Abstract
Objective
The purpose of this study was to evaluate the MR spectrum and MR cholangiographic imaging findings of clonorchiasis.
Materials and Methods
We reviewed 26 patients with confirmed clonorchiasis by either stool tests (n=24) or surgery (n=2). MR imaging was performed on a 1.5 T system (GE Medical Systems, Milwaukee, WI) with a torso coil. Axial T1- and T2-weighted, gadolinium-enhanced dynamic images and MR cholangiography were obtained. Image analyses were used to identify abnormalities of the intrahepatic and extrahepatic bile ducts and the presence of hepatobiliary malignancy. All MR examinations were reviewed by the consensus of two abdominal radiologists.
Results
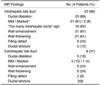
Intrahepatic bile duct abnormalities were seen in 23 (89%) of the 26 patients. The most common finding was mild dilatation of the intrahepatic bile duct which was found in 21 (81%). "Too many intrahepatic ducts" were found in 16(62%), wall enhancement and thickening in 21 (81%) and filling defects and ductal stricture in the intrahepatic bile duct in 6 (24%) and 3 (12%) patients, respectively. Extrahepatic ductal dilation was found in 5 (19%) and 9 (35%) revealed hepatobiliary malignancy.
Clonorchiasis is an important parasitic disease of the bile ducts caused by chronic infestation of Clonorchiasis sinensis following ingestion of raw freshwater fish flesh in East and South-east Asia (1, 2). Clonorchiasis is one of the most frequent causes of cholangiocarcinoma and cholangitis in endemic countries, and therefore its early diagnosis is critical for the prevention of complications (3-5).
Several reports have described the radiological features of clonorchiasis on cholangiography, ultrasonography and CT (6-10). MR imaging has been used in the diagnosis of various diseases of the biliary system, and MR cholangiography (MRC) is a relatively new noninvasive type of imaging for evaluation of the extrahepatic biliary pathology (i.e. strictures, stones, and obstruction). MR cholangiography is generally comparable with endoscopic retrograde cholangiopancreatography (ERCP) for the demonstration of segmental and peripheral intrahepatic bile ducts, and may show intrahepatic ductal abnormalities in a comparable fashion to that of ERCP (11-14). To our knowledge, only one radiological report has briefly reviewed the MR findings of clonorchiasis (15). The purpose of our study was to evaluate the MR imaging and MRC findings of clonorchiasis.
From the medical records between January 1998 and June 2002 26 patients with either positive stool examination (n=24) or surgery (n=2) for Clonorchiasis sinensis that underwent abdominal MR imaging were entered into this study. The patients included 16 men and 10 women, with ages ranging from 19 to 76 years old, with a mean of 42 years. Nine patients had undergone ERCP. The reasons for the MR imaging were as follows: evaluation of bile duct dilation detected at ultrasonography, evaluation of liver mass detected at CT or ultrasonography and clarification of undetermined abnormalities at ERCP in 18, 5 and 3 cases, respectively. The clinical symptoms were usually nonspecific, with the exception of 5 cases with jaundice. The serum bilirubin levels and serum alkaline phosphatase concentrations of 5 and 7 cases, respectively, were elevated.
MR imaging was performed on a 1.5T system (Signa Horizon, GE Medical Systems, Milwaukee, WI) using a phased array torso coil. T1-weighted images were acquired using a conventional spin-echo (TR range/TE range, 400-600/7-15) sequence in 11 patients, and an in-phase gradient-recalled echo (GRE) (TR/TE/flip angle=120/4.2/90°) sequence, and an opposed phase GRE sequence (TR/TE/flip angle=120/1.8/90°) in 15. The GRE images were obtained using fast multiplanar spoiled gradient-recalled acquisition. T2-weighted images were obtained with fast spin-echo (FSE, TR range/effective TE=3,000-7,000/104) sequences in seven patients, and a single shot fast spin-echo (SSFSE, TR/effective TE=∞/92) sequence in 19. The imaging matrix number was 256×128 or 192 for FSE and GRE sequences, usually using a rectangular field of view to reduce the number of phase-encoding views. The sampling bandwidth was 64 kHz (±32 kHz) for the FSE sequence, with section thicknesses of 8 mm and a section gap of 2 mm or less. In 21 patients, MRC was performed in thick slab SSFSE sequence (TR/TE/slice thickness=∞/800/40 mm) and coronal thin slice SSFSE sequence (TR/TE/slice thickness=∞/180/4 mm). Thick slab images were obtained in the coronal plane and multiple oblique planes. In 24 patients, echo fast gradient echo 3D images (TR/TE/Flip angle, 7-9/2-3/15°), with spectral fat saturation, were obtained before and after administration of gadopentetate dimeglumine (Magnevist, Berlex, Wayne, NJ). After acquiring unenhanced images, 0.1 mmol/kg of contrast material was injected intravenously, as a rapid bolus, followed by 10 ml of normal saline flush. The images were obtained at 30-45 sec (arterial phase), 70-90 sec (portal venous phase) and 3-5 min (delayed phase) after the contrast injection. In 19 patients, both multiphasic contrast-enhanced dynamic imaging and MRC were performed.
