Abstract
Objective
To assess the efficacy and safety of a "mini-perc" technique of percutaneous nephrolithotomy using a 14-Fr peel-away sheath for the removal of pyelocaliceal stones, and to determine appropriate inclusion criteria.
Materials and Methods
From July 1999 to June 2002, the medical records and radiographic images of 72 patients who underwent the "mini-perc" technique of percutaneous nephrolithotomy with a 14-Fr peel-away sheath, were reviewed to determine clinical history, stone characteristics, immediate stone free rate, final stone free rate after additional procedures, complications, and hospital stay. We also analyzed the effect of the longest stone diameter, the cumulative longest diameter of stones, the cumulative stone burden, and the stone density on the immediate stone free rate using a Fisher exact test.
Results
The only major complication, arterial bleeding, occurred in a patient with Child A liver cirrhosis and was successfully treated by embolization with coils and a gelatin sponge. The immediate stone free rate was 80.6%, which was significantly influenced by stone diameter but not stone density. The mean hospital stay after the procedure was 3.97 days.
In the early 1980's, percutaneous nephrolithotomy replaced open surgery in a majority of renal stone treatments (1). However, it is frequently regarded as a second-line therapy for several reasons, including procedure-related hemorrhages requiring a blood transfusion or intervention (2-5), a greater demand for postoperative parenteral pain medication, and a longer hospital stay (6).
To reduce the disadvantages of conventional percutaneous nephrolithotomy, a "mini-perc" technique was first developed for children and reported by Helal et al. (7). Additionally, Jackman et al. (8, 9) defined the "mini-perc" as a percutaneous nephrolithotomy achieved through a sheath too small to accommodate a standard rigid nephroscope. Other studies also described this technique as an effective and safe procedure (10-12). However, there have been no follow-up reports of experiences in a larger series.
The purpose of this study was to assess the safety and effectiveness of using a 14-Fr peel-away sheath for the removal of pyelocaliceal stones by reviewing our experience, as well as to determine the appropriate inclusion criteria.
During the 3-year period from July 1999 to June 2002, the "mini-perc" technique of percutaneous nephrolithotomy on pyelocaliceal stones was performed in 72 consecutive patients at our hospital. This study was approved by the Institutional Review Board, and written informed consent was obtained from each patient or their family members at the time of enrollment in the study, after the nature of the procedure and possible complications had been fully explained. There were 27 women and 45 men, and the age range was 1.4 years to 73 years (mean age, 49.5 years ± 14.7). The indications included failed shock wave lithotripsy and/or ureteroscopy in 19 subjects, a large cumulative stone burden (> 6 cm2) in 25, renal pelvis and/or lower pole calyceal stones in 62, upper calyceal stones in two, stone in calyceal diverticulum in one, and one child. Thirty-one of 72 patients had more than two of these indications.
Medical records of each patient were reviewed to determine the duration of symptoms, previous medical history, pre- and post-"mini-perc" interventional procedures, and hospital stay after the "mini-perc". Radiologic examinations were also reviewed in all patients, including abdominal radiography, intravenous urography, antegrade pyelography, renal ultrasound, abdominal computed tomography, and abdominal magnetic resonance imaging.
Data on the stone number, location, longest stone diameter, the cumulative longest diameter of stones, cumulative stone burden, and stone density were also determined on a preoperative plain abdominal radiograph. The stone burden was defined as the two-dimensional area determined by multiplying the length by the width of the stone. Stone density was graded on three levels based on comparison with the adjacent rib (3: more dense, 2: isodense, 1: less dense). Postoperative evaluation of residual stones was done radiologically and nephroscopically. The immediate stone-free rate, complications after the "mini-perc", and final stone-free rate after additional procedures were determined. We also assessed the effect of the longest stone diameter, the cumulative longest diameter, cumulative stone burden, and stone density on the immediate stone-free rate.
