Abstract
Objective
To evaluate the long-term follow-up results of percutaneous ethanol injection (PEI) for the treatment of hepatocellular carcinoma (HCC) in Korea.
Materials and Methods
Sixty-eight nodular HCCs initially detected in 64 patients, were subjected to US-guided PEI as a first-line treatment. Long-term survival rates, local tumor progression rates, and complications were evaluated, as were the influences of tumor size and Child-Pugh class on these variables.
Results
No major complications occurred. The overall survival rates of the 64 patients at three and five years were 71% and 39%, and their cancer-free survival rates were 22% and 15%, respectively. The overall survival rate of patients with a small HCC (≤ 2 cm) was significantly higher (p = 0.014) than that of patients with a medium-sized HCC (≤ 2 cm). The overall survival rate of patients with Child-Pugh class A was significantly higher (p = 0.049) than that of patients with Child-Pugh class B. Of 59 cases with no residual tumor, local tumor progression was observed in ablation zones in 18, and this was not found to be significantly influenced by tumor size or Child-Pugh class.
Conclusion
The results of our investigation of the long-term survival rates of PEI in HCC patients in Korea (a hepatitis B virus-endemic area) were consistent with those reported previously in hepatitis C endemic areas. Patients with a smaller tumor or a better liver function exhibited superior survival rates.
Percutaneous ethanol injection (PEI) is a low-risk, well-established treatment for patients suffering from cirrhosis and a relatively early-stage hepatocellular carcinoma (HCC). Since early reports regarding the therapeutic efficacy of PEI were issued (1-4) and subsequent reports on medium-term survival results (5-9), the long-term therapeutic efficacy of PEI for HCC has been addressed by several investigators (10-14). The majority of these studies have been conducted in Japan, Italy, and Spain; all hepatitis C endemic areas. However, relatively few reports have addressed long-term (5 years or longer) survival in hepatitis B endemic areas, which include China, Taiwan, Vietnam, Korea, and certain African countries. A Korean report and two Taiwanese papers, which included medium-term (3-year) survival results, found one, two, and three year overall survival rates for PEI of 85-98%, 61-96%, and 50-88%, respectively (15-17). Thus, the objective of the present study was to characterize the long-term results of PEI for HCC in Korea, a hepatitis B endemic area.
Between January 1995 and April 1999, 64 patients with 68 nodular HCCs were treated by PEI as a first-line treatment at our institution. The study subjects comprised 41 men and 23 women, ranging from 34 to 87 years old (mean, 59 years). Fifty-six patients tested positive for serum hepatitis B surface antigen, and seven tested positive for anti-hepatitis C virus antibody. Fifty-five patients exhibited cirrhosis following hepatitis, eight had chronic active hepatitis, and one patient showed no evidence of a liver pathology. At the time of PEI treatment, the numbers of Child-Pugh class A and B liver cirrhosis patients were 32 and 23, respectively.
All of the included patients fulfilled the following criteria for PEI treatment: a single nodular HCC of < 4 cm in maximum diameter; multinodular HCCs (up to three in number), and each tumor < 3 cm in maximum diameter; tumors were accessible via a percutaneous approach; the absence of portal venous thrombosis or extrahepatic metastases; Child-Pugh class A or B liver cirrhosis; a prothrombin time ratio > 40%, and a platelet count > 40,000/mm3 (40 cells×109/L). This study was approved by our institutional review board, and written informed consent was provided by all patients.
Hepatocellular carcinoma diagnoses were verified using ultrasound (US)-guided percutaneous needle biopsies in 63 of the 68 masses (92.6%). The remaining 5 tumors were considered to be HCCs based on characteristic imaging findings and elevated levels of serum α-fetoprotein (AFP). Small HCCs and medium-sized HCCs were defined as being ≤ 2 cm in diameter and > 2 cm in diameter, respectively. HCCs were graded histologically as well differentiated, moderately differentiated, or poorly differentiated in accordance with the Liver Cancer Group of Japan's classification of primary hepatic cancer.
