Abstract
We report here on a rare case of carotid artery angioplasty and stenting in a patient with spontaneous recanalization after complete occlusion of the proximal internal carotid artery (ICA). The patient initially showed severe stenosis at the left proximal ICA on MR angiography (MRA). Digital subtraction angiography (DSA) performed three days after MRA showed complete occlusion of the proximal ICA. The follow-up DSA after four weeks showed recanalization of the ICA, and then carotid artery stenting was successfully performed. There has been no neurologic complication during more than one year follow-up.
Acute internal carotid artery (ICA) occlusions may result in profound disability and death (1). An occluded ICA can spontaneously recanalize, but this doesn't happen frequently, and the natural course of a proximal ICA occlusion and its possibility of recanalization, including the exact time of recanalization after occlusion, are not well known (2, 3). A few studies have reported the incidence of spontaneous recanalization of the proximal internal carotid artery, which has mostly occurred in patients with ICA dissections (4-6). A few limited studies have reported a considerable incidence of spontaneous recanalization in patients with underlying atherosclerotic lesion or atherothombotic diseases (2). The possibility of repeated occlusion and repeated cerebral ischemic infarction may exist for the patients exhibiting spontaneous recanalization of the ICA and underlying atherosclerosis. We report here on a case of carotid artery stenting (CAS) in a patient who exhibited underlying atherosclerosis with spontaneous recanalization after complete occlusion of the proximal ICA.
A 56-year-old man was admitted for acute right hemiparesis and a mild speech disturbance (3 on the modified Rankin Scale). He was well before admission without a history of hypertension, diabetes mellitus or hypercholesterolemia. On admission, the MRI scan revealed watershed and a small cortical ischemic infarction at the left cerebral hemisphere with diffusion abnormality on the diffusion weighted image (DWI, Fig. 1A) and a decreased apparent diffusion coefficient (ADC). MR angiography (Fig. 1B) revealed severe stenosis at the left proximal ICA.
Three days after admission, digital subtraction angiography (DSA) was performed to plan for CAS. The DSA showed complete occlusion of the left proximal ICA without forward flow to the distal ICA from the point of occlusion, moderate to severe stenosis at the left proximal external carotid artery and atherosclerotic plaque with ulcer at the distal common carotid artery (Fig. 2A). The delayed phase of the left common carotid angiography (Fig. 2B) showed retrograde filling of contrast media from the supraclinoid ICA to the cervical ICA distal to the occlusion. The left arteries of the anterior circulation were seen from the prominent transdural collateral vascular supply of the distal external carotid artery (ECA) branches via the transopthalmic route, and from the right anterior cerebral artery via the anterior communicating artery. There was no evidence of aggravation of the patient's neurologic status as compared with his neurologic status at the time of admission. We did not attempt to recanalize the occluded ICA because the patient already had acute ischemic infarction and he showed no neurological aggravation. He was medicated with only aspirin (300 mg/day) and clopidogrel (75 mg/day). The patient's neurologic status then slightly improved.
A follow-up DSA (Figs. 3A, B) was performed four weeks after ictus for attempting to insert a stent into the severely stenotic proximal ECA and ulcerated CCA, and the DSA revealed spontaneous recanalization of the left proximal ICA with a tight stenosis and forward flow. The patient was stable at that time. For prevention of repeated occlusion of the ICA and ischemic infarction, CAS was performed under local anesthesia without sedation. The blood pressure, pulse and oxygen saturation were continuously monitored throughout the procedure, and the neurologic assessment was performed by a neurosurgeon. Systemic anticoagulation was performed via the intravenous administration of a bolus of heparin (5,000 U).
