Abstract
Objective
To assess the utility of hysterosonography (HS) as a screening method in patients with abnormal uterine bleeding.
Materials and Methods
We retrospectively reviewed transvaginal ultrasonography (TVS) and HS for 105 patients whose diagnosis was confirmed pathologically. All 105 patients were initially evaluated on the same day with both TVS and HS. On TVS and HS examination, endometrial cavitary lesions were classified as diffuse hyperplasia, endometrial polyp, endometrial cancer, uterine synechia and submucosal leiomyoma. Hysteroscopy with biopsy (n=35), curettage (n=60) or hysterectomy (n=10) was performed, and the results of TVS and HS examination were correlated with the pathological findings.
Results
The sensitivity and specificity were 79.0% and 45.8% for TVS, and 95.1% and 83.3% for HS, respectively. The positive and negative predictive values were 83.0% and 39.3% for TVS, and 95.1% and 83.3% for HS, respectively. Twenty-seven showed a discrepancy between the TVS and HS, and eight cases showed a discrepancy between HS and the pathologic diagnosis.
Conclusion
TVS is a sensitive method to evaluate the endometrial cavitary lesions, but it often does not provide the physician with sufficient diagnostic information. With its higher sensitivities, specificities and positive and negative predictive values, HS can be better used than TVS in evaluating those patients with abnormal uterine bleeding.
Abnormal uterine bleeding is a common problem of perimenopausal or postmenopausal women (1). The causes can be variable, from simple dysfunctional uterine bleeding without any organic cause to the endometrial cancer. Because 10% to 15% of postmenopausal vaginal bleeding is due to endometrial carcinoma, these symptoms should be thoroughly evaluated (1-5). For the evaluation of this condition, invasive procedures such as hysteroscopy and curettage are commonly used.
For the evaluation of abnormal uterine bleeding, transvaginal ultrasonography (TVS) plays an important role as the initial modality (2, 3). It is widely accepted that hysterosonography (HS) is the method of choice for the evaluation of the endometrial pathology (6-11). During the last several years we had frequently experienced cases in which TVS showed a normal evaluation, but HS showed endometrial pathology, and there are cases in which TVS suggested an endometrial lesion, but HS showed no organic abnormality. We postulated that TVS is limited in its ability for screening the lesions within the endometrial cavity for patients with abnormal uterine bleeding, and that HS can be used as a screening method in those cases. In this study, we attempted to evaluate the usefulness of HS as a screening method for patients with abnormal uterine bleeding by comparing TVS and HS findings with pathologic findings.
Four hundred and fourteen women presented in our institution with abnormal uterine bleeding between July 1996 and February 2002. We included only the patients with technical success in TVS and HS in this study. Finally, 105 patients with pathologic confirmation were included in this study. The patient's ages ranged from 27 to 73 years (average, 44.3 years old). Forty-seven women were postmenopausal and 58 were premenopausal. All 105 patients were first evaluated on the same day with TVS followed by HS. Within two days following TVS and HS, hysteroscopy with biopsy (n=35) or curettage (n=60) was performed in 95 patients. Hysterectomy was performed in ten patients within one month. The pathological findings were then correlated with US findings.
All ultrasonographic examinations using both TVS and HS were performed with 7-8 MHz intracavitary end-fire transducers (HDI 3000, Advanced Technology Laboratories, Bothell, WA, U.S.A. and GE LOGIQ 700 MR, GE Medical System, Milwakee, WI, U.S.A.).
Two gynecologic radiologists performed the ultrasonographic examinations; in TVS examinations, the uterus was scanned in the sagittal and coronal planes. The double-layer endometrial thickness was measured at the widest point between the endometrial-myometrial interfaces in the sagittal plane by using electronic calipers. If there was fluid in the endometrial cavity, the anterior and posterior walls of the endometrial cavity were measured separately, and the measurements were then added to obtain the endometrial thickness. The presence of focal endometrial thickening or a focal mass was noted.
The HS examinations were performed using the conventional technique (12, 13). A sterile double-bladed metal speculum was inserted into the vagina, and the cervix was cleaned with povidone-iodine solution. The 6 Fr- pediatric urine catheter (Sewoon Medical, Seoul, Korea) was inserted into the external cervical os, and the balloon was inflated with 4-8 ml of the saline to seal the external os tightly to prevent any leakage into the vagina. The speculum was removed and the probe was reinserted into the vagina, and then the sterile saline was slowly injected. A small amount of saline was injected early in the examination to avoid excessive cramping and discomfort of the patient, and the fluid slowly filled the cavity completely. During the HS examination, the presence or absence of focal endometrial lesion as well as endometrial thickness were also evaluated (Fig. 1).
