Abstract
Objective
The aim of this study is to evaluate the reliability of MR imaging to predict the stability of the torn anterior cruciate ligament (ACL) after complete recovery of the ligament's continuity.
Materials and Methods
Twenty patients with 20 knee injuries (13 males and 7 females; age range, 20-54) were enrolled in the study. The inclusion criteria were a positive history of acute trauma, diagnosis of the ACL tear by both the physical examination and the MR imaging at the initial presentation, conservative treatment, complete recovery of the continuity of the ligament on the follow up (FU) MR images and availability of the KT-2000 measurements. Two radiologists, who worked in consensus, graded the MR findings with using a 3-point system for the signal intensity, sharpness, straightness and the thickness of the healed ligament. The insufficiency of ACL was categorized into three groups according to the KT-2000 measurements. The statistic correlations between the grades of the MR findings and the degrees of ACL insufficiency were analyzed using the Cochran-Mantel-Haenszel test (p < 0.05).
Results
The p-values for each category of the MR findings according to the different groups of the KT-2000 measurements were 0.9180 for the MR signal intensity, 1.0000 for sharpness, 0.5038 for straightness and 0.2950 for thickness of the ACL. The MR findings were not significantly different between the different KT-2000 groups.
Despite the poor healing of torn anterior cruciate ligaments (ACL) as compared with the medial collateral and posterior cruciate ligaments or menisci, the ACL also has a certain healing capacity, and it can regain its continuity after conservative treatment (1-4). A healed ACL shows well defined, normal-sized straight bands or hypointense comma-like tracts in its expected course on the MR images (2, 3). However, healing of the ligament implies formation of scar tissue at the site of the injury (5). Ligaments that looked intact on the MR imaging are associated with variable degrees of insufficiency in function, and some ligaments may require reconstruction surgery. However, to the best of our knowledge, there have been no reports evaluating the degree of stability of ACLs following complete rupture of the ligaments in spite of their intact appearance on the MR imaging. We performed instrumented measurement of the anterior laxity of the knee for testing the status of ACL with using a KT-2000 arthrometer. Normal subjects have a difference in the anterior displacement between the left knee and the right knee of no more than two millimeters, while patients with unilateral disruption of the ACL have a difference in the anterior displacement between the injured knee and the normal knee of more than two millimeters (6). We performed this study to correlate the MR findings of healed ACL injuries with the KT-2000 measurements in order to predict stability of the healed ACL by the MR findings.
We retrospectively reviewed the initial and follow up (FU) MR images of 92 patients' 92 knee joints from 1998 to 2004. The inclusion criteria for the study were : a positive history of acute recent trauma on presentation, diagnosis of ACL tear by both the physical examination and the MR imaging at the initial presentation, complete recovery of the ACL continuity on the FU MR images (Figs. 1, 2), and the availability of the KT-2000 measurements. Disruption of all the fibers revealed by the MR images, including both the obligue coronal and oblique sagittal scans along the course of ACL, was diagnosed as a complete tear of the ACL. There were neither avulsion injuries nor partial tears of the ACL, and no injuries to the contralateral knee joints. All of the injured knees were treated using a brace without reconstruction surgery; and each case was followed up by one experienced orthopaedic surgeon. Finally, twenty patients (13 males and 7 females, age range: 20-54 years, mean age: 32 years) with 20 knee injuries were selected for the review. Among them, arthroscopy was performed in eight patients due to the anterior instability of the knee joint (6/8), knee locking by the torn medial meniscus (1/8) and the knee joint contracture (1/8). The mean time interval between the FU MR and arthroscopy was 4 months 3 days ± 2 months 18 days (range 0-170 days). Our institutional review board approved this study protocol, and informed consents were not required from the patient.
The MR examinations were performed with a 1.5-T magnet (Signa; GE Medical Systems, Milwaukee, WI) using a quadrature knee coil with the following MR imaging protocols: the sagittal and coronal T2- and proton density-weighted (PDW) fast spin echo (FSE) images, the axial fat-saturated PDW FSE images and the oblique coronal and oblique sagittal PDW FSE images of the ACL. The oblique coronal and oblique sagittal images were obtained in the plane parallel to the course of the ACL. The parameters of the knee MR imaging were as follows: a TR/TE of 2000/20 (PDW image), a TR/TE of 2000/80 (T2-weighted image), 8-12 echo train length, 3-4-mm slice thickness, 1-mm interval, 256 × 192 matrix, 2 min 34 sec-3 min 28 sec scan time and a 14-cm field of view.
