Abstract
Objective
To determine the diagnostic accuracy of CT arthrography and virtual arthroscopy in the diagnosis of anterior cruciate ligament and meniscus pathology.
Materials and Methods
Thirty-eight consecutive patients who underwent CT arthrography and arthroscopy of the knee were included in this study. The ages of the patients ranged from 19 to 52 years and all of the patients were male. Sagittal, coronal, transverse and oblique coronal multiplanar reconstruction images were reformatted from CT arthrography. Virtual arthroscopy was performed from 6 standard views using a volume rendering technique. Three radiologists analyzed the MPR images and two orthopedic surgeons analyzed the virtual arthroscopic images.
Results
The sensitivity and specificity of CT arthrography for the diagnosis of anterior cruciate ligament abnormalities were 87.5%-100% and 93.3-96.7%, respectively, and those for meniscus abnormalities were 91.7%-100% and 98.1%, respectively. The sensitivity and specificity of virtual arthroscopy for the diagnosis of anterior cruciate ligament abnormalities were 87.5% and 83.3-90%, respectively, and those for meniscus abnormalities were 83.3%-87.5% and 96.1-98.1%, respectively.
Magnetic resonance imaging (MRI) is the imaging modality of choice for patients with internal derangements of the knee (1-3). On the other hand, computed tomography (CT) plays only a limited role in such cases (4, 5). However, further developments in CT technology may make it one of the preferred modalities for knee imaging. The recently developed multislice CT technique provides multi-slice data acquisition with sub-millimeter slice thickness and sub-second rotation time. The axial resolution of CT images is equivalent to that of the in-plane resolution (6, 7). With such advantages, CT arthrography of the knee can provide sagittal and coronal images, just like MRI, through the process of multiplanar reformation (MPR) at high resolution (7). With high Z-axis resolution and multiplanar reformation, the diagnostic accuracy of CT arthrography for internal derangements of the knee is reported to equal that of MRI (7, 8). However, few reports have been published concerning CT arthrography using multidetector CT (7, 8). In addition, virtual arthroscopy of the knee joint can be obtained through the volume rendering of isovoxel image data sets (9). Virtual arthroscopy can be applied to preoperative planning or can be used to simulate arthroscopy for teaching purposes. However, the diagnostic accuracy or visualizing ability of virtual arthroscopy has not been validated.
In this study, we compared CT arthrography and conventional arthroscopy, in order to examine the diagnostic accuracy of multiplanar reformatted CT arthrography and virtual arthroscopy for the diagnosis of the pathology of the anterior cruciate ligament (ACL) and the menisci.
The study population consisted of 38 consecutive patients who underwent CT arthrography of the knee and subsequent conventional arthroscopy from May 2001 to October 2002. The mean interval between the CT scan and conventional arthroscopy was 27.6 days. The patients' ages ranged from 19 to 52 (mean, 24.9) years and all were male. The chief complaints were acute trauma (n=30), chronic knee joint pain (n=7) and knee joint locking (n=1).
Before CT scanning, the anterolateral aspect of the knee was punctured with an 18G needle, and 20 ml of contrast material containing 370 mg of iodine per milliliter (Ultravist 370, Shering, Berlin, Germany) was injected. If the patient had joint effusion, the fluid was drained just before injecting the contrast medium. Patients were required to 'soft walk' or perform flexion-extension movements of the knee joint for 15 minutes before the CT scan. Suprapatella bandages with an elastic band were applied to reduce the volume of the joint cavity, so as to allow sufficient contrast medium to be administered between the articular cartilage and the meniscus. Patients were scanned in the supine position and with 15 degrees flexion of the affected knee joint, so as to provide more space between the cartilage and meniscus, and around the cruciate ligament. The contralateral leg was removed from the scan field by maximum flexion of the hip and knee joint, in order to prevent the 'beam hardening' effect and to improve the image quality.
CT scans were performed with a 4-channel multislice CT scanner (Somatom Volume Zoom, Siemens, Erlangen, Germany). The parameters used were 0.5 mm collimation, a pitch value of 1, 120-kVp and 150-mA. The images were reconstructed with a slice thickness of 0.5 mm with 0.2 mm increments. The scan range was from the upper border of the patella to just below the fibular head. About 400-600 axial images were obtained from each patient.
Sagittal (Fig. 1A), coronal (Fig. 2A), and transverse MPR images were reformatted using a PC-based 3D reconstruction program (Rapidia, Infinitt, Seoul, Korea) with a thickness of 1 mm. The oblique MPR images along the course of the ACL (Fig. 3A) were additionally reformatted. The window width and center used for the MPR images were 1400 and 300, respectively.