Pre-stenting balloon angioplasty was performed by using a 3 mm diameter balloon (Maveric, Boston Scientific, Galway, Ireland). A self-expandable Carotid Wallstent (Boston Scientific, Natick, MA, 8 mm in diameter and 3.1 cm in length) was deployed from the left proximal ICA to the distal common carotid artery. After the stent insertion, post-stenting balloon angioplasty was performed due to the residual stenosis by using a 6 mm diameter balloon (Ultrasoft-SV, Boston Scientific, Natick, MA). We could not use the distal protection device during the procedure because the diameter of the distal cervical ICA was less than 2.5 mm. No neurophysiological changes were identified during or after the procedure. Angiography after CAS showed good deployment of the stent (Fig. 4), and there were no findings of intracranial vascular abnormality.
There was no evidence of periprocedural hypertension. After the procedure, the patient was closely monitored in the intensive care unit for 24 hours and hydration was done under strict blood pressure control (under 120/80 mmHg). Four days after procedure, the patient was discharged without any complication. During one year follow-up, there has been no neurologic complication (Modified Rankin Scale 0-1). There was no significant recurred stenosis on the follow-up Doppler ultrasound that was done one year after the CAS (Fig. 5).
Although spontaneous recanalization of acutely occluded carotid arteries is not a rare phenomenon, the prognosis and outcome of patients with acute ICA occlusion are poor (3). Recanalizations of occluded ICAs have been reported to occur between one hour to 24 days after the baseline examinations (3, 7). The exact timing of spontaneous recanalization remains unclear because the time between the initial occlusion and the follow-up examination has varied in different reports. Spontaneous recanalization of the ICA has been described as a common phenomenon in ICA dissections in about 57% to 68% of the cases (4-6), but it has rarely been seen in the patients suffering with an underlying atherosclerotic disease or an embolic cause. The majority of occlusions of the ICA are due to atherosclerosis, where preexisting high-grade stenotic lesions of the sinus generate local thrombosis due to the rupture of an unstable atherosclerotic plaque (1). All angiographic runs should be carried out to the completion of the late venous phase through the distal extracranial ICA and thought the entire intracranial ICA in the cases of possible occlusion to differentiate "pseudo-occlusion" that is due to an extremely slow blood flow (2). The mechanism of recanalization, whether it occurs early or late, is also unclear. Several mechanisms, including vasospasm, distal embolization of an occlusive clot, and spontaneous intravascular lysis and fragmentation of the thrombus have been proposed to explain recanalization (2, 3). The possible explanation for the spontaneous recanalization of this case is that there might have been some autolysis. Spontaneous recanalization depends on the composition of the thrombus (2), and the role medications and collateral flow may have in the process of recanalization are unclear (3, 8). The patient only received aspirin and clopidogrel after discovery of the ICA occlusion. Retrograde flow from the supraclinoid ICA to occluded proximal ICA may have had an important role for recanalization in our case, which means there was good collateral flow to the affected site. Our patient had prominent transopthalmic collateral flow, good collateral flow from the contralateral anterior carotid artery (ACA) and retrograde flow to the proximal ICA. Meves et al. (2) reported four cases of spontaneous recanalization of the ICA occlusion with underlying atherosclerotic disease, and retrograde flow was shown in all four cases. Nguyen-Huynh et al. (3) also reported two cases of spontaneous recanalization of ICA occlusion, and one of which showed retrograde contrast media filling to the proximal ICA. CT angiography and color Doppler ultrasonography have been reported as effective noninvasive modalities to detect recanalization of occluded ICAs.
With development of neurointerventional techniques and devices, including the distal protection device, CAS has become an excellent treatment modality for carotid stenosis (9, 10). The technical success rate, the procedure related morbidity and mortality rates and the restenosis rates seem to compare favorably with carotid endarterectomy.
Follow-up angiography four weeks after ictus was performed for our patient to look for the possibility of inserting a stent into the stenotic proximal external carotid and ulcerated distal common carotid arteries, which might be future sources of distal embolism from the ECA to the intracranial cerebral arteries. Follow-up angiography showed recanalization of the proximal ICA with severe atherosclerotic stenosis, and so CAS was done during the same session as the follow-up angiography. We did not attempt to perform a recanalization procedure on the occluded ICA at the time of the initial DSA because the patient had acute ischemic infarction at the ipsilateral cerebral hemisphere that could have caused possible intracranial hemorrhage after the procedure. Fortunately, our patient did not show an aggravated neurological status at that time after the initial ictus.
