlooked as a focus of myofascial irritability with lower back pain. Because patients with obturator internus bursitis have vague symptoms, such as, nonspecific myofacial irritability, fever, and buttock swelling, clinical diagnosis is made by direct palpation over the anatomical locus of the obturator internus bursa. When a patient is lying on one side with the affected knee drawn toward the chest, the obturator mternus bursa may be palpated superiorly from the ischial tuberosity. Several papers have described the clinical findings of obturator internus muscle abscesses in children, and haveemphasized the use of MRI and CT to confirm the diagnosis (9). Moreover, obturator internus muscle abscesses are frequently mistaken for septic arthritis of the hip joint, because of their similar clinical presentations. The MRI findings of obturator internus muscle abscesses are; muscle swelling and a rim-enhanced fluid pocket in or adjacent to the obturator internus muscle. These abscesses usually have a thick enhancing wall and a larger cavity than infected obturator internus bursa. In our cases, there was no evidence of septic arthritis, i.e., of joint effusion, synovial enhancement, or bone marrow signal changes in the hip joint. In one case report concerning obturator internus tendinitis, the patient was treated with a CT-guided injection of steroid and local anesthetic into the tendon sheath (10).
Normally, the obturator internus bursa is in a collapsed state, and is only distended and visualized by MRI when it is inflamed or infected. Fluid collection in the obturator internus bursa is caused by primary bursal infection or is associated with a pelvic infection. In the described cases, we were able to characterize the locations and shapes of obturator internal bursae on MR images. These bursae were visualized as narrow and elongated thin-walled fluid pockets resembling "boomerangs". The transverse plane provided best visualization, because the bursae were located parallel to the curved portion of the obturator internus tendon posterior to the ischium. Furthermore, fat-suppressed gadolinium-enhanced T1-weighted MR images nicely demonstrate these lesions.
In our cases, fluids within bursae were not drained. Nevertheless, the clinical and radiological improvements achieved by antibiotic treatment confirmed in both cases a diagnosis of obturator internus bursitis. The majority of patients with obturator internus bursitis or obturator internus muscle abscesses have been reported to respond adequately to antibiotics without surgical drainage (8, 9). Thus, knowledge of the MRI features of obturator internus bursitis can avoid unnecessary surgery.
In conclusion, a diagnosis of obturator internus bursitis should be considered when the "boomerang"-shaped fluid collection is observed between the obturator internus tendon and the posterior grooved surface of the ischium on MR images.
Figures and Tables
Fig. 1
Illustration showing anatomy of obturator internus bursa on posterior oblique (left) and left lateral pelvic CT views (right). GT = greater trochanter of femur, IS = ischial spine, I = ischium, SG = superior gemellus muscle and tendon, OI = obturator internus muscle and tendon, IG = inferior gemellus muscle and tendon, obturator internus bursa (red area)
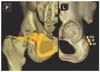
Fig. 2
28-year-old man with diffuse pelvic infection and reactive bursitis of obturator internus bursa.
A. Transverse fat-suppressed Gd-enhanced T1-weighted MR image shows fluid collection with enhanced thin peripheral rim (arrows) between ischium (I) and obturator internus muscle and tendon (arrowheads). Inflammation was also noted in right inguinal area, lesser pelvis, and along sciatic nerve.
B. Follow-up MR image 12 days later showing complete disappearance of fluid in obturator internus bursa and of soft tissue enhancement in right pelvic area.

Fig. 3
33-year-old male with calcific tendinitis of obturator internus tendon and infected bursitis.
A. Transverse fat-suppressed Gd-enhanced T1-weighted MR image showing boomerang-shaped obturator internus bursitis (arrows) between obturator internus muscle and posterior surface of ischium (I). Obturator internus tendon, inferior gemellus muscle, and soft tissue around sciatic nerve (arrowheads) show strong enhancement in this image.
B. Sagittal fat-suppressed Gd-enhanced T1-weighted MR image demonstrating location of obturator internus bursa (arrows), which lies anterior to obturator internus or inferior gemellus tendon (arrowheads) and posterior to ischium (I).
C. Transverse multidetector CT maximum intensity projection image showing high density in posterior aspect of right hip joint, which represented calcific tendinitis (arrows) along obturator internus tendon.

References
1. Williams A, Newell RL. Standring S, editor. Pelvic girdle, gluteal region and hip joint. Gray's Anatomy. 2005. 39th ed. Philadelphia: Elsevier;1447–1448.
2. Wunderbaldinger P, Bremer C, Schellenberger E, Cejna M, Turetschek K, Kainberger F. Imaging features of iliopsoas bursitis. Eur Radiol. 2002. 12:409–415.
3. Dunn T, Heller CA, McCarthy SW, Dos Remedios C. Anatomical study of the "trochanteric bursa". Clin Anat. 2003. 16:233–240.
4. Pfirrmann CW, Chung CB, Theumann NH, Trudell DJ, Resnick D. Greater trochanter of the hip: attachment of the abductor mechanism and a complex of three bursae-MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001. 221:469–477.
5. Cho KH, Lee SM, Lee YH, Suh KJ, Kim SM, Shin MJ, et al. Non-infectious ischiogluteal bursitis: MRI findings. Korean J Radiol. 2004. 5:280–286.
6. Robinson P, White LM, Agur A, Wunder J, Bell RS. Obturator externus bursa: anatomic origin and MR imaging features of pathologic involvement. Radiology. 2003. 228:230–234.
7. Shinohara H. Gemelli and obturator internus muscles: different heads of one muscle? Anat Rec. 1995. 243:145–150.
8. Swezey RL. Obturator internus bursitis: a common factor in low back pain. Orthopedics. 1993. 16:783–785.
9. Viani RM, Bromberg K, Bradley JS. Obturator internus muscle abscess in children: report of seven cases and review. Clin Infect Dis. 1999. 28:117–122.
10. Rohde RS, Ziran BH. Obturator internus tendinitis as a source of chronic hip pain. Orthopedics. 2003. 26:425–426.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download