All the MR examinations were reviewed by two abdominal radiologists, with final conclusions reached by means of consensus. Image analyses were performed to identify abnormalities of the intrahepatic and extrahepatic bile ducts and the presence of hepatobiliary malignancy. For abnormalities of the intrahepatic ducts, the ductal dilation, "too many intrahepatic ducts" sign, wall thickening, wall enhancement, ductal stricture and filling defects were assessed. Intrahepatic ductal dilation was diagnosed when the ductal diameter was greater than 3 mm or if the ducts were seen in the peripheral portion of the liver (16, 17). The criteria for intrahepatic bile duct dilation were as follows: mild, dilated, but identified as an individual structure; marked massive dilation (greater than 10 mm), with individual ducts difficult to identify (18). "Too many intrahepatic ducts" sign was defined as diffuse, uniform dilatation of the small intrahepatic bile ducts, tertiary, quaternary or more peripheral ducts on MRC (6, 10). Wall enhancement was assessed subjectively, and was defined as having higher signal intensity than the adjacent hepatic parenchyma on contrast-enhanced, delayed phase imaging. Wall thickening of the intrahepatic bile duct was defined as a wall thickness of 1.5 mm or more, using electronic calipers on a PACS monitor (18). Stricture was defined as a focal caliber change present in any segment. On abnormalities of the extrahepatic bile duct, ductal dilation was considered present when the duct was dilated greater than 8 mm (19). The ducts were considered mildly and markedly dilated when the diameters were 8-10 mm or greater than 11 mm, respectively. Wall thickening was defined as a thickness of 1.5 mm or more (18). Associated hepatobiliary malignancies, such as cholangiocarcinoma and hepatocellular carcinoma, were also evaluated.
In nine patients that had undergone ERCP, the abnormal findings of the intrahepatic and extrahepatic bile ducts (ductal dilatation, "too many intrahepatic ducts" sign, stricture, and filling defect) were retrospectively reviewed by the same two radiologists, with no prior knowledge of the patients' clinical information and MR findings.
The MR findings of the patients with clonorchiasis are summarized in Table 1. Intrahepatic bile duct abnormalities were seen in 23 (89%) of the 26 patients. The most common finding was mild dilation of the intrahepatic bile duct, which was present in 21 (81%) patients. "Too many intrahepatic ducts" sign was found in 16 (62%) of the 26 patients (Fig. 1). Wall enhancement and thickening were identified in 21 (81%) patients (Fig. 2), and filling defects (Fig. 3) and ductal stricture in 6 (24%) and 3 (12%), respectively.
Extrahepatic bile duct abnormalities were seen in 7 (27%) of the 26 patients. The most common finding was wall enhancement of the common bile duct, which was present in 5 (24%) patients with cholangiocarcinoma (Fig. 4). Extrahepatic ductal dilation was found in 5 (19%) of 26 patients. Marked dilation was seen in one patient who had a carcinoma in the common bile duct.
Nine (35%) patients revealed a hepatobiliary malignancy. In these patients, 7 (27%) had a cholangiocarcinoma; 3 in the hilar portion, 2 in the common bile duct and 2 in the intrahepatic ducts. One patient had combined tumors (distal common bile duct carcinoma and hepatocellular carcinoma). Of the 3 patients with a hepatocellular carcinoma, two had liver cirrhosis caused by the hepatitis B virus or alcoholic liver cirrhosis.