The CAS procedures in this special situation require the experience and extensive knowledge of CAS by the interventionist. Another possibility of risk during CAS can exist during passing the distal protection device to the stenotic segment and also during pre-stenting balloon angioplasty that is done without a distal protection device. We did not use the distal protection device because there was no available distal protection device with a small enough diameter to insert within the distal cervical ICA. So, we performed pre-stenting balloon angioplasty very gently, and all procedures were done with careful monitoring of the vital signs and neurologic status of the patient. The patient was carefully monitored after the procedure as well.
In summary, we performed successful CAS without any neurologic complication occurring during the one year follow-up in a patient with a spontaneous recanalized ICA occlusion. Although reports on stent insertion at a recanalized ICA occlusion are rare, CAS may considered as the treatment of choice for the patient having an underlying atherosclerotic stenosis and a recanalized ICA following complete occlusion.
Figures and Tables
Fig. 1
The initial diffusion weighted image (A) showed bright signal intensity at the left frontoparietal lobe cortex. Focal severe stenosis is visible at the left proximal internal carotid artery on MR angiography (B).

Fig. 2
Left common carotid arteriography (A) obtained three days after initial ictus revealed complete occlusion of the left proximal internal carotid artery. The delayed phase of left common carotid angiography (B) showed transdural intracranial collateral flow through the ophthalmic artery and retrograde contrast media filling of the distal cervical internal carotid artery.

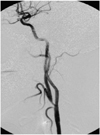
Fig. 3
Follow-up digital subtraction angiography obtained four weeks after the initial attack showed recanalization of the left proximal internal carotid artery with a remaining tight stenosis at the proximal internal carotid artery.

References
1. Meyer FB, Sundt TM Jr, Piepgras DG, Sandok BA, Forbes G. Emergency carotid endarterectomy for patients with acute carotid occlusion and profound neurological deficits. Ann Surg. 1986. 203:82–89.
2. Meves SH, Muhs A, Federlein J, Buttner T, Przuntek H, Postert T. Recanalization of acute symptomatic occlusions of the internal carotid artery. J Neurol. 2002. 249:188–192.
3. Nguyen-Huynh MN, Lev MH, Rordorf G. Spontaneous recanalization of internal carotid artery occlusion. Stroke. 2003. 34:1032–1034.
4. Bogousslavsky J, Despland P-A, Regli F. Spontaneous carotid dissection with acute stroke. Arch Neurol. 1987. 44:137–140.
5. Steinke W, Rautenberg W, Schwartz A, Henerici M. Noninvasive monitoring of internal carotid artery dissection. Stroke. 1994. 25:998–1005.
6. Sturzenegger M, Mattle HP, Rivoir A, Baumgartner RW. Ultrasound findings in carotid artery dissection: Analysis of 43 patients. Neurology. 1995. 45:691–698.
7. Pryor JC, Setton A, Nelson PK, Berenstein A. Complications of diagnostic cerebral angiography and tips on avoidance. Neuroimaging Clin N Am. 1996. 6:751–758.
8. Ringlelstein EB, Biniek R, Weiller C, Ammeling B, Nolte PN, Thron A. Type and extent of hemispheric brain infarctions and clinical outcome in early and delayed middle cerebral artery recanalization. Neurology. 1992. 42:289–298.
9. Wholey MH, Al-Mubarek N, Wholey MH. Updated review of the global carotid artery stent registry. Catheter Cardiovasc Interv. 2003. 60:259–266.
10. Malek AM, Higashida RT, Phtouros CC, Lempert TE, Meyers PM, Smith WS, et al. Stent angioplasty for cervical artery stenosis in high-risk symptomatic NASCET-ineligible patients. Stroke. 2000. 31:3029–3033.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download