Routine percutaneous renal access was performed in the interventional radiology suite on the day or one day prior to the planned "mini-perc". Local anesthesia was used at the puncture site with the exception of a 17-month-old boy, who underwent general anesthesia (Fig. 1). The definitive puncture was performed into the appropriate calyx with a 22-gauge Chiba needle (Cook, Bloomington, IL) under real-time ultrasound and fluoroscopic guidance. The approach most commonly was done through a lower pole calyx, or the postero-inferior aspect of the renal stones (Fig. 1D). The nephrostomy was created in an upper pole calyx in two patients who had upper calyceal stones. A 0.035-inch Radifocus guide wire (Terumo, Tokyo, Japan) was advanced through the nephrostomy tract into the bladder as a safety guide wire. An Amplatz Super Stiff guide wire (Boston Scientific, Miami, FL) was inserted into the bladder as a working guide wire (Fig. 1E). Nephrostomy tract dilation was then performed to the 14 Fr with serial dilators (Cook, Bloomington, IL), a 14-Fr peel-away sheath (Cook, Bloomington, IL) (Fig. 2) was advanced through the working guide wire.
One urologist (S.S.J), who had 8-years of experience in urology and had started using the "mini-perc" in 1998, utilized the 8/9.8 Fr rigid ureteroscope with the Coherent Ho: YAG laser lithotrite (Coherent medical group, New York, NY; 365 µm or 550 µm fiber, 10 to 20 Hz frequency, 0.5 to 1 J power). Small fragmented stones were then extracted by suction, an N-circle tipless basket (Cook Urological, Spencer, IA), and three-pronged grasping forceps (Cook Urological, Spencer, IA).
A 14-Fr Malecot nephrostomy catheter (Cook, Bloomington, IL) was routinely left in the renal pelvis upon the completion of the procedure, and was removed within 48 hours. Imaging studies were not obtained prior to the nephrostomy tube removal, unless intraoperative findings suggested significant extravasation or residual calculi. Otherwise, nephrostomy tubes were clamped when the urine was clear and removed two hours later unless the patient reported flank pain.
The mean duration of the symptomatic period was 19.5 months ± 51.1 (range, 0.5-360 months) in 57 of 72 patients. Fifteen patients were asymptomatic, and one of them was incidentally identified during work-up of cervical cancer. Previous renal or ureter stones in another location was present in 28 subjects, and urinary tract infections were found in four subjects. Previous interventional procedures included shock wave lithotripsy in 19 subjects, laparoscopic or open ureterolithotomy in five, traditional percutaneous nephrolithotomy in one and vesicolithotripsy in one.
The mean total hospital stay was 7.68 days ± 3.21 (range 4-22 days). On average, the hospital stay after the "mini-perc" was 3.97 ± 2.72 (range, 1-13 days).
Fifty-seven percent of the patients (41 of 72) had stones in the left kidney, and 43% (31 of 72) in the right kidney. The total number of calculi was 89, with 40 of the renal pelvis, 29 of the lower calyx, eight of the upper calyx, four of the middle calyx, and eight of staghorn stones. The mean number of calculi per patient was 1.44 ± 0.82 (range 1-5). The mean value of the longest diameter was 2.83 cm ± 1.61 (range, 0.3-8.9 cm), and that of the cumulative longest diameter was 3.42 cm ± 1.99 (range, 0.6-10.2 cm). The mean value of the cumulative stone burden was 7.18 cm2 ± 7.93 (range, 0.24-39.5 cm2). Stone densities 1 and 2 were observed in five and 26 patients, respectively. The remaining 41 patients had more dense stones than the adjacent rib density.
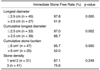
In no case was it necessary to convert from the "mini-perc" to conventional percutaneous nephrolithotomy. The immediate stone-free rate was 80.6% (58 of 72 patients). The total number of residual fragments was 21 (mean, 1.5 ± 0.65, range, 1-3) in 14 patients. The location was as follows: seven in the lower calyx, six in the upper calyx, and four in the middle calyx. The remaining four were staghorn stones. The longest diameter, the cumulative longest diameter, and the cumulative stone burden affected the probability of the immediate stone-free rate (Table 1). The immediate stone-free rate was significantly higher in patients with a longest stone diameter of less than 2.5 cm or a cumulative stone burden of less than 6 cm2. However, there were no statistically significant differences in stone density (Table 1).