All of patients underwent conventional, multisession US-guided PEI (total session, 248; mean session per tumor, 3.65). The needle used for these procedures were 21-gauge needles, with three side holes, and no end hole (PEIT Needle; Hakko, Tokyo). The total amount of alcohol injected was determined by tumor diameter: 8 ml for lesions of 1.0 cm in diameter, 15 ml for 2.0 cm lesions, and 25 ml for 3.0 cm lesions. Injections were performed two or three times a week, depending on patient tolerance, until the total amount of alcohol injected reached the intended volume. Three to eight milliliters of ethanol were administered to each tumor until the ethanol distributed throughout a tumor or until ethanol leakage from a tumor was observed.
Immediate US was conducted in order to evaluate any emergent complications, and therapeutic efficacy was assessed from US, CT, and AFP assays, one month after PEI treatment completion. Patient response was considered complete when sequential CT scans evidenced no areas of contrast material enhancement in a lesion, and when CT and US scans indicated no increase tumor size. In cases with evidence of technical success with no new lesions by one month follow-up CT, subsequent follow-up CTs were administered at 3-month intervals.
When, during follow-up, our imaging methods revealed local recurrences or new lesions that were treatable, additional PEI, percutaneous transarterial chemoembolization, radiofrequency ablation, surgery, or combinations thereof were conducted.
Follow-up times ranged from three to 99 months (median, 50 months; mean, 43.6 months). Of the 64 subjects, 13 (20.3%) were followed-up for five years or more.
Cumulative overall and cancer-free survival rates were calculated using the Kaplan-Meier method. The log-rank test was employed to determine differences in survival rates with respect to; tumor size, histopathologic grades, and Child-Pugh classification. Differences in local tumor progression rates with respect to tumor size and Child-Pugh classification were calculated using Chi-square and Fisher's exact tests. These calculations were carried out using SPSS software (SPSS for Windows; SPSS Inc., Chicago, IL).
Tumor sizes in our study patients ranged between 0.8 and 4 cm (mean 2.1 cm); in 39 patients, 43 HCCs were found that were ≤ 2 cm in diameter, and in 25 patients, 25 HCCs that were in > 2 cm in diameter. The degree of histopathologic differentiation was assessed using Edmonson grade, as follows; 18 tumors grade I, 23 tumors grade II, 15 tumors grade III, three tumors grades I or II, and four tumors of grades II or III.
At the end of this study, 20 patients remained alive, and 38 patients had succumbed. Six patients were lost to follow-up. The cumulative overall and cancer-free survival curves of the 64 study subjects are shown in Figure 1. Overall survival rates at one, two, three, and five years were 92%, 81%, 71%, and 39%, respectively, and the corresponding cancer-free survival rates were 56%, 30%, 22%, and 15%, respectively.
One-, 2-, 3-, and 5-year survival rates were 95%, 90%, 76%, and 55%, respectively, for the 39 patients with tumors ≤ 2 cm in largest dimension; and were 88%, 67%, 63%, and 17%, respectively, for the 25 patients with HCCs > 2 cm in largest dimension (Fig. 2). Mean survival of patients with a HCC ≤ 2 cm in diameter was significantly longer (p = 0.014) than that of patients with a HCCs > 2 cm in diameter. The ages (p = 0.855), sexes (p = 0.458), and Child-Pugh classes (p = 1.000) of patients a HCC ≤ 2 cm or > 2 cm in diameter were not significantly different.
Mean 1-, 2-, 3-, and 5-year survival rates were estimated to be 91%, 80%, 75%, and 38%, respectively, for the 21 patients with well-differentiated HCC (grade I or I > II); and 91%, 78%, 65%, and 33%, respectively, for the 38 patients with moderately- or poorly differentiated HCCs (grade II, III or grade II > I), and no statistically significant difference was found between these two differentiation-based groups (p = 0.705).
For patients with Child-Pugh class A cirrhosis of the liver (n = 32), the 1-, 3-, 5-, and 6-year survival rates were 100%, 84%, 48%, and 36%, respectively, and these figures were significantly higher (p = 0.049) than those of patients with Child-Pugh class B (n = 23), who had survival rates of 82% at one year, 55% at three years, 21% at five years, and 11% at 6 years (Fig. 3). The ages (p = 0.696) and sexes (p = 0.254) of Child-Pugh class A and Child-Pugh class B patients were not significantly different.