Three radiologists (S.H.H., J.Y.C., W.L.) blinded to the arthroscopy and virtual arthroscopy results analyzed the MPR images on the computer monitor using a PC-based 3D reconstruction program, Observers 1 (S.H.H.) and 2 (J.Y.C.) were musculoskeletal radiologists experienced in the interpretation of knee MRI, but not in CT arthrography. Observer 3 (W.L.) had limited experience of knee joint MRI, but was familiar with CT arthrography. Observers 1 and 2 were introduced to the pitfalls and provided with tips on the interpretation of CT arthrographic findings by observer 3, using ten sample cases not included in the study group. The observers checked the abnormality of the ACL and both menisci. A meniscal abnormality was defined as the presence of contour irregularities, the presence of contrast material tracking into the substance of the meniscus or between the meniscus and the capsule, or the presence of discoid lateral meniscus (7). The ACL was considered to be normal if it appeared as a continuous tubular structure. The linear collection of contrast media parallel to the long axis of the ACL on the tibial side of the ACL on the sagittal and oblique coronal reformations was considered as a normal finding. An ACL abnormality was defined as a ligament discontinuity, or the presence of abnormal contours or an abnormal course. Contrast media collection on the femoral attachment side of the ACL was considered as an indication of partial tear (10). The sensitivity, specificity, positive predictive value and negative predictive value for the detection of abnormalities of the ACL and both menisci, along with their 95% confidence intervals, were obtained for each observer, and the interobserver agreements were analyzed by Kappa analysis. The strength of the interobserver agreement was determined as follows: 0.0 ≤ K ≤ 0.2, poor; 0.2 < K ≤ 0.4, fair; 0.4 < K ≤ 0.6, moderate; 0.6 < K ( 0.8, good; 0.8 < K ≤ 1.0, very good. McNemar's test was used for the statistical analysis of the difference in the values between observers. Statistical analyses were performed using GraphPad InStat version 3.05 (GraphPad Software, San Diego, CA).
Virtual arthroscopy was performed using a PC-based 3D reconstruction program (Rapidia, Infinitt, Seoul, Korea) (Figs. 1B, 2B, 3B, 4B). In the endoscopic mode, a conventional arthroscopic point of view was set up, from which the operator could control the view direction and angle by moving the view point as desired. To ensure that the entirety of the intra-articular structures was surveyed, navigation was started from six standard starting points. A radiologist familiar with the 3D reconstruction program set the six arthroscopic view starting points and adjusted the endoscopic settings, i.e., the window width and level. The six standard starting points established were: from the ACL point, the posterior cruciate ligament point, the medial meniscus anterior horn, the medial meniscus posterior horn, the lateral meniscus anterior horn and the lateral meniscus posterior horn. The radiologist who prepared the virtual arthroscopy, used multiplanar reformatted images as reference images for the purpose of positioning the standard view point and, consequently, had information of the multiplanar reformatted imaging findings, but did not know the results of the conventional arthroscopy examination. Two orthopedic surgeons (S.J.K., H.H.K.), blinded to the results of the conventional arthroscopy examination and the multiplanar reconstruction images findings, reviewed and navigated the virtual arthroscopy data on a computer monitor and made diagnoses based on these images. The sensitivity, specificity, positive predictive value and negative predictive value for the detection of abnormalities of the ACL and both menisci, along with their 95% confidence intervals, were obtained for each observer, and the interobserver agreements were analyzed by Kappa analysis.
To evaluate the visualizing ability of virtual arthroscopy, but not its diagnostic accuracy, Kappa analysis was used to evaluate the level of agreement between the CT arthrographic and the virtual arthroscopic diagnoses.
There were 8 ACL abnormalities (Fig. 4) and 24 meniscal abnormalities (Figs. 1, 2) among the 38 ACLs and 76 menisci studied by conventional arthroscopy. The ACL abnormalities were three complete tears, two near total tears, and three partial tears. Meniscus abnormalities occurred in 10 medial menisci and 14 lateral menisci. The meniscal abnormalities consisted of 21 tears of various types and three discoid lateral menisci. Other lesions found in the knee joints were one free loose body in the joint cavity, two chondral defects, and one posterior cruciate ligament tear. These other lesions were easily identified by CT arthrography, but were not included in the analysis due to their small number. The CT arthrographic sensitivity, specificity, positive predictive value and negative predictive value of each observer are summarized in Tables 1 and 2 for the ACL and the meniscus, respectively. The sensitivity and specificity of CT arthrography for the ACL abnormalities were 87.5% to 100% and 93.3 to 96.7%, respectively, and for the meniscus were 91.7% to 100% and 98.1%, respectively. The sensitivity of observers 1 and 2, who were musculoskeletal radiologists with no previous experience in the use of CT arthrography for the detection of ACL and meniscal abnormalities, was slightly superior to that of observer 3, who was familiar with CT arthrography but had limited experience with knee MRI. For the statistical analysis of the difference in sensitivities between observers 1 and 3 and between observers 2 and 3 for the detection of the ACL abnormalities, McNemar's test was used. The p-value for the difference in sensitivity for the detection of the ACL abnormalities were 0.4975 for observers 1 and 3, and 1.0 for observers 2 and 3. These differences were considered to be statistically insignificant. The interobserver agreements for the detection of the ACL and meniscal abnormalities obtained by means of the Kappa statistics are summarized in Table 3. The Kappa values were 0.622 to 0.79 for the detection of ACL abnormalities and 0.846 to 0.91 for the detection of meniscal lesions. The strengths of agreement were 'good' for the ACL abnormalities and 'very good' for the meniscal abnormalities.
