Abstract
The purpose of this study is to demonstrate whether the signal intensity (SI) of myocardial infarction (MI) on contrast enhanced (CE)-cine MRI is useful for differentiating recently infarcted myocardium from chronic scar. This study included 24 patients with acute MI (36-84 years, mean age: 57) and 19 patients with chronic MI (44-80 years, mean age: 64). The diagnosis of acute MI was based on the presence of typical symptoms, i.e. elevation of the cardiac enzymes and the absence of any remote infarction history. The diagnosis of chronic MI was based on a history of MI or coronary artery disease of more than one month duration and on the absence of any recent MI within the previous six months. Retrospectively, the ECG-gated breath-hold cine imaging was performed in the short axis plane using a segmented, balanced, turbo-field, echo-pulse sequence two minutes after the administration of Gd-DTPA at a dose of 0.2 mmol/kg body weight. Delayed contrast-enhanced MRI (DCE MRI) in the same plane was performed 10 to 15 minutes after contrast administration, and this was served as the gold standard of reference. The SI of the infarcted myocardium on the CE-cine MRI was compared with that of the normal myocardium on the same image. The area of abnormal SI on the CE-cine MRI was compared with the area of hyperenhancement on the DCE MRI. The area of high SI on the CE-cine MRI was detected in 23 of 24 patients with acute MI (10 with homogenous high SI, 13 high SI with subendocardial low SI, and one with iso SI). The area of high SI on the CE-cine MRI was larger than that seen on the DCE MRI (p < 0.05). In contrast, the areas of chronic MI were seen as iso-SI with thin subendocardial low SI on the CE-cine MR in all the chronic MI patients. The presence of high SI on both the CE-cine MRI and the DCE MRI is more sensitive (95.8%) for determining the age of a MI than the presence of myocardial thinning (66.7%). This study showed the different SI patterns between recently infarcted myocardium and chronic scar on the CE-cine MRI. CE-cine MRI is thought to be quite useful for determining the age of myocardial infarction, in addition to its utility for assessing myocardial contractility.
In the acute and chronic setting of ischemic heart disease, the portion of the myocardium showing delayed enhancement on MRI is known to have suffered myocardial infarction (MI), and this is non-viable myocardium. There is no difference in the hyperenhancement between acute and chronic infarcted myocardium on the delayed contrast enhanced (DCE) MRI. In the past, determining the age of the infarcted myocardium has been done by measuring its thickness (1). Some reports have shown that a combined assessment with using DCE MRI and T2-weighted MRI is useful for distinguishing chronic scar from acute MI (2, 3).
Cine MRI with the steady state free precession (SSFP)-based sequences is a major sequence of cardiac MRI that can represent the contractility of the myocardium and the ventricular function (4). CE-cine MRI with the SSFP-based sequences has recently been shown to provide the simultaneous assessment of myocardial function and the viability in those patients suffering with acute MI via its intrinsic T2/T1 contrast (5).
We hypothesized that there are different enhancement patterns for acute and chronic infarcted myocardium on the CE-cine MRI. The purpose of this study is to determine whether the signal intensity (SI) of MI on CE-cine MRI is useful for differentiating recently infarcted myocardium from chronic scar tissue.
From March 2003 to March 2004, 56 patients underwent cardiac MRI with the CE-cine MRI and DCE MRI sequences at our hospital. We retrospectively reviewed the clinical and medical history of these patients and we then classified them into the acute and chronic MI groups. In the acute MI group, twentyfour patients (21 men and 3 women, mean [± standard deviation; SD] age: 58±11 years) had chest pain and elevation of cardiac-specific serum enzymes for almost one month or less before MRI scanning (range: 1-6 days, mean: 3.5 days). They all underwent revascularization one to six days (median: 3 days) prior to the MR scanning.
In the chronic MI group, nineteen patients (17 men and 2 women, mean [± SD] age: 64±8 years) had documented histories of ischemic heart disease of more than one and on the absence of a recent MI with in the previous six months (> 6 months); most of these patients (n = 16) underwent diagnostic coronary angiography at our hospital. All the chronic MI patients were asymptomatic at the time of their MRI examination.