During follow-up examinations, of 59 tumors (in 59 patients) with no residual tumor, local tumor progression in ablation zones was detected for 18 tumors (31%). The local tumor progression rates were 23% (9 of 39 HCCs) for tumors ≤ 2 cm in diameter, and 45% (9 of 20 HCCs) for tumors > 2 cm. For 50 tumors in cirrhotic livers, local tumor progression rates were 30% (9 of 30 HCCs) in patients with Child-Pugh class A, and 20% (4 of 20 HCCs) in patients with Child-Pugh class B, and no significant relation was found between tumor size (p = 0.161) and Child-Pugh class (p = 0.522).
No major complications occurred among a total of 248 PEI sessions, an average of 3.65 sessions per tumor. Follow-up CT showed intraperitoneal hemorrhage in two patients, but these resolved spontaneously.
Percutaneous ethanol injection has been widely employed to treat HCCs smaller than 3 to 5 cm (7, 9, 10, 12-14, 18). Because of its strong dehydrating effect, ethanol induces the immediate coagulative necrosis of tumor cells, and enables the complete ablation of small neoplastic lesions, without adversely affecting liver function (1, 3-6, 19-21).
Several studies on survival after PEI have been reported in hepatitis C endemic areas, such as, Japan and Italy. As compared with HCCs in patients with hepatitis C infections, HCCs related to hepatitis B infections show larger, more infiltrative, and a greater frequently of multiple tumors at first imaging, and in addition, recurrences are more commonly after treatment (15, 22, 23). However, the underlying hepatic functional reserves in patients with hepatitis B associated HCC are usually better than those with hepatitis C associated HCC (22). According to one report, after surgical resection, patients with hepatitis B associated HCC showed poorer survival than patients with hepatitis C associated HCC (23).
In our study, we obtained 3-year and 5-year survival rates of 71% and 39%, respectively. Survival reached 76% at three years and 55% at five years, in patients with a tumor of ≤ 2 cm in diameter, and 63% at 3years, and 17% at 5 years, in patients with a tumor > 2 cm in diameter. These results are consistent with those reported by other investigators in areas in which the hepatitis C virus is endemic (10-14). Moreover, these similar survival figures demonstrate the reliability and reproducibility of the PEI technique. In addition, several investigators have shown that survival rates are influenced by tumor size and Child-Pugh class (10, 11), and our findings concur.
In the present study, the survival rates of Child-Pugh class A patients were 48% at five years and 36% at six years. These figures are similar to those obtained for patients treated by hepatic resection (10, 24). Surgical resection in early-stage HCC was reported to result in 5-year survival rates of 41-51% (25-27). Yamamoto et al. (24) also examined the efficacies of PEI and surgical resection for the treatment of small HCCs, and found that 3- and 5-year overall survival rates were almost identical (82.1%, and 59.0%, respectively, in the PEI group; 84.4%, and 61.5%, respectively, in the surgical group). Although no prospective, randomized trials have been conducted to compare the efficacies of PEI and surgery, their long-term results appear comparable.
Moreover, a comparison of relevant data demonstrated that survival after PEI tends to be superior to survival after conventional transarterial chemoembolization. The mean 5-year survival rate shown by 556 patients with HCC lesions of < 5 cm, all of whom had been treated by conventional transarterial chemoembolization, was only 14% (10). However, transarterial chemoembolization may cause liver functions to worsen, because the technique also damages noncancerous liver parenchyma (28, 29). However, more recent results obtained for segmental and subsegmental transarterial chemoembolization have been more encouraging (30-32).
Some recent reports have asserted that the local tumor progression rate after PEI is about 33-43% (33, 34), which is consistent with our findings (31%). However, this high tumor recurrence rate does not represent a comparative limitation of PEI, as similar rates are frequently found in cirrhotic patients with HCC treated with any therapeutic modality, including surgery (35, 36). Moreover, in the present study, tumor size and Child-Pugh class were found to be related to local tumor progression.
