Abstract
Interstitial ectopic pregnancy is a rare condition of pregnancy and may be very dangerous if not identified and treated urgently. We report a case of successful treatment of an interstitial pregnancy using selective uterine artery embolization. A 27-year-old woman with interstitial pregnancy was treated by uterine artery embolization after failure of systemic methotrexate treatment. Her serum beta-human chorionic gonadotropin (β-hCG) was undetectable one month after the therapeutic embolization and transvaginal sonography 31 days after embolization showed normal endometrium and cornu. The patient achieved a normal pregnancy eight months after embolization.
Interstitial pregnancy is defined as any gestation that develops in the uterine portion of the fallopian tubes lateral to the round ligament. Interstitial pregnancies account for 2-4% of all ectopic pregnancies and have been reported to have an associated 2% to 2.5% maternal mortality rate (1).
The traditional treatment for interstitial pregnancy using surgical cornual resection may cause infertility or uterine rupture in subsequent pregnancies. Recently, the early identification of intact interstitial pregnancy has been made possible in many cases with high resolution transvaginal ultrasound as well as more sensitive assays for beta-human chorionic gonadotropin (β-hCG). The treatment includes: hysteroscopic transcervical currettage, local and systemic methotrexate (MTX) therapy and prostaglandin or potassium chloride injection of the ectopic mass under sonographic guidance (2).
We describe a case of successful treatment of interstitial pregnancy using uterine artery embolization, after failure of methotrexate treatment.
A 27-year-old woman, gravida 2, para 0, was referred to the gynecology department at our institution with a history of seven week amenorrhea and slight vaginal bleeding of two day duration.
Her menses had been regular, every 28-30 days. The patient had no history of pelvic inflammatory disease, intrauterine device use, abdominal surgery, or treatment for induction of ovulation. Her obstetrical history was significant for no normal delivery and two early spontaneous miscarriages. Upon examination in the delivery room the patient's vital signs were stable and the general physical examination was unremarkable. Transvaginal sonogram demonstrated the presence of a gestational sac (2.2×2.6 cm in diameter) with a fetal heart beat surrounded by an asymmetric myometrial mantle in the outer right margin of the uterus, which raised suspicion for an interstitial pregnancy (Fig. 1A).
The patient's serum values were: β-hCG 23,285 mIU/mL 1 day before admission and increased to 29,454 mIU/mL on the day of admission. Treatment was started with 1.0 mg/kg (body weight: 53 kg) MTX intramuscularly on the same day of admission. The β-hCG increased to 35,654 mIU/mL on the 2nd day of admission. If the MTX therapy is successful, the β-hCG level is expected to drop immediately. However, the serum β-hCG levels were not decreased in this patient; therefore, we thought that the MTX therapy was not effective. We decided to attempt surgical treatment. However, the patient wanted to avoid surgical intervention. We decided to proceed with uterine artery embolization on the second day of admission.
The institutional review board approved the procedure and the patient provided written informed consent prior to the procedure. In the angiography room, under local anesthesia, a 5-Fr catheter was advanced through the sheath introducer inserted from the right common femoral artery and was positioned in the right internal iliac artery. Next, a 2.8-Fr microcatheter (Progreat, Terumo, Tokyo, Japan) was coaxially advanced into the right uterine artery from the 5-Fr catheter with use of a microguidewire (GT wire, Terumo, Tokyo, Japan); selective uterine arteriography was performed and showed increased vascularity in the cornu region (Fig. 1B). The microcatheter was then further advanced into the ascending portion of uterine artery. Embolization was achieved using PVA particles (Coutour, Boston Scientific, Cork., Ireland) of 500-710 µm until a standing column of contrast was obtained; this signified the occlusion of the ascending portion of the uterine artery with a preserved cervicovaginal branch (Fig. 1C). The left internal iliac artery was selected, and the same technique was used to embolize the left uterine artery; embolic material was used with gelfoam.
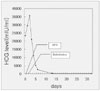
The serum β-hCG level decreased to 21,149 mIU/mL on the second day and 2,627 mIU/mL on the fifth day after the procedure. The patient had no complications such as pain, fever or infection. The patient was discharged in good condition six days after the procedure. The serum β-hCG level decreased to 188 mIU/mL 11 days later and was undetectable one month after the procedure (Fig. 2).
Ultrasonography examination demonstrated a collapsed gestational sac with a normal endometrial stripe one month after the procedure (Fig. 1D). The patient had an unremarkable gynecologic examination. Spontaneous menstruation occurred five weeks after the procedure. Eight months after embolizaton, the patient was pregnant. Transabdominal ultrasonography demonstrated an intrauterine gestation sac with a fetal heart beat (Fig. 1E).
Interstitial pregnancy is a rare form of ectopic pregnancy and has a maternal mortality rate as high as 2% to 3%, which is twice that of other tubal gestations (1).
The exact pathogenesis of this type of gestation is unknown; however, it is thought to be associated with abnormal transportation of the fertilized ovum within the fallopian tube. Similar to other ectopic pregnancies, risk factors include: a history of pelvic inflammatory disease, intrauterine device and previous tubal surgery. In particular, patients with ipsilateral salpingectomy or cornual reanastomosis appear to have specific risk for interstitial pregnancies (3).