Two radiologists, who were kept unaware of the pathologic diagnoses and clinical data of the patients, interpreted the ultrasonography images in a random order. We observed the endometrial abnormalities on all the images of TVS and HS by using picture archiving and communication system. The ultrasonographic images were analyzed by a consensus. On the TVS examination, the endometrium was regarded as abnormal if it was equal to or thicker than 15 mm in the premenopausal period, and equal to or thicker than 8 mm in the postmenopausal period. On the HS examination, the endometrium was regarded as abnormal if it was equal to or thicker than 8 mm in the premenopausal period and in a postmenopausal patient on hormone replacement therapy. The HS examination was regarded as abnormal if the endometrium was equal to or thicker than 5 mm in a postmenopausal patient who was not on hormone replacement therapy, when the thickness of both layers were added (14).
The size of the focal abnormality was also measured. On TVS and HS examination, endometrial lesions were classified as diffuse thickening, focal thickening suggestive of endometrial polyp, endometrial cancer, uterine synechia and submucosal leiomyoma. The sensitivities, specificities, and positive and negative predictive values of the TVS and HS examinations were calculated.
Pathologic examination revealed the presence of 37 endometrial polyps (35%) (Figs. 2, 3), 26 submucosal leiomyomas (25%) (Fig. 4), 12 endometrial hyperplasia (11%), three endometrial carcinomas (3%) and two adenomyomas (2%) (Fig. 5). One patient had uterine synechia, and twenty-four of 105 patients (23%) showed no organic cause for uterine bleeding (Table 1).
Out of the 105 patients, 77 patients had abnormal findings on the TVS examination, and 64 of the 77 patients had positive pathologic findings (positive predictive value=83%). 28 patients showed normal findings on the TVS examination, and 11 of them had normal findings on the pathology tests (negative predictive value=39%). In spite of normal looking TVS examinations, 17 of the patients had pathological abnormalities. Thirteen patients had suspicious abnormalities on the TVS examinations, but no abnormality was demonstrated on pathology.
For the comparison of HS to pathology, 81 patients had abnormal endometrial findings on the HS examination, and 77 of the 81 patients had positive pathologic findings (positive predictive value=95%). Twenty-four patients showed normal endometrial findings on the HS examinations, and 20 of the 24 patients had normal finding on the pathology tests (negative predictive value=83%).
The sensitivity and specificity of TVS were 79.0% and 45.8%, respectively (Table 2). The false negative cases included six hyperplasia, four small polyps of less than 5 mm in size, three submucosal leiomyomas, two adenomyomas (falsely considered as intramural lesions), a case of synechia and a case of chronic endometritis. The six false-positive lesions demonstrated focal thickening of the endometrium (Fig. 6), which include a case of diffuse thickening, four cases of endometrial polyps and a case with suspected submucosal leiomyomas.
The sensitivity and specificity of HS were 95% and 83%, respectively. The false negative cases include two cases of diffuse hyperplasia, one case of submucosal leiomyoma and a case of chronic endometritis. The submucosal leiomyoma was about 6 cm in diameter, and it was misdiagnosed as intramural leiomyoma during the HS examination. The false positive cases included two cases with diffuse hyperplasia, an intramural leiomyoma and a case of hemorrhagic debris falsely diagnosed as an endometrial tumor. The 27 cases showing a discrepancy between TVS and HS diagnosis and eight cases showing a discrepancy between HS examination and pathologic diagnosis were analyzed and summarized in Table 3 and Table 4.
TVS has been the first choice modality for the evaluation of the endometrium during the last two decades. HS has recently been widely used for the more thorough evaluation of endometrial lesions (2-8). Some investigators have attempted to assess the diagnostic values of HS examination by correlating and comparing it with pathologic and hysteroscopic findings (9-11). In the previous literature the combination of TVS and HS examination has been proved to be more accurate and cost-effective than hysteroscopy with biopsy (6, 9). The sensitivity and specificity of HS examination have been reported to be as high as 85-91% and 83-100%, respectively (6, 7, 10). In a more recent study, 14% of 114 patients showing normal TVS findings revealed abnormalities upon HS examination (14). However, the study was limited to those patients with normal TVS findings and there has not been any extensive study for actually evaluating the role of HS as a screening method for patients with abnormal uterine bleeding.
As in the previous literature (9), our study also found that TVS was quite a sensitive method to evaluate the abnormal uterine bleeding, with high sensitivity (79%) and positive predictive value (83%). However, it has its limitations in depicting small nodular lesions, which are isoechoic within the endometrium, and even a normal thickness endometrium may be seen to represent endometrial hyperplasia. In our study, small endometrial polyps or submucosal leiomyomas (usually less than 15 mm sized) could not be correctly detected with TVS. Even large adenomyoma and synechia could not be diagnosed either. TVS also cannot differentiate submucosal from intramural leiomyoma in many instances, which is an important distinction for the physician to consider for the treatment planning (8, 11). Owing to its ability to demonstrate small endometrial lesions, HS can be used as a method of choice to evaluate those patients with abnormal uterine bleeding. Our results indicate that one should not hesitate to perform an HS examination for patients with abnormal uterine bleeding, even if these patients are found to have normal TVS findings.
