Abstract
Objective
One of the best known side effects of using opium is spasm of the sphincter of Oddi, which may increase the diameter of the extrahepatic bile ducts. Ultrasound is the first imaging modality used for evaluating the biliary system because it is commonly available and noninvasive. The principal objective of this study was to measure the common bile duct (CBD) diameter via ultrasonography in opium addicts and to evaluate the relation between the CBD diameter and the period of addiction.
Materials and Methods
This research was an analytical-cross sectional study that was done on 110 opium addicts that were admitted to a drug treatment center. The diameter of the CBD in these cases was measured by ultrasonography and the results were analyzed with other factors like age, the period of addiction and the laboratory findings.
Results
According to the findings, there is a significant increase in the range of the CBD diameter in comparison with normal bile ducts. Also, the mean diameter of the CBD in the different age groups showed a significant difference (p < 0.0001) and there was a significant relation between the CBD diameter and the period of addiction (p < 0.001, r = 0.74); so, with the increased length of the addiction period, the mean CBD diameter increases.
Ultrasonography is the primary imaging modality for assessing the biliary ducts and it is commonly used as it is available, cheap and non-invasive. One of the findings that sonographers face when performing ultrasonography of the biliary ducts is the increased common bile duct (CBD) diameter as compared to its normal status. There are different etiologies for CBD dilatation such as CBD stones, tumor of the pancreatic head, tumors of Vater's ampula, masses and enlargement of the hilar lymph nodes of the liver. The etiology of obstruction may be found via ultrasonography if dilatation of CBD is due to mechanical obstruction, but when the etiology of obstruction is not obvious, more time and expense, further assessment and even invasive methods may be required in order to discover the etiology. For instance it may be necessary to use CT-scan, endoscopic retrograde cholangiopancreatography, percutaneous transhepatic cholangiography and even CBD exploration through surgical operation (1, 2).
On the other hand, spasm of the sphincter of Oddi is known as one of the important effects of opioids, and long term spasm of this sphincter in addicted individuals may consequently cause biliary stasis and dilatation of the CBD (3-6).
It is sometimes difficult to differentiate the pathologic dilatation of the CBD due to mechanical obstruction from its dilatation as the result of opioids consumption in addicted individuals. Although the normal diameter of the CBD in healthy individuals is listed in textbooks (2), the absence of a certain range and measurement for an increased CBD diameter in addicted individuals is one of the diagnostic problems when performing ultrasonography of their biliary ducts.
The main purpose of this study is to measure the changes of CBD diameter in opioid addicted people as compared to the normal status.
This analytic cross-sectional study was conducted on 110 opium-addicted individuals who were over 20 years old and they were referred to a drug treatment clinic in Rafsanjan from August to November in 2002. The Research Committee of Rafsanjan University of Medical Sciences approved our study and written informed content was obtained from all the participants in the study. The sample volume was determined through a pilot study on 8 addicted individuals and convenient nonrandomized sampling was then done.
The criteria for entering this study were as follows: the addicted individuals were above 20 years old and they without a history or the symptoms of biliary diseases, the results of their serum bilirubin and alkaline phosphatase tests were normal and they had no tumors, stones or any signs of biliary diseases on the ultrasonography of the liver, biliary ducts, gallbladder and pancreas.
Ultrasonography of the liver and biliary ducts was done, with the patients in a fasting state, by using a FUKUDA DENSHI CF-SONIC UF-7700 and a multi-frequency 3.5 MHz convex probe. Ultrasonographic measurements of the CBD diameter were done in the parasagittal plane and all of the examinations were done by a single sonographer.
According to the facts that the selected cases lacked the signs and symptoms of biliary obstruction and their serum bilirubin and alkaline phosphotase levels were normal and no signs signifying mechanical biliary obstruction were noticed on the sonographic findings, no further evaluation was done by a more invasive gold standard test to rule out obstruction.