For the MRI examination, each patient was placed in the supine position in a 1.5-T clinical scanner (Gyroscan Intera, Philips), and a phased-array receiver coil was placed on the chest for imaging. All the images were acquired while the patient held his or her breath for approximately eight seconds; the images were then gated to the electrocardiogram. Five short-axis views of the cine images were acquired with using the balanced turbo field echo sequence (TR: 3.5 ms, TE: 2.0 ms, flip angle: 50 degrees, matrix: 272×272, slice thickness: 10 mm, gap: 10 mm). The gadolinium-based contrast agent (gadopentetate dimeglumine) was then administered intravenously at a dose of about 0.2 mmol per kilogram of body weight. The CE-cine MR images were acquired in the same plane with the same MR sequence two minutes after contrast administration. The DCE MR images were acquired with nine to ten short axis views by using a two-dimensional, inversion-recovery gradient-echo MR sequence (T1 turbo field echo, TR: 5.1 ms, TE: 1.5 ms, flip angle: 15 degrees, matrix: 304×304, slice thickness: 10 mm and no gap). The inversion time was individually selected to minimize the signal from the viable myocardium.
The apical, mid-ventricular and basal slices were selected from the sets of the CE-cine MRI images in mid-diastolic phase and the slices that corresponded the most to the above stated images were obtained from the set of DCE MRI images. Selecting images in the identical plane was possible in all the cases.
Two observers (K.A.K and J.B.S) analyzed the two sets of images. The SI of the myocardium was classified into the following four categories, as compared with the SI of surrounding viable myocardium: high signal intensity, high signal intensity with internal low iso and low SI. The area of abnormal SI was also measured on both the CE-cine and DCE MRI images. The least thickness of myocardium with abnormal SI was measured on the CE-cine MR images at the end diastolic phase. All the measurement was done by two observers while working in consensus.
We calculated the sensitivity of the abnormal signal intensity on the CE-cine MR images and the end diastolic myocardial thickness for the differentiation of acute MI from chronic MI, respectively. The threshold thickness we used for diagnosing chronic MI in our study was 6 mm because it has been shown by pathological studies that the scarred myocardium of chronic MI is usually associated with substantial myocardial thinning to < 6 mm, or even with aneurysm formation (6). The areas of abnormal SI on the CE-cine and DCE MR images of the acute and chronic MIs were compared using the paired t-test. The statistical test was two-tailed, and p values less than 0.05 were considered to indicate statistical significance.
All of the MRIs of the acute and chronic MI patients showed hyperenhancement on the DCE MRI. The areas of the acute MIs were shown as homogeneous high SI in 13 patients (Fig. 1), high SI with internal low SI in ten patients (Fig. 2), and as iso-SI in one patient on the CE-cine MRI. In contrast, the areas of chronic MI were seen as having low signal intensity on the CE-cine MRI (Fig. 3) in all patients (Table 1). In eight patients with acute MI, the end diastolic thickness of the infarcted areas was less than 6 mm, but in 16 patients, it was equal to or greater than 6 mm. For the chronic MI, the thickness of the infarcted area was less than 6 mm in all except one patient. If the height of the SI on CE-cine MRI was used as a diagnostic criterion, the sensitivity for the detection of acute MI was 95.8%. If a thickness equal to or greater than 6 mm for the acute infarcted myocardium was used as a diagnostic criterion, the sensitivity was 66.7%.
In the acute MI patients, the mean area of the abnormal SI on the CE-cine MRI (640.42 ± 321.32 mm2) was larger than the mean area of the abnormal SI on the DCE MRI (428.35 ± 310.96 mm2) (p < 0.05, paired t-test). In the chronic MI patients, the mean area of the abnormally low SI on the CE-cine MRI (106.67 ± 86.53 mm2) was smaller than the mean area of the abnormally high SI on the DCE MRI (252.36 ± 158.50 mm2) (p < 0.05).
The occurrence of chronic ischemic heart disease has increased due to the prevention of acute coronary syndromes and the reduced mortality rate from acute MI (8). However, it is not easy to localize the acute infarcted myocardium when there is clinical evidence for recurrent acute MI that underlies the chronic myocardial infarction (2). Other findings such as performing ECG and coronary angiography may not be able to localize the acute lesion. Differentiating acute from chronic irreversible myocardial injury is important for the treatment planning and follow-up after treatment. Both patterns of injury present as a regional wall motion abnormality on echocardiography, and although wall thinning is feature of chronic infarcts, this finding may not be observed on non-transmural infarcts. Both the acute and chronic MIs appear as fixed defects on radionuclide imaging. Even though DCE MR is useful and accurate for detecting myocardial infarction, it is not possible to assess the age of the infarction with using this modality (Fig. 4). There have been several recent reports demonstrating the difference of SI between acute MI and chronic scar with using T2 weighted MR imaging (2, 3).