The only major complication was hemorrhage, which occurred in one (1.4%) of 72 patients who was diagnosed previously with Child A liver cirrhosis. Arteriography revealed a contrast extravasation from the arcuate artery of the kidney (Figs. 3A, B). After embolization with a coil and gelatin sponge, no further bleeding occurred (Fig. 3C). Other serious complications such as injury to neighboring organs (lung, intestine, liver, and spleen) or loss of a kidney did not occur.
Mild fever occurred in seven (9.7%) of the 72 patients, which subsided spontaneously within one day. Fever due to toxic hepatitis occurred as a postoperative complication in one patient (1.4%). Oozing at the puncture site occurred in two patients (2.8%) and abdominal paralytic ileus in another two (2.8%).
Additional procedures after the "mini-perc" were performed in 11 (15.3%) of 72 patients, including extraction of the smallest residual stone fragments. There were shock wave lithotripsy in nine, shock wave lithotripsy and conventional nephrolithotomy in one, and ureteroscopy in one. After additional procedures, the final stone-free rate was 87.5% (63 of 72).
The mean follow-up time was 7.23 months ± 8.29 (range, 0.5-37 months). The final follow-up modality was KUB (kidney, ureter, and bladder) in 44 patients, IVP (intravenous pyelogram) in 24, US in three and CT in one. These images were used to establish that two (3.2%) of 63 patients were finally stone-free.
Percutaneous nephrolithotomy, with its introduction in 1976, is a well-established technique for the treatment of large renal calculi, and is performed either alone or in conjunction with extracorporeal shock wave lithotripsy (13-15). The disadvantages of extracorporeal shock wave lithotripsy are overcome by percutaneous nephrolithotomy, which has higher stone-free rates, shorter treatment times, and a reduced risk of febrile infection of the urinary tract (14, 16-18). Nevertheless, the main risk of percutaneous stone therapy is hemorrhaging that requires a blood transfusion 11-14% of the time, and an increased risk of kidney loss (14, 15). Therefore, conventional percutaneous nephrolithotomy is not justified as the primary form of urinary stone treatment for smaller lower pole concrements, although it is recommended as an effective method in children (19).
Traditional percutaneous nephrolithotomy uses a 30-Fr nephrostomy sheath for renal access. The recent development of smaller sheaths suggested that percutaneous nephrostomy tract formation can be performed with minimal damage to the involved renal parenchyma, thereby reducing the procedure-related morbidity without diminishing its therapeutic efficacy (1, 7-12). The use of the 15-Fr Hickman peel-away sheath was described by Helal et al. (7) as the first development of minimally invasive percutaneous nephrostomy in a 2-year-old child. Jackman et al. (9) described a novel percutaneous renal access technique using an 11-Fr peel-away vascular access sheath in seven infants and preschool age children. They defined the "mini-perc" as a percutaneous nephrolithotomy achieved through a sheath too small to accommodate a standard rigid nephroscope. The same group of authors (8) adapted the "mini-perc" to adult patients utilizing a 13-Fr ureteroscopy sheath for percutaneous access in seven patients. Monga (11) reported similar results using a 20-Fr nephrostomy sheath in 21 patients. Lahme et al. (12) also described this technique using a 15-Fr Amplatz sheath in 19 patients. However, the "mini-perc" technique of percutaneous nephrolithotomy in a large group, to our knowledge, has not been evaluated. We believe that our study of 72 patients is the most substantial assessment of this procedure since its initial description in 1997.