We found 27 cases showing a discrepancy between the findings of TVS and HS and eight cases showing a discrepancy between HS findings and pathologic diagnosis (Table 3, 4). In the 27 cases, HS could not find two endocavitary lesions, one submucosal myoma and the other intramural myoma. The two myomas were detected on both HS and TVS examination, but the locations were incorrectly diagnosed with HS. In some cases the differentiation between endometrial polyp and polypoid adenomatoid hyperplasia was difficult. However, HS had successfully detected these lesions that could not be found in TVS in sixteen cases, including an atypical adenomyoma and the uterine synechia. In addition, HS could exclude the nine pseudolesions seen with TVS, and this resulted in the avoidance of any unnecessary intervention or possible surgery. As a result of using two modalities for diagnosis, in 105 cases, 25 patients saw their physicians change the treatment plan after HS.
Out of the eight cases showing a discrepancy between HS findings and pathologic diagnosis, HS could not diagnose chronic endometritis in one patient, and two cases of endometrial hyperplasia showed as normal endometrial thickness. Another two cases were misdiagnosed as endometrial hyperplasia, because the endometrium was diffusely thickened upon HS after an adequate instillation of saline, with the endometrial walls measuring 8 mm and 10 mm in thickness, respectively. A case that was misdiagnosed as an endometrial polyp upon HS examination was found to have attached hemorrhagic debris in the endometrial cavity during hysteroscopy and on the pathology tests. The two cases of myomas were misdiagnosed with HS and correctly diagnosed in TVS.
One of the limitations of this study was that the TVS or HS findings were only correlated with pathologic results and not with the hysteroscopic findings. This was because hysteroscopy was not performed for every patient. Endometrial hyperplasia and hyperplastic polyps could not be easily distinguished with the biopsy specimen alone, and a small focal abnormality sometimes could not be matched on biopsy. Another limitation is that we could not apply the normal limits of endometrial thickness according to the menstrual phase in all of the premenopausal women because their exact menstrual periods were not known. Some cases of endometrial hyperplasia falsely diagnosed as being negative on TVS and HS examination could have been better diagnosed if the menstrual phase were considered. Also, the pathologic evaluation in some cases was not sufficient because of too small a biopsy specimen was obtained to differentiate endometrial hyperplasia from polyps. Finally, we did not consider any other aspects of HS examinations as a screening method, including costeffectiveness, consumption of time, patient's discomfort and the effects on treatment. Further investigations in this regard are needed in the future.
In conclusion, TVS is a sensitive method to evaluate the endometrial cavitary lesions, but often this modality does not provide the physician with sufficient diagnostic information. With higher sensitivities, specificities, and positive and negative predictive values, HS can be better applied than TVS for evaluating patients with abnormal uterine bleeding.
Figures and Tables
Fig. 1
A 42-year-old woman presented with dysmenorrhea and frequent vaginal spotting.
A. Longitudinal image of transvaginal ultrasonography shows a thin smooth endometrium without any focal lesion.
B. Longitudinal image of hysterosonography shows no abnormality of the endometrium. A small amount of debris in the endometrial cavity and a scar from previous Caesarean section in the anterior wall of the isthmic portion are seen.

Fig. 2
A 45 year-old woman presented with abnormal uterine bleeding.
A. Longitudinal image of transvaginal ultrasonography shows an extremely thickened endometrium and multiple cystic portions in the mass.
B. Longitudinal image of hysterosonography shows a huge endometrial tumor, which was regarded as a polyp.
C. T2-weighted sagittal image of the uterus shows about a 9 cm sized heterogeneous hyperintense mass confined in the endometrial cavity. Hysteroscopic removal was done and the diagnosis of endometrial polyp was confirmed in pathology.

Fig. 3
A 48 year-old premenopausal woman presented with menorrhagia and dysfunctional uterine bleeding.
A. Longitudinal image of transvaginal ultrasonography shows a homogeneously hyperechoic 12-mm-thick endometrium without any focal lesion, which looks normal.
B. Longitudinal image of hysterosonography shows an elongated endometrial mass (arrows), which was regarded as endometrial hyperplasia. Curettage biopsy was done and an endometrial polyp was confirmed upon pathologic examination.
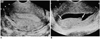
Fig. 4
A 37 year-old premenopausal woman presented with menorrhagia and dysfunctional uterine bleeding.