The data gained through the ultrasonography, together with the age of the addicted individuals and the period of their addiction, was recorded on specific questionnaires and tables.
According to the information available in textbooks, the CBD diameter increases with age, so that its maximum diameter is 4 mm up to the age of 40, 5 mm at the age of 50 and it reaches 6 mm at 60 and increases after that in the same way (2); therefore, in order to control for age as a confounding factor, different age groups were classified and the relationship between the period of addiction and the diameter of the biliary ducts was determined for each group. The studied individuals were categorized into the age groups of 20-29, 30-39, 40-49, 50-59, 60-69 and above 70 years old.
One-way analysis of variance (ANOVA) tests were used to compare the average diameter of the CBD in different age groups. Tukey-Kramer multiple comparison tests were used for double comparisons. Pearson's correlation coefficient was also used to determine the relationship between the period of addiction and the diameter of the biliary ducts. P < 0.05 was considered significant for each of the mentioned tests. The data were analyzed by INSTAT statistical software (GraphPad Software Inc., San Diego, CA)
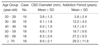
Table 1 shows some statistical indices of the assessed parameters for different age groups of the addicted individuals who were referred to the addiction clinic. As shown in the table, the average diameter of the CBD increases with age; a diameter of 3.8 mm in the 20-29-years-old group reaches 8.9 mm in the above 70-year-old group. The average diameter of the CBD was compared amongst the different age groups using the one-way ANOVA test and a significant difference was found between the average diameters of the CBD of the various age groups (F = 15.362, p < 0.0001). Using the Tukey-Kremer multiple comparison test, we found that that CBD average diameter of the 20-29-year-old group was significantly less than that of the other age groups and the average diameter of the CBD in the individuals above 70-years-old was more than that of all the other groups except for the 60-69-year-old group; this indicates the significant increase of the CBD average diameter with the age of the opium-addicted individuals.
Table 2 shows the association of the CBD diameter and years of addiction in each age group. The correlation coefficient of the CBD diameter and the years of addiction was 0.74 (95% CI: 0.64-0.81) for all the cases, which shows a significant relationship (p < 0.001); so, as the years of addiction increase, the CBD diameter tends to dilate.
On the hand, compared with the indicated normal range, 65.5% of the total individuals suffered from CBD dilatation and the indices for the different age groups of 20-29, 30-39, 40-49, 50-59, 60-69 and 70-years-old and above were 36.8%, 89.5%, 66.7%, 61.1%, 72.2% and 61.1%, respectively.
The CBD diameter has been specified in ultrasonography textbooks and the present information shows that the CBD diameter increases with age. The results of the present study show that in all the age groups, the CBD diameter has a wider range in the addicted individuals compared to the normal diameter. Also, according to the obtained results, the CBD diameter is significantly different amongst the age groups and it shows the significant increase of CBD diameter with age for the opium-addicted individuals. The correlation coefficient of the CBD diameter and the years of addiction is r = 0.74 for all 110 assessed cases, and this shows the significant increase of CBD diameter with the increase of the years of addiction.
In a previous study by Zylberberg et al. (7) 36 patients with hepatitis-C and who consumed Methadone or Bupernorphine at the same time were assessed. Amongst these patients, three cases (8.3%) showed dilatation of their biliary ducts on ultrasonography (CBD ≥ 9 mm) without mechanical obstruction. They also assessed, via sonography, 298 patients with hepatitis-C who didn't take narcotics, and they found just one case with biliary duct dilatation (0.03%) (p < 0.001). They also suggested that taking narcotics might lead to dilatation of the biliary ducts, and this doesn't need invasive diagnostic assessment (7).
In another study done by Berezny et al. (1) with using ultrasonography, they showed a case of increased CBD diameter due to codeine consumption and they recommended using ultrasound as a useful method for the assessment of the CBD diameter changes in order to diagnose spasm of the sphincter of Oddi.