The sensitivity, specificity, positive predictive value and negative predictive value of virtual arthroscopy as performed by the two orthopedic surgeons, observer 4 (S.J.K.) and 5 (H.H.K.), are summarized in Tables 4 and 5 the sensitivity and specificity of virtual arthroscopy for the ACL abnormalities were 87.5% and 83.3-90%, respectively, and for the meniscus abnormalities were 83.3%-87.5% and 96.1-98.1%, respectively. The orthopedic surgeons reported that the virtual arthroscopy images were very similar to the conventional arthroscopic view. The interobserver agreements for the detection of the ACL and meniscal abnormalities by virtual arthroscopy obtained using Kappa statistics are summarized in Table 6. The Kappa values were 0.804 for ACL abnormality detection and 0.936 for meniscal lesion detection. The strengths of agreement were 'very good' for both the ACL abnormalities and meniscal abnormalities.
The agreement between virtual arthroscopy and CT arthrography for the detection of the ACL and meniscal abnormalities was assessed using the Kappa statistics of the CT arthrographic findings of observer 3, who prepared the virtual arthroscopy, and the virtual arthroscopic findings of observers 4 and 5.
The Kappa values were 0.732 (observers 3 and 4) and 0.773 (observers 3 and 5) for the detection of the ACL abnormalities, and 0.938 (observer 3 and 4) and 0.936 (observer 3 and 5) for the detection of the meniscal lesions. The strengths of agreement for virtual arthroscopy and CT arthrography were 'good' for the ACL abnormalities and 'very good' for the meniscal abnormalities. The visualizing ability of virtual arthroscopy was thought to be excellent for meniscal lesions and good for ACL lesions.
Recent developments in CT technology have led to increased scan speed, improved coverage volume, and especially to high temporal and spatial resolution (6). The value of CT arthrography lies mainly in its multiplanar reconstruction capacity. Sagittal and coronal reconstruction images are very similar to the views provided by MR imaging. The diagnostic value of CT arthrography for abnormalities affecting the menisci and ACLs has been reported to be equivalent to that of MR imaging in most studies (7, 8, 10-12).
CT arthrography has some unique pitfalls, however, which are not encountered in MR imaging (8). One example of this involves the analysis of the synovial fold around the meniscus and the ACL (Fig. 3A). Tissue contrasts in MR are obtained from the unique signal intensity (SI) of a chemical component, and the normal meniscus has a dark SI and good tissue contrast against the surrounding synovial fat tissue. However, in the case of CT arthrography, the contrast is mainly obtained from the high attenuation of the intra-articular contrast media and the low attenuation of the soft tissue. The high attenuation of bone is another distinguishing feature in CT arthrography of the knee. The fundamental differences between these tissue contrasts must be understood before assessing CT arthrography, in order to avoid certain pitfalls. The synovial fold can mimic meniscal tears and ACL tears, but with some experience and an appropriate introduction to the technique, the differential diagnosis of a normal synovial fold from a true meniscal or ligament tear is quite straightforward. It can be helpful when assessing the findings of CT arthrography to consider the remaining tissue contrast between fat and the cartilage or ligament, given the use of an optimal window width and level settings (Fig. 2A). In our study, the musculoskeletal radiologist, who had no prior experience in CT arthrography, showed good diagnostic accuracy after being given a brief explanation of these pitfalls. One strong point of CT arthrography versus MRI is its excellent delineation of the articular cartilage between the cortical bone and the contrast media in the joint cavity. Another good point of CT arthrography is that the differentiation of a true meniscal tear from the internal degeneration of the meniscus is straightforward. CT arthrography reveals only the space accessed by the contrast media, and thus the intra-meniscal pathology is not shown.