On CE-cine MRI, the high SI of acute infarcted myocardium was documented in a previous study, and the results of our study were concordant with those of that previous study (8). This finding can be explained by the SI's dependence on the SSFP-based cine sequence (9). In acute myocardial infarction, not only the infarcted myocardium, but also the infarct-associated myocardial edema has been noted as a high signal intensity lesion on T2-weighted cardiac MR imaging. The subendocardial area of low SI surrounded by a rim of high SI in a acute myocardial infarction was thought to be an area exhibiting the microvascular phenomenon, the so-called 'no-reflow zone'. Some authors have suggested that the simultaneous assessment of myocardial function and viability is possible by performing CE-cine MR and with using the SSFP-based sequence (6, 7).
Our study showed that chronic infarcted myocardium was represented as low SI on the CE-cine MRI. This finding was not observed in the acute myocardial infarction cases. To our knowledge, this finding has not been previously reported in the literature. Based on the difference in the SI of the acute and chronic MIs, our study shows that CE-cine MR is also useful for differentiating chronic and acute MIs in the clinical setting (Fig. 4). The mechanism of this phenomenon is not clear and it needs to be explained. In our opinion, there are three possible explanations. The first mechanism is the dependence of the SI of cine MRI on the T2 SI. After the acute phase, collagen deposition is a dynamic process that starts within days after MI and it may continue for years thereafter. As the T2 relaxation times are inversely related to the amount of collagen in the muscle tissue, this results in the low SI of the myocardium on the SSFP-based sequence (6). The second possible mechanism is that there was extensive transformation of compact scar into adipose tissue. This lipomatous metaplasia was present in 68% of the cases of ischemic hearts when the hearts were excised at transplantation because of irreversible congestive heart failure (10). The area of adipose tissue may be seen as low SI on CE-cine MRI due to the chemical shift artifact. The last possible mechanism is that fibrosis can show delayed and persistent enhancement due to the delayed wash-in and wash-out of the contrast material.
As described earlier, recent studies have shown that the T2 weighted image is useful for assessing the stage of myocardial infarction (2, 3). The most important drawback of this imaging sequence is its relatively long acquisition time with multiple breath holds. One of the advantages of CE-cine MR is that it does not need additional imaging time. Because DCE MRI is obtained within 10 or 15 minutes after the administration of contrast media, the CE-cine MR can be obtained during the waiting time. In those patients with cardiac distress and severe dyspnea, the precontrast cine-MR studies can be omitted because the CE-cine MR images can also be used for the functional analysis, which would result in a further decrease of the scanning time.
In our study, the measured area of the abnormal SI on the CE-cine MRI of patients with acute MI was larger than that of the abnormal signal intensity on the DCE MRI. We believe that the discrepancy in the area of abnormal SI between the CE-cine MRI and DCE MRI can be explained by the difference in the delayed time of the imaging. The time of taking MR imaging after the Gd-DTPA injection is critical for determining the infarct size. The size of the enhanced region is known to vary according to the delay time of MR imaging after the Gd-DTPA injection (11). In one report, at 25 minutes after injection, the delayed enhancement correctly identified the infarct size. It has been suggested that Gd-DTPA could overestimate the infarct size, if it is done too soon after injection (11). The area of the abnormal SI of infarcted myocardium, as measured on the CE-cine MRI, was smaller than that seen on the DCE MRI. The reason or possible mechanism for this should be researched.
Our study has several limitations. First, the number of patients included in our study was a bit small. Even though we selected the cases in a consecutive fashion, there may have been a selection bias because of the retrospective nature of this study. Second, we did not compared the CE-cine MR images with the T2-weighted images, and this is known to be a method of choice for differentiating acute MR from chronic MI. Finally, the mechanism of the difference in the SI on the CE-cine MRI between acute MI and chronic MI was not clearly explained in the previous study, and it was also not explained in our study. Further studies are needed to solve these limitations.
In conclusion, this study showed the different SI patterns between recently infarcted myocardium and chronic scar on CE-cine MRI. In addition to the known advantages of being able to perform simultaneous assessment of myocardial function and the heart muscle viablilty for acute MI, CE-cine MRI may also be useful for differentiating acute MI from chronic MI. This method may be used as a time-effective alternative to the T2 weighted images.
Figures and Tables
Fig. 1
Both the contrast-enhanced cine (A) and delayed contrast-enhanced (B) MR images in a 71-year-old male who had a history of chest pain for three days. The images show an area of high signal intensity in the middle inferior and inferoseptal wall (arrows). Note that the area of abnormal signal intensity on the contrast-enhanced-cine MR is larger than that on the delayed contrast-enhanced MR.