There are several unique aspects and advantages of our study. First, the immediate stone free rate was evaluated according to the longest diameter, the cumulative longest diameter, the cumulative stone burden, and the stone density. We noted that if the longest diameter of the stone was greater than 2.5 cm, the immediate stone free rate was significantly lower than that achieved with stones with the longest diameter of less than 2.5 cm. The cumulative longest diameter and cumulative stone burden also significantly influenced immediate stone-free rates, showing a sharp drop at diameters greater than 2.5 cm and at stone burden greater than 6 cm2. Therefore it might be wise to exclude patients with large diameter calculi or large stone burdens. There was no significant difference according to the stone density.
Our use of the 14-Fr peel-away sheath is an important point. Several instruments for the percutaneous tract have been used (see Discussion above). The 14-Fr peel-away sheath was applied to both adults and a 17-month-old boy in our study. There was a 78.2% reduction in the volume of renal parenchyma that was dilated by the 14-Fr sheath compared to traditional 30-Fr sheaths, and a 51% reduction compared to the 20-Fr sheath used by Monga (11).
The immediate stone-free rate was 80.6%, slightly lower than those of previous reports - 85% in children and 89% in adults by Jackman et al. (8, 9), 90% by Monga (11), and 100% by Lahme et al. (12). However, the average stone burden was 7.18 cm2 in our study, while those of previous reports were much smaller in comparison -1.2 cm2 and 1.5 cm2 by Jackman et al. (8, 9), 2.8 cm2 by Monga (11), and 2.4 cm2 by Lahme et al. (12).
In our study, the only major complication was hemorrhaging that occurred in a patient with early Child A liver cirrhosis, and therefore predisposed to bleeding. There were no major complications in the previous studies, but they had comparatively fewer cases (7-12). Moreover, the low rate (1.4%) of major complications enabled us to use the 14-Fr peel-away sheath instead of the 11-Fr peel-away vascular access sheath for children (9) and the 13-Frureteroscopy sheath for adults (8). Theoretically, the smaller diameter of the device for the percutaneous tract should decrease perioperative bleeding, pain, and postoperative parenchymal scarring (10). When serious complications developed, the radiologist, skilled in interventional techniques, played an integral role in managing them.
The mean hospital stay after the procedure was 3.97 days. A pediatric series of the "mini-perc" reported six days of hospital stay on average (9), and the same group of authors estimated 1.7 days of that for adults (8). Monga (11) estimated 1.1 days of mean hospital stay. These previous results are promising in terms of shortening the hospital stay for future patients.
There were a few limitations in our study. First, though nephrolithiasis is a rare disease in children that accounts for only 2% to 3% of all stone patients (20), we treated only one child, a 17-month-old boy, without complications. Therefore, the safety and usefulness of this technique has not been thoroughly evaluated in children. Further investigation is warranted to clarify whether the "mini-perc" technique using 14-Fr peel-away sheath could offer improved results in children. Second, there was no comparison study between the "mini-perc" technique and other treatment modalities for renal calculi. Only a literature review was available.
In conclusion, our three-year study described the first results of the "mini-perc" technique of percutaneous nephrolithotomy using a sufficient number of patients. We used the 14-Fr peel-away sheath in both children and adults. Also, we obtained high immediate stone free rates, which were influenced by stone diameter and burden. We observed a low complication rate and short hospital stays. An interventional radiologist played an important role in making and dilating the nephrostomy tract, and managing complications after the procedure. The treatment of renal calculi with the "mini-perc" requires the collaborative effort of interventional radiologists, urologists and genitourinary radiologists.
Figures and Tables
Fig. 1
A 17-month-old boy with upper pole calyceal and pelvic stones in the right kidney.
A-C. Abdominal radiograph and non-enhanced helical CT scans (120 kVp, 160 mA, 2.5 mm collimation) show upper pole calyceal and pelvic stones in the right kidney.
D. Nephrostomy was created toward the postero-inferior aspect of the renal stones.
E. Intraoperative abdominal radiograph demonstrates a safety guide wire (arrows) and a working guide wire (arrowheads) inserted on prone position.