CBD dilatation in addicted individuals is due to the effects of morphine on Oddi's sphincter. A study performed in 2004 showed that morphine causes an increase of the basic pressure and the range and the frequency of phasic contractions of the sphincter of Oddi, but it has no effects on the length of period of phasic contraction. The combination of these effects leads to increased CBD internal pressure and so its dilatation (8). These acute effects of morphine on Oddi's sphincter vanish when prescribing Atropine or Hyoscine (9); However, in the addicted individuals exposed to morphine for a long time, the indicated effects lead to permanent dysfunction of Oddi's sphincter, dilatation of biliary ducts and biliary colic, and endoscopic sphinterotomy results in considerable improvement of the symptoms (10). However, it should be remembered that all narcotics increase the internal pressure of biliary ducts, but the biggest increase is with morphine (11). Delayed transit of radioactive substances in the biliary ducts after prescribing morphine during NHI (nuclear hepatobiliary imaging) imitates that signs similar to pathologic obstruction should be indications for performing NHI in addicted individuals (12).
In this study, a strong, significant association was found between the increase of CBD diameter and addiction to opioids, so that with more years of addiction, the CBD diameter is more dilated. So, we suggest that there is no need for additional or invasive diagnostic methods for opium-addicted individuals with a dilated CBD discovered by ultrasonography, and these individuals are without any signs of obstruction in the biliary ducts, and their levels of serum alkaline phosphatase and bilirubin are normal at the same time. However, since the number of cases in this study was small and any gold standard diagnostic method was not used, more extended research is recommended to confirm our findings.
Figures and Tables
References
1. Berezny GM, Beck IT, DaCosta LR, O'Brien PG, Paloschi GB. Ultrasound in the diagnosis of sphincter of Oddi spasm. J Clin Gastroenterol. 1985. 7:528–532.
2. Rumack CM, Wilson SR, Charboneau JW. Diagnostic ultrasound. 1988. 2nd ed. St. Louis: Mosby;207.
3. Katznug BG. Basic & Clinical pharmacology. 2001. 8th ed. New York: McGraw-Hill;521.
4. Hardman JG, Limbird LE. Goodman & Gilman's the pharmacological basis of therapeutics. 2001. 10th ed. New York: McGraw-Hill;585.
5. Kaihlenen PM. The complete drug reference. 1999. 32nd ed. Boston: Pharmaceutical Press;68.
6. Butler KC, Selden B, Pollack CV Jr. Relief by naloxone of morphine-induced spasm of the sphincter of Oddi in a post-cholecystectomy patient. J Emerg Med. 2001. 21:129–131.
7. Zylberberg H, Fontaine H, Correas JM, Carnot F, Brechot C, Pol S. Dilated bile duct in patients receiving narcotic substitution: an early report. J Clin Gastroenterol. 2000. 31:159–161.
8. Wu SD, Zhang ZH, Jin JZ, Kong J, Wang W, Zhang Q, et al. Effect of narcotic analgesic drugs on human Oddi's sphincter motility. World J Gastroenterol. 2004. 10:2901–2904.
9. Wu SD, Kong J, Wang W, Zhang Q, Jin JZ. Effect of morphin and M-cholinoceptor bloching drugs on human sphincter of Oddi during choledochofiberoscopy manometry. Hepatobiliary Pancreat Dis Int. 2003. 2:121–125.
10. Sharma SS. Sphincter of Oddi dysfunction in patients addicted to opium: an unrecognized entity. Gastrointest Endosc. 2002. 55:427–430.
11. Thompson DR. Narcotic analgesic effects on the sphincter of Oddi: a review of the data and therapeutic implications in treating pancreatitis. Am J Gastroenterol. 2001. 96:1266–1272.
12. Barlas D, Margouleff D, Vignogna-Barlas L, Lesser ML. Opioids prolong nuclear hepatobiliary imaging when given prior to scaning. J Emerg Med. 2002. 23:231–236.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download