Radiofrequency ablation is now replacing PEI for the treatment of HCCs, because of its higher rate of complete necrosis, requirement for fewer treatment sessions, and higher cancer-free survival rates (37-40). However, in terms of cost, PEI is definitely superior to radiofrequency ablation. In our experience, PEI should be recommended particularly for diminutive HCCs (< 1.5 cm), including residual and recurrent tumors, because treatment with probably require only one or two PEI sessions.
However, our study has its limitations. First, a number of the patients enrolled in this study were also treated using modalities other than PEI. Multimodal treatments, including repeat PEI, transarterial chemoembolization, radiofrequency ablation, and surgery were conducted in cases with residual or recurrent tumors, i.e., PEI in four, transarterial chemoembolization in 16, radiofrequency ablation in nine, surgical resection in three, radiofrequency ablation and transarterial chemoembolization in 11, PEI and transarterial chemoembolization in six, and surgical resection and radiofrequency ablation in two. This is also an inherent limitation of similar prior studies. Second, the proportion of censored data was relatively high. The retrospective nature of this study made it difficult to perform adequate follow-up examinations for all patients, and survival was confirmed by telephone interview with a family member for 23 of 64 patients, which made it impossible to determine cumulative local or remote site tumor recurrence rates. Third, the relation between survival rate and tumor location was not assessed, because of the retrospective nature of the study, it was difficult to assess if HCCs were located in the periphery or the center of livers using only transverse CT images.
In conclusion, our study demonstrates the long-term effectiveness of PEI for the treatment of HCC in a hepatitis B virus endemic area. Our long-term survival results for HCC patients treated with PEI are comparable to those previously reported in hepatitis C endemic areas. Unsurprisingly, both tumor size and degree of liver function were found to significantly affect survival rates and times. Although radiofrequency ablation is rapidly replacing PEI as a treatment modality, PEI still appears to be both effective and safe for the treatment of small HCCs.
Figures and Tables
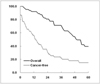 | Fig. 1The cumulative overall and cancer-free survival curves of our 64 study subjects with hepatocellular carcinoma, who treated by percutaneous ethanol injection. |
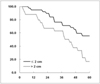 | Fig. 2Cumulative survival curves of the 64 hepatocellular carcinoma patients after percutaneous ethanol injection treatment, according to tumor size. The survival rates of patients with a hepatocellular carcinoma of ≤ 2 cm in diameter (n = 39, black line) were determined to be significantly higher (p = 0.014, log-rank test) than those of patients with as hepatocellular carcinoma of ≤ 2 cm in diameter (n = 25, gray line). |
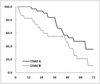 | Fig. 3The cumulative survival curves of 55 hepatocellular carcinoma patients after percutaneous ethanol injection treatment, with respect to the Child-Pugh classification of the clinical stage of coexistent cirrhosis of the liver. The survival rates of class-A patients (n = 32, black line), and class-B patients (n = 23, gray line) were significantly different (p = 0.049, log-rank test). |
References
1. Bartolozzi C, Lencioni R. Ethanol injection for the treatment of hepatic tumours. Eur Radiol. 1996. 6:682–696.
2. Livraghi T, Festi D, Monti F, Salmi A, Vettori C. US-guided percutaneous alcohol injection of small hepatic and abdominal tumors. Radiology. 1986. 161:309–312.
3. Shiina S, Yasuda H, Muto H, Tagawa K, Unuma T, Ibukuro K, et al. Percutaneous ethanol injection in the treatment of liver neoplasms. AJR Am J Roentgenol. 1987. 149:949–952.
4. Sheu JC, Sung JL, Huang GT, Chen DS, Yang PM, Lai MY, et al. Intratumor injection of absolute ethanol under ultrasound guidance for the treatment of small hepatocellular carcinoma. Hepatogastroenterology. 1987. 34:255–261.