In 9 patients that had undergone ERCP, intrahepatic bile duct abnormalities (ductal dilatation, n=9; "too many intrahepatic ducts" sign, n=9; ductal stricture, n=7; and filling defect, n=2) were found. MR imaging showed evidence of intrahepatic abnormalities in all patients. Ductal dilation was shown in all patients. "Too many intrahepatic ducts" sign was seen in 7 of the 9 patients. However, ductal stricture was observed on the MR imaging in 5 of the 9 patients, which was less than that found on ERCP. A filling defect was observed on MR imaging in 4 of the 9 patients, which was more than that found on ERCP. There was no dilation or stricture of the extrahepatic bile ducts in either the ERCP or MRC.
The characteristic findings of clonorchiasis were diffuse, mild dilation of the small intrahepatic bile ducts, particularly in the periphery of the liver. However, the extrahepatic bile ducts were not dilated or only slightly dilated (6, 7). These findings are not encountered in tumors of the bile duct, in periampullary cancer or in choledocholithiasis. In our study, the most common pattern of the biliary ductal dilation was mild dilation of the intrahepatic bile ducts, which occurred in 81% of our patients.
Dilation of the smaller bile ducts is most likely due to obstruction caused by the worms. The 8-15-mm worms or worm aggregates could easily occlude the small peripheral ducts, but larger ducts, such as extrahepatic ducts, are wide enough to be patent even if worms are lodged within them (1). However, the mechanism of obstruction cannot be explained on the basis of fluke size alone as the flukes are flat and 1.5-5 mm thick. Adenomatous hyperplasia, mucus in the bile ducts caused by cholangitis, periductal fibrosis and stricture may have an additional role in the occlusion of ducts and the resultant dilation of the proximal intrahepatic ducts (3, 6, 20-22).
Lim et al. (10) reported that "too many intrahepatic ducts" sign in 22 (76%) of their 29 patients with clononorchiasis on direct cholangiography. In our study, MR cholangiography found "too many intrahepatic ducts" sign in 16 (62%) of the 26 patients. A slightly lower percentage of our study showed "too many intrahepatic ducts" sign than the previous study. We think this was caused by the different selection criteria. The inclusion data of the previous study did not included mild infestation of clonorchiasis, as many of the patients with clonorchiasis had not undergone direct cholangiography for a mild infestation. Our study included a mild infestation of clonorchiasis.
Ultrasonography showed an increased echogenicity of the ductal wall, reflecting cholangitis and periductal fibrosis (17). Choi et al. (8) reported that CT failed to show thickening of the bile duct wall, which might be evidence of periductal fibrosis caused by the worms. On the contrary, Kim et al. (9) showed periductal contrast enhancement in 45% of clonorchiasis patients, thereby suggesting periductal fibrosis. Periductal enhancement was frequently observed in 21 (81%) of our cases. This was due to the increased spatial resolution of the soft tissue on MR compared to CT.
The filamentous wavy and/or elliptical filling defects within the bile ducts, representing adult flukes, are pathognomonic findings on direct cholangiography, but the defects can be obscured by the contrast medium (7, 20). The filling defects of the worm are usually small and irregular, with a uniform size on direct cholangiography (6, 10, 20). The criterion for the diagnosis of stones is known to be the presence of a round, oval or multiangular signal void in the lumen of the bile duct on MRC (11, 14). In our study, the filling defects within the dilated intrahepatic bile ducts were shown in 6 (24%) of the 26 patients. The filling defects were elliptical, irregular shaped, hypointense lesions on the T2-weighted image and MRC. Although not all the patients underwent direct cholangiography or imaging-pathologic correlation, the filling defects of MR image may be regarded as fluke aggregates.
C. sinensis has a high prevalence of coexistent with a hepatobiliary malignancy (3, 5, 23). Chung et al. (23) found that C. sinensis infection was associated with a cholangiocarcinoma about five times more often than with a hepatocellular carcinoma. Experimental study has shown that prolonged C. sinensis infection produces adenomatous hyperplasia and bile duct carcinomas (24). Our study showed that 9 (35%) of the 26 patients had hepatobiliary malignancy. In these patients, 7 had cholangiocarcinoma. There were no patients with other causes predisposing to a cholangiocarcinoma, such as ulcerative colitis, gallstones or recurrent pyogenic cholangitis. Two patients with hepatocellular carcinomas had liver cirrhosis caused by hepatitis B infection, a well-known cause of hepatocellular carcinomas.