The mean time interval between the initial and the FU MR examinations was 7 months 18 days ± 6 months 14 days (range 25-790 days). Two musculoskeletal radiologists retrospectively reviewed the FU MR images by working in consensus. The evaluated MR findings were: signal intensity (SI), sharpness of the ligament contour, straightness of the ligament course and thickness of the healed ACL. These parameters were graded using a 3-point scale for the MR images, respectively, namely, homogeneous low SI, low SI spotted with high SI, heterogeneous or band-like high SI for SI; sharp, partly obscure or obscure for the sharpness of the ligament contour; straight, mild sagging or wavy, or severe wavy for straightness of the ligament course and normal, thick or thin for the thickness of the healed ACL. The SI of the ligaments was described as low when they appeared isointense or lower than that of muscles. The thickness of the ACL at the tibial attachment was used as a reference to determine the thickness of ACL at the torn portion.
The KT-2000 arthrometric laxity measurements (MEDmetric Corp., San Diego, CA) were used to evaluate the objective and quantitative stability of the injured ACL. One orthopedic surgeon who majored in sports medicine measured the difference in the KT-2000 displacement values between the injured and the normal knee joints with the knee in 30 degree flexion at an anterior load of 134 N for all of the subjects. This side-to-side difference was used as the KT-2000 measurement. The contralateral knee joints of the patients did not show any ACL laxity. The mean time interval between the FU MR and the KT-2000 results was 2 months 21 days ± 2 months 29 days (range: 1-189 days). We considered the KT-2000 results that were less than 3 mm as representing a stable ACL; those that measured more than 5 mm may suggest an insufficient ACL, and the patients may require reconstruction surgery. The patients were categorized into 3 groups according to the KT-2000 side-to-side differences: group 1, ≤ 3 mm (n = 11), group 2, 3-5 mm (n = 3) and group 3, > 5 mm (n = 6).
The results in respect of the grades according to the MR findings, and the groups, according to the KT-2000 laxity measurements, are summarized in Table 1. The ACL frequently showed an increased SI (heterogeneous or band-like high signal, 10/20, 50% or low SI spotted with a high signal area, 8/20, 40%) (Figs. 1C, D) and a partly obscure contour (9/20, 45%). The course of the ACL was straight (10/20, 50%) or mild sagging or wavy (9/20, 45%). The thickness of the healed ACL was relatively thick (10/20, 50%) or normal (7/20, 35%) (Figs. 2C, D).
Among the 20 patients reviewed in the study, arthroscopy was performed in eight patients. Five ligaments ( No. 1-5 in Table 1) were torn (complete tear, 4; partial tear, 1) and three (case No. 6, 7 and 8 in Table 1) were intact. Although statistic analyses were not performed, due to the small number of the subjects, the arthroscopically intact ligaments more frequently showed a normal thickness and a sharp contour of the ligament (2/3, 66%) as compared with the arthroscopically confirmed torn ligaments (0/5, 0%).
The p-values for each of the MR findings, according to the different groups of the KT-2000 measurements were 0.9180 for the SI of the ligaments, 1.0000 for the sharpness of the ligament contour, 0.5038 for the straightness of the ligament course and 0.2950 for the thickness of the ACL. There were no statistical differences between any of the MR findings in the different KT-2000 groups.
Primary healing of the ACL has been reported to be poor in both clinical and experimental studies (7-11). These inferior results have led to the preference for reconstruction of the ACL rather than conservative treatment, which involves bracing and muscle-strengthening exercises, after acute injury in athletic, active patients (12). However, the healing capability of a torn ACL has been reported on both experimentally and clinically (1-5, 7, 13). Arnoczky et al. (7) reported on the microvasculature of the cruciate ligaments and its response to injury in an experimental study on dogs. Periligamentous vessels forming the vascular synovial envelope around the ACL transversely penetrate the ligament and anastomose with the longitudinal network of the endoligamentous vessels. Healing starts from the surrounding soft tissues and also from the ligament or tendon itself. Regeneration is poor when there is little surrounding soft tissue available, as is the case in the ACL.
MR imaging is a diagnostic technique with a high sensitivity and specificity for the diagnosis of ACL lesions, be they either incomplete or complete tears (14, 15). The FU MR is needed to clarify the natural course of the meniscal lesions (16), meniscal repairs (17) and ACL reconstructions (18, 19). There is a report that the MR imaging may be a reliable method to use for evaluating the continuity and synovialisation of a torn ACL after it has healed (2).