The diagnostic accuracies of CT arthrography were excellent in the present study and were equivalent to those obtained in most MR imaging (11, 12) and CT arthrography (7, 10) studies. The diagnostic accuracy achieved in this study by the radiologists with no experience in CT arthrography demonstrates that the findings of CT arthrography are easy to assess and that its learning curve may be shorter than that of MRI.
CT had a limitation in terms of the delineation of structures outside the synovial cavity, such as that of the collateral ligament and the posterior cruciate ligament (PCL). In the patients examined in this study, medial collateral ligament (MCL) tears could be recognized by CT arthrography in some cases by a contrast media leak in the area of the MCL and a thickening of the MCL. However, no gold standard for the identification of collateral ligament injury was evident. The diagnostic accuracy of CT arthrography for collateral ligament abnormalities was not evaluated. The PCL is partially located in the synovial cavity. We had one confirmed PCL injury and, in this case, the PCL tear was evident when examined by CT arthrography and by virtual arthroscopy. The PCL can easily be recognized by the tissue contrast that is observed between the fat and the ligament, even in segments lying outside the joint cavity. There is always a possibility of detecting PCL lesions by CT arthrography, but we did not perform an analysis on the PCL, due to the small number of PCL lesions, and the lack of a gold standard for confirming the absence of PCL abnormalities. Arthroscopists do not always investigate the PCL, unless there is a clinical suspicion of PCL injury.
Virtual arthroscopy is based on CT arthrography and can be viewed as an alternative method of presenting CT arthrographic findings. Thus, the diagnostic accuracy of virtual arthroscopy was good for the meniscal lesions, but not as good for the ACL lesions. The outer margin of the torn ACL was not clear, unlike in the case of the meniscal tear, and the differentiation between a redundancy of the ACL and a partial tear was not easy; moreover, the femoral side of the ACL was difficult to navigate by virtual arthroscopy. However, the high agreement between CT arthrography and virtual arthroscopy in this study demonstrated the good visualizing ability of virtual arthroscopy. Most meniscal lesions seen on MPR images can be presented as virtual arthroscopy images, which are more familiar to the arthroscopist than to the radiologist. These intuitive and realistic images are helpful to the arthroscopist and can be used for simulated examinations before performing the more invasive conventional arthroscopy. Such a simulation of arthroscopy is thought to be useful both for pre-operative planning and as an educational method (13, 14). If the virtual arthroscopy image can be fused with a haptic model of arthroscopy simulation, realistic preoperative case-by-case simulations may be possible in the future (14). The present study demonstrates that virtual arthroscopic images are very similar to those of conventional arthroscopy. Thus, our results can be used for basic studies on the clinical applications of virtual arthroscopy.
Preparing the routine view for virtual arthroscopy is operator dependant, because the 3D rendering program has not yet been fully automated. Routine view images set by a radiologist may represent the radiologist's diagnosis. Actually, the diagnosis obtained by virtual arthroscopy was found to correlate well with that obtained from MPR images, which is evidence of the good visualizing ability of virtual arthroscopy.
The patients included in the present study were all young healthy male soldiers. Thirty of the 38 patients had a history of acute trauma. This biased study population may have increased the sensitivity and specificity of our study, because examinations of young male patients with acute trauma usually show excellent image quality. The small number of patients involved also limits our results, and the lack of a comparison with MRI is a substantial limitation. Thus, to fully assess the diagnostic accuracy of CT arthrography, the meniscus, ACL, collateral ligaments and PCL should be subjected to a comparative study with MRI.
Even though CT arthrography is more invasive, because of the intra-articular injection of contrast material and of the use of ionizing radiation, CT is usually easier to access than MR in most situations, and the cost of CT is lower than that of MRI. Thus, CT arthrography may offer a good alternative for the assessment of internal knee derangements, since the diagnostic accuracy of multiplanar reformatted CT arthrography for ACL and meniscal abnormalities and the virtual arthroscopic expression of meniscal lesions are excellent.
Figures and Tables
Fig. 1
Medial meniscus tear in a 28-year-old man with knee pain after trauma.
A. Sagittal CT image clearly demonstrating an oblique tear of the medial meniscus (arrow).
B. Virtual arthroscopy of the medial meniscus showing cleavage (arrow) and a rugged free margin of torn meniscus (arrowheads). The tibial plateau (asterisk) and femur condyle (curved arrow) are also shown.

Fig. 2
CT arthrography and virtual arthroscopy of the lateral meniscus tear of a 29-year-old man with knee joint pain.
A. Coronal CT arthrography showing a vertical and horizontal tear of the lateral meniscus (arrow). Note the intact medial collateral ligament (arrowheads).