The differential diagnosis of clonorchiasis includes primary sclerosing cholangitis, recurrent pyogenic cholangitis and cholangiocarcinoma. Primary sclerosing cholangitis has stenosis, beading and pruning of the dilated intrahepatic bile duct; however, the ducts are much more irregular and serpiginous, which are unlikely in clonorchiasis (19). Recurrent pyogenic cholangitis is characterized by decreased branching and abrupt tapering ("arrowhead" appearance) of the peripheral hepatic ducts as a result of stenosis of the peripheral ducts (25). Dilatation of the extrahepatic bile duct and a stone on recurrent pyogenic cholangitis are more common than clonorchiasis. The pattern of intrahepatic bile duct dilation in clonorchiasis is diffuse, mild dilation of the intrahepatic bile duct without abrupt tapering of the peripheral hepatic ducts. With a cholangiocarcinoma, the obstruction lesion is usually detected, and the entire tree proximal to the mass is proportionally dilated, not just the peripheral hepatic bile ducts, as in clonorchiasis (7).
There were two limitations to this study; firstly, the MR sequences were variable due to the study being retrospective. A prospective study will be necessary to evaluate the roles of the various MR sequences. Secondly, not all patients underwent direct cholangiography, which is regarded as the gold standard for depicting bile duct abnormalities, including ductal dilatation, stricture and filling defects. However, direct cholangiography is an invasive technique and does not depict intrahepatic bile duct dilatation on the proximal level of obstruction. Several reports have shown MRC to be a useful imaging technique that demonstrates the ductal changes in the biliary system (11-13, 16, 26).
In conclusion, MR imaging demonstrates various findings of clonorchiasis, including mild diffuse dilatation, wall thickening and enhancement, and filling defects in the intrahepatic bile ducts and an associated hepatobiliary malignancy. The most common finding of clonorchiasis on MR imaging is diffuse, mild dilatation of the small intrahepatic bile ducts without dilatation of the extrahepatic bile duct.
Figures and Tables
 | Fig. 1Clonorchiasis in a 49-year-old man. Coronal single-shot fast spin echo MR cholangiogram (TR/effective TE=∞/800, 40-mm section thickness) shows too many intrahepatic bile ducts, without dilatation of extrahepatic bile duct. Focal stricture (arrow) is seen in the left intrahepatic bile duct. |
 | Fig. 2Clonorchiasis in a 58-year-old man. Gadolinium-enhanced echo fast gradient echo 3D (TR/TE, 7/2) transverse (A) and coronal (B) images show periductal enhancement of mildly dilated intrahepatic bile duct (arrows). There is no dilatation of extrahepatic bile duct. |
 | Fig. 3Clonorchiasis in a 58-year-old man.
A. Transverse T2-weighted single shot fast spin-echo image (TR/effective TE=∞/92) shows elliptical filling defects (arrows) in a dilated intrahepatic bile duct.
B. Oblique coronal single-shot fast spin-echo MR cholangiogram (TR/effective TE=∞/800, 40-mm section thickness) shows multiple small, ovoid or elliptical shaped, filling defects (arrows) in both the intrahepatic bile ducts. MR cholangiogram more clearly demonstrates the diffuse, mild dilatation of the small intrahepatic bile ducts than in theT2-weighted image (A).
|
 | Fig. 4Clonorchiasis, with a common bile duct carcinoma, in a 75-year-old man.
A. Coronal single-shot fast spin-echo MR cholangiogram (TR/effective TE=∞/800, 40-mm section thickness) shows abrupt obstruction of the proximal common bile duct (arrow) with marked dilatation of the intrahepatic bile duct.
B. Gadolinium-enhanced echo fast gradient echo 3D (TR/TE, 7/2) image at the level of obstruction shows thickened, an enhanced wall of the proximal common bile duct (arrows), suggestive of a cholangiocarcinoma.
|
References
1. Yamaguchi T. Clinical parasitology. 1981. London: Wolfe Medical;50–57.
2. Rim HJ. The current pathobiology and chemotherapy of clonorchiasis. Korean J Parasitol. 1986. 24:7–20.
3. Hou PC. The relationship between primary carcinoma of the liver and infestation with Clonorchiasis sinensis. J Pathol Bacteriol. 1956. 72:239–246.