Clinical studies have shown that the MR imaging could prove the capability of the ACL to heal naturally when early protective mobilization with a knee brace is used (2, 3). The MR imaging showed a bridging fibrous scar formation within the torn ligaments and synovialisation; this process can be suggested based on demonstrating comma-like hypointense fibrillar tracts that bridge the expected origin and insertion of the ACL (2). Ihara et al. (3) have reported that conservative treatment with early protective motion could result in well-defined large straight bands with a homogeneous low SI (21/50, 42%) or a low SI spotted with a high SI (16/50, 32%) on FU MR. The neoligament demonstrated a low SI on the PDW images and a gradual decrease with time of the SI of the substance of the ligaments. The investigators found significant relationships among the MRIs and the arthroscopic and stress radiographic evaluations, which appeared to correlate with clinically detectable successful ligament healing.
This study has established that FU MR examinations after conservative management demonstrated a healed ACL, well defined straight bands with heterogeneous SI or a low SI spotted with a high SI; these findings show a more prevalent heterogeneous SI than did the previous reports. There were nine cases (9/20, 45%), in which the restored continuity of the torn ACL that was revealed on FU MR actually did not result in sufficient stability. Five of them (5/20, 25%) required reconstructive surgery. It is well known that injury to a ligament results in a drastic change in its structure and physiology; this creates a situation that the ligament function is restored by the formation of scar tissue that is biologically and biomechanically inferior to the tissue it replaces (5). In one experimental study it has been reported that the mechanical and ultrastructural properties are not completely normal even one year after dissection of the ligament regardless of the treatment modality (7). The insufficiency of the healed ligaments observed in our study can be explained by these findings. Moreover, a high prevalence of radiographic osteoarthritis was reported 14 years after ACL disruption in soccer players (20). As shown in this report, ACL tears often have an influence on the knee stability. That is why we have to pay attention to the degree of insufficiency of the torn ACL.
Our study suggests that we could not distinguish between the insufficient and completely healed ACLs according to the MR findings. However, prior studies have not evaluated ligament insufficiency in healed ACL cases and they haven't produced the MRI findings that suggest laxity in a healed ACL. Resolution of these issues is complicated by the fact that we would not perform arthroscopy on clinically stable, healed ACLs. In some patients, KT-2000 arthrometric laxity measurements were used to objectively evaluate and quantify the stability of the injured ACL during FU MRI of the knee. Practically, we think this is the best way to evaluate the status of the torn ACL. There was a tendency that arthroscopically intact ligaments showed a normal thickness and a sharp contour of the ligament as compared with the arthroscopically confirmed torn ligaments, even though arthroscopy was done on a small number of patients. Although, this would need a further study, we expect that this finding may be of value when we have to manage a case of healed ACL in clinical practice.
Our study had several drawbacks. First, the population in our study was small. The subjects were chosen on the basis of the availability of the KT-2000 measurements, and many patients with FU MR were excluded due to the lack of the KT-2000 measurements. Second, we used the KT-2000 results as the gold standard because arthroscopy was not performed in many patients. There is no rationale for performing arthroscopy on patients with clinically stable ACL. Two patients, in whom the ACL was stable, underwent arthroscopy not for the evaluation of the ACL, but for meniscal repair or relief of contracture of the knee joint. Third, the time intervals between the initial and the FU MR examinations and that between the FU MR and KT-2000 examinations were somewhat long and variable. This limitation is associated with the retrospective nature of the study design. Fourth, we did not consider other associated injuries to the menisci, posterior cruciate ligament and collateral ligaments, which might have had an influence on healing of the ACL. However, the KT-2000 measurement may reflect the specific status of ACL, and other possible injuries might not significantly influence the KT-2000 results.
In conclusion, although healed ACL may demonstrate little signal abnormality or deformity on MR, the MR imaging itself is not reliable to predict the stability of the healed ACL after conservative treatment.
Figures and Tables
Fig. 1
A 25-year-old man with a completely healed anterior cruciate ligament that was confirmed by arthroscopy.
A, B. Oblique sagittal (A) and coronal (B) proton density-weighted images obtained on the day of the knee trauma show complete tear at the proximal anterior cruciate ligament and associated fracture at the lateral tibial plateau.
C, D. Follow up oblique sagittal (C) and coronal (D) images after four-months reveal a nearly normal-looking anterior cruciate ligament. The anterior cruciate ligament appears to show a low signal intensityspotted with a high signal intensity, a sharp contour, a straight course and a normal thickness. Arthroscopy performed 2-months later, due to contracture of the knee joint by the hypertrophy of ligamentum mucosum, demonstrated a normal appearance with normal tension of the anterior cruciate ligament. The side-toside difference of the KT-2000 measurement was 3 mm at the time of arthroscopy.

Fig. 2
A 54-year-old man with partial tear of anterior cruciate ligament that was confirmed by arthroscopy.
A, B. Sagittal (A) and oblique coronal (B) proton density-weighted images 15 days after the trauma show complete tear at the proximal anterior cruciate ligament and marrow contusion at the posterior aspect of the proximal tibia.