B. Virtual arthroscopy showing cleavage of the meniscus (arrow) and a displaced meniscus central segment (arrowhead). The tibia plateau (asterisk) and femur condyle (curved arrow) are clearly demonstrated.

Fig. 3
CT arthrography of the normal anterior cruciate ligament of a 27-year-old male.
A. Oblique coronal CT arthrography showing a well demarcated linear anterior cruciate ligament (arrowheads). The small amount of contrast media on the tibial side was considered a normal finding (arrow).
B. Virtual arthroscopic view of the normal anterior cruciate ligament (arrow). The smooth margin and continuity to the intercondylar notch are clearly demonstrated (arrowheads).
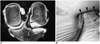
Fig. 4
A tear in the anterior cruciate ligament of a 20-year-old man with knee joint pain after trauma
A. Arthroscopy showing a rugged torn fiber of the anterior cruciate ligament. One arthroscopist judged that there was a 50% partial tear of the anterior cruciate ligament. The ridge of the intercondylar notch (arrowheads) and the torn anterior cruciate ligament (arrow) are shown.
B. Virtual arthroscopy showing an anterior cruciate ligament with abnormal shape and orientation. The ridge of the intercondylar notch is shown (arrowheads). The anterior cruciate ligament has lost its normal continuity and has an irregular torn margin (arrow).

Table 1
Sensitivity, Specificity, Positive Predictive Value and Negative Predictive Value of CT Arthrography for the Detection of Anterior Cruciate Ligament Abnormalities

Table 2
Sensitivity, Specificity, Positive Predictive Value and Negative Predictive Value of CT Arthrography for the Detection of Meniscal Abnormalities

Table 3
Interobserver Agreement for the Detection of Anterior Cruciate Ligament Abnormalities and Meniscal Abnormalities by CT Arthrography, Evaluated Using Kappa Statistics

Table 4
Sensitivity, Specificity, Positive Predictive Value and Negative Predictive Value of Virtual Arthroscopy for the Detection of Anterior Cruciate Ligament Abnormalities

References
1. Tavernier T, Dejour D. Knee imaging: what is the best modality. J Radiol. 2001. 82:387–408.
2. Crues JV III, Mink J, Levy TL, Lotysch M, Stoller DW. Meniscal tears of the knee: accuracy of MR imaging. Radiology. 1987. 164:445–448.
3. Mink JH, Levy T, Crues JV III. Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology. 1988. 167:769–774.
4. Ghelman B. Meniscal tears of the knee: evaluation by high-resolution CT combined with arthrography. Radiology. 1985. 157:23–27.
5. Malghem J, Vande Berg BC, Lebon C, Lecouvet FE, Maldague BE. Ganglion cysts of the knee: articular communication revealed by delayed radiography and CT after arthrography. AJR Am J Roentgenol. 1998. 170:1579–1583.
6. Berland LL, Smith JK. Multi detector-array CT: once again, technology creates new opportunities. Radiology. 1998. 209:327–329.
7. Vande Berg BC, Lecouvet FE, Poilvache P, et al. Dual-detector spiral CT arthrography of the knee: accuracy for detection of meniscal abnormalities and unstable meniscal tear. Radiology. 2000. 216:851–857.
8. Vande Berg BC, Lecouvet FE, Poilvache P, Maldague B, Malghem J. Spiral CT arthrography of the knee: technique and value in the assessment of internal derangement of the knee. Eur Radiol. 2002. 12:1800–1810.
9. Irie K, Yamada T. Three-dimensional virtual computed tomography imaging for injured anterior cruciate ligament. Arch Orthop Trauma Surg. 2002. 122:93–95.
10. Vande Berg BC, Lecouvet FE, Poilvache P, Dubuc JE, Maldague B, Malghem J. Anterior cruciate ligament tears and associated meniscal lesions: assessment at dual-detector spiral CT arthrography. Radiology. 2002. 223:403–409.
11. Rubin DA. MR imaging of the knee menisci. Radiol Clin North Am. 1997. 35:21–44.
12. Heron CW, Calvert PT. Three-dimensional gradient-echo MR imaging of the knee: comparison with arthroscopy in 100 patients. Radiology. 1992. 183:839–844.
13. Pedowitz RA, Esch J, Snyder S. Evaluation of a virtual reality simulator for arthroscopy skills development. Arthroscopy. 2002. 18:29E.
14. Mabrey JD, Gillogly SD, Kasser JR, Sweeney HJ, Zarins B, Mevis H. Virtual reality simulation of arthroscopy of the knee. Arthroscopy. 2002. 18:28E.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download