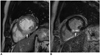
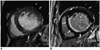
Fig. 2
The MR scan obtained on a 64-year-old male with acute myocardial infarction. The contrast-enhanced cine MR scan on the mid-diastolic phase (A) shows an area of high signal intensity with internal low signal intensity in the anterior and anteroseptal wall (arrows), and this lesion was confirmed as an area of myocardial infarction with a subendocardial no-reflow zone on the delayed contrast-enhanced MR scanning (B).

Fig. 3
The MR scan obtained in a 62-year-old male who was scheduled for coronary bypass surgery. The contrast-enhanced cine MR scan on the mid-diastolic phase (A) shows an area of low signal intensity lining the subendocardial surface of the interventricular septum (arrows). The lesion is seen as having high signal intensity on the delayed contrast-enhanced MR imaging (B).

Fig. 4
The MR scan obtained in an 87-year-old male with acute myocardial infarction and a history of chronic myocardial infarction. The contrast-enhanced cine MR scan on the mid-diastolic phase (A) shows an area of high signal intensity in the inferior wall (arrows) and an area of low signal intensity lining the subendocardial surface of the interventricular septum (arrowheads). The lesions are all seen as subendocardial infarct with high signal intensity (arrows) on the delayed contrast-enhanced MR imaging (B).
References
1. Sandstede JJ. Assessment of myocardial viability by MR imaging. Eur Radiol. 2003. 13:52–61.
2. Abdel-Aty H, Zagrosek A, Schulz-Menger J, Taylor AJ, Messroghli D, Kumar A, et al. Delayed enhancement and T2-weighted cardiovascular MRI differentiate acute form chronic myocardial infarction. Circulation. 2004. 109:2411–2416.
3. Choi SI, Lee KW, Kang SK, Ryu WH, Lim C, Chou JH, et al. Usefulness of breath-hold T2-weighted MR imaging in patients with myocardial infarction: comparison with delayed enhancement. J Korean Soc Magn Reson Med. 2003. 7:132–136.
4. Barkhausen J, Ruehm SG, Goyen M, Buck T, Laub G, Debatin JF. MR evaluation of ventricular function: True fast image with steady-state precession versus fast low angle shot cine MR imaging: Feasibility study. Radiology. 2001. 219:264–269.
5. Choi B, Choe KO, Kim Y, Chung H, Chung N, Choi D. Contrast-enhanced cine magnetic resonance imaging with balanced turbo field echo in myocardial infarction. RSNA program book. 2003. 251–252.
6. Chen Q, Storey P, Prased P, Li W, Mai V, Huang R, et al. Simultaneous imaging of myocardial function and viability. In : ISMRM 2003 Exhibition;
7. Baer FM, Voth E, Schneider CA, Theissen P, Schicha H, Sechtem U. Comparison of low-dose dobutamine-gradient-echo magnetic resonance imaging and positron emission tomography with 18F-fluorodeoxyglucose in patients with chronic coronary artery disease. A functional and morphological approach to the detection of residual myocardial viability. Circulation. 1995. 91:1006–1015.
8. Silver Malcolm D, Gotlieb A, Schoen FJ. Cardiovascular pathology. 2001. 3rd ed. Philadelphia: Churchill Livingstone;233–235.
9. Simonetti OP, Kim RJ, Fieno DS, Hillenbrand HB, Wu E, Bundy JM, et al. An improved MR imaging technique for the visualization of myocardial infarction. Radiology. 2001. 218:215–223.
10. Fuchs F, Laub G, Othomo K. True FISP-technical considerations and cardiovascular applications. Eur J Radiol. 2003. 46:28–32.
11. Winer-Muram HT, Tann M, Aisen AM, Ford L, Jennings SG, Bretz R. Computed tomography demonstration of lipomatous metaplasia of the left ventricle following myocardial infarction. J Comput Assist Tomogr. 2004. 28:455–458.
12. Oshinski JN, Yang Z, Jones JR, Mata JF, French BA. Imaging time after Gd-DTPA injection is critical in using delayed enhancement to determine infarct size accurately with magnetic resonance imaging. Circulation. 2001. 104:2838–2842.
13. Thomson RJ, Kim RJ, Judd RM. MRI for the assessment of myocardial viability. J Magn Reson Imaging. 2004. 19:771–788.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download