5. Livraghi T, Salmi A, Bolondi L, Marin G, Arienti V, Monti F, et al. Small hepatocellular carcinoma: percutaneous alcohol injection-results in 23 patients. Radiology. 1988. 168:313–317.
6. Shiina S, Tagawa K, Unuma T, Fujino H, Uta Y, Niwa Y, et al. Percutaneous ethanol injection therapy of hepatocellular carcinoma: analysis of 77 patients. AJR Am J Roentgenol. 1990. 155:1221–1226.
7. Ebara M, Ohto M, Sugiura N, Kita K, Yoshikawa M, Okuda K, et al. Percutaneous ethanol injection for the treatment of small hepatocellular carcinoma. Study of 95 patients. J Gastroenterol Hepatol. 1990. 5:616–626.
8. Giorgio A, Tarantino L, Francica G, Scala V, Mariniello N, Aloisio T. Percutaneous ethanol injection under sonographic guidance of hepatocellular carcinoma in compensated and decompensated cirrhotic patients. J Ultrasound Med. 1992. 11:587–595.
9. Livraghi T, Bolondi L, Lazzaroni S, Marin G, Morabito A, Rapaccini GL, et al. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma in cirrhosis. A study on 207 patients. Cancer. 1992. 69:925–929.
10. Livraghi T, Giorgio A, Marin G, Salmi A, de Sio I, Bolondi L, et al. Hepatocellular carcinoma and cirrhosis in 746 patients: long-term results of percutaneous ethanol injection. Radiology. 1995. 197:101–108.
11. Lencioni R, Pinto F, Armillotta N, Bassi AM, Moretti M, Di Giulio M, et al. Long-term results of percutaneous ethanol injection therapy for hepatocellular carcinoma in cirrhosis: a European experience. Eur Radiol. 1997. 7:514–519.
12. Shiina S, Tagawa K, Niwa Y, Unuma T, Komatsu Y, Yoshiura K, et al. Percutaneous ethanol injection therapy for hepatocellular carcinoma: results in 146 patients. AJR Am J Roentgenol. 1993. 160:1023–1028.
13. Castells A, Bruix J, Bru C, Fuster J, Vilana R, Navasa M, et al. Treatment of small hepatocellular carcinoma in cirrhotic patients: a cohort study comparing surgical resection and percutaneous ethanol injection. Hepatology. 1993. 18:1121–1126.
14. Kotoh K, Sakai H, Sakamoto S, Nakayama S, Satoh M, Morotomi I, et al. The effect of percutaneous ethanol injection therapy on small solitary hepatocellular carcinoma is comparable to that of hepatectomy. Am J Gastroenterol. 1994. 89:194–198.
15. Kang HW, Kim YJ, Kim KM, Kang JM, Kim SH, Kim JH, et al. Efficacy of percutaneous ethanol injection therapy in Korean with hepatocellular carcinoma. Korean J Gastroenterol. 2003. 42:502–509.
16. Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma < or = 4 cm. Gastroenterology. 2004. 127:1714–1723.
17. Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Randomized controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut. 2005. 54:1151–1156.
18. Lencioni R, Bartolozzi C, Caramella D, Paolicchi A, Carrai M, Maltinti G, et al. Treatment of small hepatocellular carcinoma with percutaneous ethanol injection. Analysis of prognostic factors in 105 Western patients. Cancer. 1995. 76:1737–1746.
19. Seki T, Nonaka T, Kubota Y, Mizuno T, Sameshima Y. Ultrasonically guided percutaneous ethanol injection therapy for hepatocellular carcinoma. Am J Gastroenterol. 1989. 84:1400–1407.
20. Tanaka K, Okazaki H, Nakamura S, Endo O, Inoue S, Takamura Y, et al. Hepatocellular carcinoma: treatment with a combination therapy of transcatheter arterial embolization and percutaneous ethanol injection. Radiology. 1991. 179:713–717.
21. Shiina S, Tagawa K, Unuma T, Takanashi R, Yoshiura K, Komatsu Y, et al. Percutaneous ethanol injection therapy for hepatocellular carcinoma. A histopathologic study. Cancer. 1991. 68:1524–1530.