Cornual resection by laparotomy or via laparoscopy have been used for treatment of interstitial pregnancies may cause problems of reduced fertility by blocking the cornu or subsequent pregnancy related uterine rupture resulting from weakening the uterine wall. Vascular supply of the interstitial area is particularly rich and the gestational sac of interstitial pregnancy is in a highly vascular area, near the anastomosis of the uterine and ovarian vessels. A surgical procedure, in the interstitial area, may result in a catastrophic hemorrhage. For this reason, other surgical treatments such as: laparoscopy guided transcervical curettage, laparoscopic cornuostomy, hysteroscopic gestational sac removal as well as medical treatments such as: local or systemic methotrexate therapy, prostaglandin or potassium chloride injection of the ectopic mass under sonographic or laparoscopic guidance have been used for treatment (4, 5). MTX therapy has become a popular approach for treatment of ectopic pregnancy; however, drug toxicity (dermatitis, alopecia areata, vomiting), hemorrhage necessitating emergency surgery and potential risk of rupture of ectopic pregnancy are serious associated complications.
Uterine artery embolization is a procedure becoming increasingly popular in obstetrics or gynecologic used for bleeding, uterine myoma and in uterine vascular malformations. It can be used as an alternative method for surgical treatment or in association with surgery to prevent major bleeding.
Recently Ophir et al. (6) and Deruelle et al. (7) have described successful treatment of interstitial ectopic pregnancy by selective uterine artery embolization without any serious complications. The uterine cornu area is a highly vascular region near the anastomosis of the uterine and ovarian vessels; however, the majority of the vascular supply in the cornu area is from the uterine artery. Therefore, the block of blood flow in the uterine artery may decrease vascularization of a pregnancy, leading to trophoblastic degeneration affecting placental function and fetal growth. In our case, we used PVA particles at the lesional side for a more compact vascular block, and used gelfoam, which is a temporary occlusion of vessels for two to six weeks, at the contralateral side for blocking only the retrograde collateral blood supply. These previously reported cases, as well as ours, demonstrate that selective uterine artery embolization could be a safe and effective treatment for the conservative management of interstitial ectopic pregnancy.
The effect of the embolization on menses and subsequent pregnancies remains unclear; however, there have been many cases reported of successful pregnancy after uterine fibroid embolization (8-10); Deruelle et al. (9) reported a subsequent pregnancy after uterine artery embolization in a patient with an interstitial ectopic pregnancy. In addition, Tropeano et al. (10) reported that the use of uterine fibroid embolization in women younger than 40 had no definite change on the ovarian reserve. In our case, eight months after the, uterine artery embolization (UAE) a subsequent pregnancy was achieved; thus the successful outcome of our case suggests that this procedure may preserve fertility in cases with early detection of unruptured interstitial pregnancy.
The other possible complications after UAE are pain, groin hematoma, uterine necrosis and pelvic infection such as tuboovarian abscess and endometritis; our case, had no complications after the procedure.
In conclusion, selective uterine artery embolization for interstitial ectopic pregnancy is a safe and effective alternative to surgical treatment and may preserve future fertility.
Figures and Tables
Fig. 1
Selective uterine artery embolization in a 27-year-old woman with interstitial ectopic pregnancy.
A. Axial image from the abdominal ultrasonogram reveals an ectopic gestational sac (arrows) in the interstitial portion of the right fallopian tube.
B. Right uterine artery angiogram shows increased vascularity in the right uterine cornu.
C. Right uterine artery angiogram after embolization shows complete occlusion of the ascending portion (arrow) of the uterine artery.
D. One month after embolization, sagital (left) and axial (right) images of the transvaginal ultrasonogram reveal normal endometrial stripe and cornu regions.
E. Eight months after emblization, the oblique sagittal image of the abdominal ultrasonogram demonstrates an eight week intrauterine pregnancy with a fetal heart beat.

References
1. Rock JA, Damario MA. Rock JA, Thompson JD, editors. Ectopic pregnancy. TeLinde's operative gynecology. 1997. 8th ed. Philadelphia: Lippincott-Raven;505–520.
2. Oelsner G, Admon D, Shalev E, Shalev Y, Kukia E, Mashiach S. A new approach for the treatment of interstitial pregnancy. Fertil Steril. 1993. 59:924–925.
3. Advincula AP, Senapati S. Interstitial pregnancy. Fertil Steril. 2004. 82:1660–1661.
4. Zhang X, Liu X, Fan H. Interstitial pregnancy and transcervical curettage. Obstet Gynecol. 2004. 104:1193–1195.
5. Katz DL, Barrett JP, Sanfilippo JS, Badway DM. Combined hysteroscopy and laparoscopy in treatment of interstitial pregnancy. Am J Obstet Gynecol. 2003. 188:1113–1114.
6. Ophir E, Singer-Jordan J, Oettinger M, Odeh M, Tendler R, Feldman Y, et al. Uterine artery embolization for management of interstitial twin ectopic pregnancy: case report. Hum Reprod. 2004. 19:1774–1777.
7. Deruelle P, Lucot JP, Lions C, Robert Y. Management of interstitial pregnancy using selective uterine artery embolization. Obstet Gynecol. 2005. 106:1165–1167.
8. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002. 109:1262–1272.
9. Deruelle P, Closset E. Management of interstitial pregnancy using selective uterine artery embolization. Obstet Gynecol. 2006. 107:427–428.
10. Tropeano G, Di Stasi C, Litwicka K, Romano D, Draisci G, Mancuso S. Uterine artery embolization for fibroids does not have adverse effects on ovarian reserve in regularly clycling women younger than 40 years. Fertil Steril. 2004. 81:1055–1061.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download