A. Longitudinal image of transvaginal ultrasonography shows an intramural leiomyoma (arrows).
B. Longitudinal image of hysterosonography shows a lobulated mass in a submucosal location (arrows).
C. Upon hysterosalpingography, an intracavitary filling-defect (arrows) is seen. The diagnosis of leiomyoma was confirmed in pathology.

Fig. 5
A 48 year-old premenopausal woman presented with dysfunctional uterine bleeding.
A. Longitudinal image of transvaginal ultrasonography shows hematometra with a fluid-debris level, and a cervical stenosis is suspected. A thin endometrium (arrows) is seen, which looks normal.
B. Longitudinal image of hysterosonography shows a large endometrial mass, which is near totally necrotic. Total hemorrhagic degeneration of a submucosal myoma was suspected. Hysterectomy was done and adenomyoma was confirmed with pathology testing.

Fig. 6
A 58 year-old postmenopausal woman presented with vaginal spotting.
A. Longitudinal image of transvaginal ultrasonography shows a small hyperechoic nodule (arrows) in the endometrium. It was regarded as a small polyp.
B. Longitudinal image of hysterosonography shows a thin endometrium without any focal lesion. On the 1 month follow-up transvaginal ultrasonography, the small nodule disappeared and the vaginal spotting disappeared as well.

Table 2
Comparison of TVS and HS with Pathologic Diagnosis for Patients with Abnormal Uterine Bleeding

References
1. Bree RL, Bowerman RA, Bohm-Velez M, et al. US evaluation of the uterus in patients with postmenopausal bleeding: A positive effect on diagnostic decision making. Radiology. 2000. 216:260–264.
2. Dubinsky TJ, Parvey HR, Maklad N. The role of transvaginal sonography and endometrial biopsy in the evaluation of peri- and postmenopausal bleeding. AJR Am J Roentgenol. 1997. 169:145–149.
3. Fleischer AC. Sonographic assessment of endometrial disorders. Semin Ultrasound CT MR. 1999. 20:259–266.
4. Lee EJ, Lee HM, Kwon HC, Joo HJ. Usefulness of sonohysterography in the differentiation of endometrial and endometrial cavity abnormalities: comparison with transvaginal sonography. J Korean Soc Med Ultrasound. 1995. 14:175–181.
5. Lee EJ, Kim JM, Ryu HS. Usefulness of sonohysterography in differentiating endometrial cancer from endometrial hyperplasia. J Korean Soc Med Ultrasound. 1999. 18:91–97.
6. Saidi MH, Sadler RK, Theis VD, Akright BD, Farhart SA, Villanueva GR. Comparison of sonography, sonohysterography, and hysteroscopy for evaluation of abnormal uterine bleeding. J Ultrasound Med. 1997. 16:587–591.
7. O'Connell LP, Fries MH, Zeringue E, Brehm W. Triage of abnormal postmenopausal bleeding: a comparison of endometrial biopsy and transvaginal sonohysterography versus fractional curettage with hysteroscopy. Am J Obstet Gynecol. 1998. 178:956–961.
8. Laifer-Narin SL, Ragavendra N, Lu DS, Sayre J, Perrella RR, Grant EG. Transvaginal saline hysterosonography: characteristics distinguishing malignant and various benign conditions. AJR Am J Roentgenol. 1999. 172:1513–1520.
9. Bree RL. Ultrasound of the endometrium: facts, controversies, and future trends. Abdom Imaging. 1997. 22:557–568.
10. Timmerman D, Deprest J, Bourne T, Van den Berghe I, Collins WP, Vergote I. A randomized trial on the use of ultrasonography or office hysteroscopy for endometrial assessment in postmenopausal patients with breast cancer who were treated with tamoxifen. Am J Obstet Gynecol. 1998. 179:62–70.
11. Becker E Jr, Lev-Toaff AS, Kaufman EP, Halpern EJ, Edelweiss MI, Kurtz AB. The added value of transvaginal sonohysterography over transvaginal sonography alone in women with known or suspected leiomyoma. J Ultrasound Med. 2002. 21:237–247.
12. Cullinan JA, Fleischer AC, Kepple DM, Arnold AL. Sonohysterography: a technique for endometrial evaluation. RadioGraphics. 1995. 15:501–514.
13. Sohaey R, Woodward P. Sonohysterography: technique, endometrial findings, and clinical applications. Semin Ultrasound CT MR. 1999. 20:250–258.
14. Laifer-Narin S, Ragavendra N, Parmenter EK, Grant EG. False-normal appearance of the endometrium on conventional transvaginal sonography: comparison with saline hysterosonography. AJR Am J Roentgenol. 2002. 178:129–133.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download