22. Benvegnu L, Alberti A. Patterns of hepatocellular carcinoma development in hepatitis B virus and hepatitis C virus related cirrhosis. Antiviral Res. 2001. 52:199–207.
23. Chen TH, Tseng LM, Chau GY, Lui WY, Tsay SH, King KL, et al. Clinicopathologic and prognostic differences between patients with hepatitis B- and C-related resectable hepatocellular carcinoma. J Formos Med Assoc. 2001. 100:443–448.
24. Yamamoto J, Okada S, Shimada K, Okusaka T, Yamasaki S, Ueno H, et al. Treatment strategy for small hepatocellular carcinoma: comparison of long-term results after percutaneous ethanol injection therapy and surgical resection. Hepatology. 2001. 34:707–713.
25. Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999. 30:1434–1440.
26. Fong Y, Sun RL, Jarnagin W, Blumgart LH. An analysis of 412 cases of hepatocellular carcinoma at a Western center. Ann Surg. 1999. 229:790–800.
27. Wayne JD, Lauwers GY, Ikai I, Dohery DA, Belghiti J, Yamaoka Y, et al. Preoperative predictors of survival after resection of small hepatocellular carcinomas. Ann Surg. 2002. 235:722–731.
28. Khan KN, Nakata K, Kusumoto Y, Shima M, Ishii N, Koji T, et al. Evaluation of nontumorous tissue damage by transcatheter arterial embolization for hepatocellular carcinoma. Cancer Res. 1991. 51:5667–5671.
29. Nishizaki T, Takenaka K, Yoshida K, Ikeda T, Sugimachi K. Influence of lipiodolization on a cirrhotic liver. J Surg Oncol. 1995. 58:263–268.
30. Uchida H, Ohishi H, Matsuo N, Nishimine K, Ohue S, Nishimura Y, et al. Transcatheter hepatic segmental arterial embolization using lipiodol mixed with an anticancer drug and Gelfoam particles for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 1990. 13:140–145.
31. Matsuo N, Uchida H, Nishimine K, Soda S, Oshima M, Nakano H, et al. Segmental transcatheter hepatic artery chemoembolization with iodized oil for hepatocellular carcinoma: antitumor effect and influence on normal tissue. J Vasc Interv Radiol. 1993. 4:543–549.
32. Matsui O, Kadoya M, Yoshikawa J, Gabata T, Arai K, Demachi H, et al. Small hepatocellular carcinoma: treatment with subsegmental transcatheter arterial embolization. Radiology. 1993. 188:79–83.
33. Khan KN, Yatsuhashi H, Yamasaki K, Yamasaki M, Inoue O, Koga M, et al. Prospective analysis of risk factors for early intrahepatic recurrence of hepatocellular carcinoma following ethanol injection. J Hepatol. 2000. 32:269–278.
34. Koda M, Murawaki Y, Mitsuda A, Ohyama K, Horie Y, Suou T, et al. Predictive factors for intrahepatic recurrence after percutaneous ethanol injection therapy for small hepatocellular carcinoma. Cancer. 2000. 88:529–537.
35. Belghiti J, Panis Y, Farges O, Benhamou JP, Fekete F. Intrahepatic recurrence after resection of hepatocellular carcinoma complicating cirrhosis. Ann Surg. 1991. 214:114–117.
36. Nagasue N, Yukaya H, Ogawa Y, Sasaki Y, Chang YC, Niimi K. Clinical experience with 118 hepatic resections for hepatocellular carcinoma. Surgery. 1986. 99:694–701.
37. Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999. 210:655–661.
38. Lim HK. Radiofrequency thermal ablation of hepatocellular carcinomas. Korean J Radiol. 2000. 1:175–184.
39. McGhana JP, Dodd GD 3rd. Radiofrequency ablation of the liver: current status. AJR Am J Roentgenol. 2001. 176:3–16.
40. Lencioni RA, Allgaier HP, Cioni D, Olschewski M, Deibert P, Crocetti L, et al. Small hepatocellular carcinoma in cirrhosis: randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology. 2003. 228:235–240.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download