C, D. Four-months later, the sagittal (C) and oblique coronal (D) images demonstrate restored continuity of anterior cruciate ligament, which shows a band-like high signal intensity within the ligament, a partly obscure contour, mild sagging and an increased thickness. Partial tear of the anterior cruciate ligament was confirmed during arthroscopy 5-months later. The side-to-side difference of the KT-2000 measurement was 5 mm at the time of arthroscopy.

Table 1
Grades by MR Imaging and KT-2000 for Intact-Looking ACL after Rupture
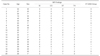
Note.-Abbreviations and grading: Grade 1-3 for each of the MR findings.
SI = signal intensity; homogeneous low SI / low SI spotted with high SI / heterogeneous or band-like high SI
CO = contour and sharpness; sharp / partly obscure / obscure
ST = straightness; straight / mild sagging or wavy / severe wavy
TH = thickness; normal / thick / thin
KT-2000 Group; Group 1 = KT-2000 side-to-side differences ≤ 3 mm; Group 2 = 3-5 mm; Group 3 = > 5 mm
References
1. Fujimoto E, Sumen Y, Ochi M, Ikuta Y. Spontaneous healing of acute anterior cruciate ligament (ACL) injuries - conservative treatment using an extension block soft brace without anterior stabilization. Arch Orthop Trauma Surg. 2002. 122:212–216.
2. Higueras Guerrero V, Torregrosa Andres A, Marti-Bonmati L, Casillas C, Sanfeliu M. Synovialisation of the torn anterior cruciate ligament of the knee: comparison between magnetic resonance and arthroscopy. Eur Radiol. 1999. 9:1796–1799.
3. Ihara H, Miwa M, Deya K, Torisu K. MRI of anterior cruciate ligament healing. J Comput Assist Tomogr. 1996. 20:317–321.
4. Malanga GA, Giradi J, Nadler SF. The spontaneous healing of a torn anterior cruciate ligament. Clin J Sport Med. 2001. 11:118–120.
5. Frank CB. Ligament structure, physiology and function. J Musculoskelet Neuronal Interact. 2004. 4:199–201.
6. Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R. Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am. 1985. 67:720–726.
7. Arnoczky SP, Rubin RM, Marshall JL. Microvasculature of the cruciate ligaments and its response to injury. An experimental study in dogs. J Bone Joint Surg Am. 1979. 61:1221–1229.
8. Bray RC, Leonard CA, Salo PT. Correlation of healing capacity with vascular response in the anterior cruciate and medial collateral ligaments of the rabbit. J Orthop Res. 2003. 21:1118–1123.
9. Andersson C, Odensten M, Good L, Gillquist J. Surgical or non-surgical treatment of acute rupture of the anterior cruciate ligament. A randomized study with long-term follow-up. J Bone Joint Surg Am. 1989. 71:965–974.
10. Hefti FL, Kress A, Fasel J, Morscher EW. Healing of the transected anterior cruciate ligament in the rabbit. J Bone Joint Surg Am. 1991. 73:373–383.
11. Noyes FR, Mooar PA, Matthews DS, Butler DL. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983. 65:154–162.
12. Noyes FR, Matthews DS, Mooar PA, Grood ES. The symptomatic anterior cruciate-deficient knee. Part II: the results of rehabilitation, activity modification, and counseling on functional disability. J Bone Joint Surg Am. 1983. 65:163–174.
13. Fujimoto E, Sumen Y, Deie M, Yasumoto M, Kobayashi K, Ochi M. Anterior cruciate ligament graft impingement against the posterior cruciate ligament: diagnosis using MRI plus three-dimensional reconstruction software. Magn Reson Imaging. 2004. 22:1125–1129.
14. Tung GA, Davis LM, Wiggins ME, Fadale PD. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993. 188:661–667.
15. Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J. Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology. 1988. 166:861–864.
16. Farley TE, Howell SM, Love KF, Wolfe RD, Neumann CH. Meniscal tears: MR and arthrographic findings after arthroscopic repair. Radiology. 1991. 180:517–522.
17. Steenbrugge F, Verstraete K, Verdonk R. Magnetic reasonance imaging of the surgically repaired meniscus: a 13-year follow-up study of 13 knees. Acta Orthop Scand. 2004. 75:323–327.
18. Yamato M, Yamagishi T. MRI of patellar tendon anterior cruciate ligament autografts. J Comput Assist Tomogr. 1992. 16:604–607.
19. Cheung Y, Magee TH, Rosenberg ZS, Rose DJ. MRI of anterior cruciate ligament reconstruction. J Comput Assist Tomogr. 1992. 16:134–137.
20. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004. 63:269–273.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download