F. One month after the procedure, renal stones are shown successfully removed on abdominal radiograph.

Fig. 3
A 65-year-old man with massive hematuria after the "mini-perc", who was diagnosed with Child A liver cirrhosis.
A. Right renal arteriogram shows suspicious contrast extravasation at the lower pole of the kidney.
B. Superselective renal arteriogram revealed a contrast extravasation from the arcuate artery of the right kidney.
C. After embolization with a coil and gelatin sponge, no further bleeding was seen.
References
1. Puppo P. Percutaneous nephrolithotripsy. Curr Opin Urol. 1999. 9:325–328.
2. Segura JW, Patterson DE, LeRoy AJ, Williams HJ, Barrett DM, Benson RC, et al. Percutaneous removal of kidney stones: review of 1,000 cases. J Urol. 1985. 134:1077–1081.
3. Stoller ML, Wolf JS, Lezin MA. Estimated blood loss and transfusion rates associated with percutaneous nephrolithotomy. J Urol. 1994. 152:1977–1981.
4. Lee WJ, Smith AD, Cubelli V, Badlani GH, Lewin B, Vernace F, et al. Complications of percutaneous nephrolithotomy. AJR Am J Roentgenol. 1987. 148:177–180.
5. Kessaris DN, Bellman GC, Pardalidis NP, Smith AD. Management of hemorrhage after percutaneous renal surgery. J Urol. 1995. 153:604–608.
6. Lingeman JE, Coury TA, Newman DM, Kahnoski RJ, Mertz JH, Mosbaugh PG, et al. Comparison of results and morbidity of percutaneous nephrolithotomy and extracorporeal shock wave lithotripsy. J Urol. 1987. 138:485–490.
7. Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997. 11:171–172.
8. Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW. The "mini-perc" technique: a less invasive alternative to percutaneous nephrolithotomy. World J Urol. 1998. 16:371–374.
9. Jackman SV, Hedican SP, Peters CA, Docimo SG. Percutaneous nephrolithotomy in infants and preschool age children: experience with a new technique. Urology. 1998. 52:697–701.
10. Monga M. Mini-percutaneous antegrade endopyelotomy. Tech Urol. 1999. 5:223–225.
11. Monga M, Oglevie S. Minipercutaneous nephrolithotomy. J Endourol. 2000. 14:419–421.
12. Lahme S, Bichler KH, Strohmaier WL, Gotz T. Minimally invasive PCNL in patients with renal pelvic and calyceal stones. Eur Urol. 2001. 40:619–624.
13. Fernstrom I, Johansson B. Percutaneous pyelolithotomy: A new extraction technique. Scand J Urol Nephrol. 1976. 10:257–259.
14. Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Nephrolithiasis clinical guidelines panel summary report on the management of staghorn calculi. The american urological association nephrolithiasis clinical guidelines panel. J Urol. 1994. 151:1648–1651.
15. Rodrigues NN, Claro JA, Ferreira U. Is percutaneous monotherapy for staghorn calculus still indicated in the era of extracorporeal shockwave lithotripsy? J Endourol. 1994. 8:195–197.
16. Netto NR, Claro JF, Lemos GC, Cortado PL. Renal caluli in lower pole calices: what is the best method of treatment? J Urol. 1991. 146:721–723.
17. Webb DR, Payne SR, Wickham JE. Extracorporeal shockwave lithotripsy and percutaneous renal surgery. Comparisons, combinations and conclusions. Br J Urol. 1986. 58:1–5.
18. Fuchs G, Miller K, Rassweiler J, Eisenberger F. Extracorporeal shock-wave lithotripsy: one-year experience with the Dornier lithotripter. Eur Urol. 1985. 11:145–149.
19. Boddy SA, Kellett MJ, Fletcher MS, Ransley PG, Paris AM, Whitfield HN, et al. Extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy in children. J Pediatr Surg. 1987. 22:223–227.
20. Sinno K, Boyce WH, Resnick MI. Childhood urolithiasis. J Urol. 1979. 121:662–664.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download