4. Flavell DJ. Liver-fluke infection as an aetiological factor in bile duct carcinoma of man. Trans R Soc Trop Med Hyg. 1981. 75:814–824.
5. Belmaric J. Intrahepatic bile duct carcinoma and clonorchiasis infection in Hong Kong. Cancer. 1973. 31:468–473.
6. Choi TK, Wong KP, Woong J. Cholangiographic appearance in clonorchiasis. Br J Radiol. 1984. 57:681–684.
7. Lim JH. Radiologic findings of clonorchiasis. AJR Am J Roentgenol. 1990. 155:1001–1008.
8. Choi BI, Kim HJ, Do YS, Han MH, Lee SH. CT findings of clonorchiasis. AJR Am J Roentgenol. 1989. 152:281–284.
9. Kim MS, Yoo HS, Lee JT, Jung SH. Radiologic imaging of bile duct change by clonorchiasis. J Korean Radiol Soc. 1988. 24:878–882.
10. Lim JH, Ko YT, Lee DH, Lee KS, Suh SJ, Woo SK. Clonorchiasis and its complications: cholangiogram revisited. J Korean Radiol Soc. 1992. 28:229–235.
11. Becker CD, Grossholz M, Becker M, Mentha G, de Peyer R, Terruer F. Choledocholithiasis and bile duct stenosis: diagnostic accuracy of MR cholangiopancreatography. Radiology. 1997. 205:523–530.
12. Barish MA, Soto JA. MR cholangiopancreatography: technique and clinical applications. AJR Am J Roentgenol. 1997. 169:1295–1303.
13. Kim MJ, Mitchell MJ, Ito K, Outwater EK. Biliary dilatation: differentiation of benign from malignant causes-value of adding conventional MR imaging to MR cholangiopancreatography. Radiology. 2000. 214:173–181.
14. Guibaud L, Bret PM, Reinold C, Atri M, Barkun ANG. Diagnosis of choledocholithiasis: value of MR cholangiography. AJR Am J Roentgenol. 1994. 163:847–850.
15. Choi BI, Kim TK, Han JK. MRI of Clonorchiasis and cholangiocarcinoma. JMRI. 1998. 8:359–366.
16. Park MS, Yu JS, Kim KW, et al. Recurrent pyogenic cholangitis: comparison between MR cholangiography and direct cholangiography. Radiology. 2001. 220:677–682.
17. Lim JH, Ko YT, Lee DH, Kim SY. Clonorchiasis: sonographic findings in 59 proved cases. AJR Am J Roentgenol. 1989. 152:761–764.
18. Teefey SA, Baron RL, Rohrmann CA, Shuman WP, Freeny PC. Sclerosing cholangitis: CT findings. Radiology. 1988. 169:635–639.
19. Ito K, Mitchell DB, Outwater EK, Blasbalg R. Primary sclerosing cholangitis: MR imaging features. AJR Am J Roentgenol. 1999. 172:1527–1533.
20. Okuda K, Emura T, Morokuma K, Kojima S, Yokagawa M. Clonorchiasis studies by percutaneous cholangiography and a therapeutic trial of toluene-2, 4-diiso-thiocyante. Gastroenterology. 1973. 65:457–461.
21. Hou PC. The pathology of Clonorchiasis sinensis infestation of the liver. J Pathol Bacteriol. 1955. 70:53–64.
22. Lee SH, Shim TS, Lee SM, Chi JG. Studies on pathological changes of the liver in albino rats infected with Clonorchiasis sinensis. Korean J Parasitol. 1978. 16:148–155.
23. Chung CS, Lee SK. An epidemiological study of primary liver carcinoma in Busan area with special reference to clonorchiasis. Korean J Pathol. 1976. 10:33–46.
24. Hou PC. Hepatic clonorchiasis and carcinoma of the bile duct in a dog. J Pathol Bacteriol. 1965. 89:365–367.
25. Kim MJ, Cha SW, Mitchell DG, Chung JJ, Park S, Chung JB. MR imaging findings in recurrent pyogenic cholangitis. AJR Am J Roentgenol. 1999. 173:1545–1549.
26. Fulcher AS, Yurner MA, Franklin KJ, et al. Primary sclerosing cholangitis: evaluation with MR cholangiography-a case-control study. Radiology. 2000. 215:71–80.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download