Abstract
Objective
We wished to evaluate the incidence of non-contiguous spinal injury in the cervicothoracic junction (CTJ) or the upper thoracic spines on cervical spinal MR images in the patients with cervical spinal injuries.
Materials and Methods
Seventy-five cervical spine MR imagings for acute cervical spinal injury were retrospectively reviewed (58 men and 17 women, mean age: 35.3, range: 18-81 years). They were divided into three groups based on the mechanism of injury; axial compression, hyperflexion or hyperextension injury, according to the findings on the MR and CT images. On cervical spine MR images, we evaluated the presence of non-contiguous spinal injury in the CTJ or upper thoracic spine with regard to the presence of marrow contusion or fracture, ligament injury, traumatic disc herniation and spinal cord injury.
Results
Twenty-one cases (28%) showed CTJ or upper thoracic spinal injuries (C7-T5) on cervical spinal MR images that were separated from the cervical spinal injuries. Seven of 21 cases revealed overt fractures in the CTJs or upper thoracic spines. Ligament injury in these regions was found in three cases. Traumatic disc herniation and spinal cord injury in these regions were shown in one and two cases, respectively. The incidence of the non-contiguous spinal injuries in CTJ or upper thoracic spines was higher in the axial compression injury group (35.3%) than in the hyperflexion injury group (26.9%) or the hyperextension (25%) injury group. However, there was no statistical significance (p > 0.05).
Cervical spinal trauma is commonly accompanied with other non-contiguous spinal injuries. The lower cervical and upper thoracic regions are especially notorious for this (1-4), and for this reason, it has been emphasized that the whole cervical spine including the cervicothoracic junction (CTJ) must be examined radiologically in any neck injury (4-5). Non-contiguous fractures of the entire spinal column have been recognized in 4.0-24.0% of cases in the previous reports following violent trauma (1, 6-13). In addition, Shear et al. (14) have reported non-contiguous fractures and subluxations of the cervical spine as a distinct group of injuries having a 9% incidence. However, these studies were based only on the plain radiographs. MR imaging has had an increasing role for the detection of the non-contiguous spinal injuries (15, 16) as well as for the assessment of the spinal injury itself (17-20). In addition, because CTJ and some thoracic spines are usually included in the field of view of the sagittal scan on the cervical spinal MR, information about these areas could well be documented on the cervical spine MR. From this point of view, this study was undertaken to evaluate the incidence of non-contiguous spinal injury in the CTJ or the upper thoracic spines on cervical spinal MR images for the patients having cervical spinal injury.
Eighty-five patients who had cervical spinal MR performed for acute cervical spinal trauma during the proceeding three years were included in our study. For 10 of 85 patients, their cervical spinal MR images had been reported as normal. We retrospectively reviewed the rest of the 75 cervical spinal MR images. There were 58 men and 17 women with a mean age of 35.3 years (range: 18-81 years). Most of the injuries were the result of motor vehicle accidents (n=57), this was followed by falls from a height (n=15), and assaults (n=3). The MR images was obtained by using 1.5 T Siemens Magnetom Vision system (Siemens AG, Erlangen, Germany) or GE Signa system (GE Medical Systems, Milwaukee, Wis). The MR images were obtained 24-48 hours after the patients' admission to the hospital. The timing of the MR images to the date of injury was 1-7 days after the trauma (mean period: 1.23 day). The standard protocol consisted of the sagittal T1-weighted (TR/TE = 550-650/12 ms) and T2-weighted (TR/TE = 3500-3600/112-120 ms, echo train lengths of 8) fast spin echo sequences, a trans-axial T1 weighted spin echo sequence (TR/TE = 700-750/12 ms), and a transaxial T2 weighted fast spin echo sequence (TR/TE = 3500-3600/112-120 ms, echo train lengths of 8) or a trans-axial gradient echo technique (2D fast low angle shot, TR/TE = 620/22 ms, flip angle = 25°) instead of the T2 weighted image. The section thicknesses were 4 mm with a interslice spacing of 1 mm, and the matrix size was 512×200-250. The lowest thoracic vertebra individually included on the sagittal scan was from T4 to T7 (the mean level of the included thoracic vertebrae: 4.5), with a field of view (FOV) of 28 cm.
We classified the cervical spinal injuries based on the mechanism of injury; the axial compression injury group (n=17), the hyperflexion injury group (n=26), and the hyperextension (n=32) injury group, after classifying the cervical spinal injuries according to the Allen and Ferguson classification (21). The axial compression injury group consisted of three Jefferson fractures, one Jefferson fracture combined with dens fracture, and 13 vertical compression injuries of the lower cervical spines. The hyperflexion injury group consisted four flexion dens fractures and 12 distractive flexion injuries, nine compressive flexion injuries, and one compressive and distractive flexion injury of the lower cervical spines. The hyperextension injury group consisted of eight hangman's fractures, two extension teardrop fractures of the axis, 13 compressive extension injuries, eight distractive extension injuries, and one compressive and distractive extension injury of the lower cervical spines.
We evaluated the non-contiguous injury in the CTJ or upper thoracic spine on 75 cervical spinal MR imagings, Non-contiguous injuries are those separated by at least one normal intervening vertebra apart from the cervical spinal injury site (3). The non-contiguous injury was evaluated with regard to the presence of marrow contusion, overt fracture, ligament injury, traumatic disc herniation and spinal cord injury. We also reviewed the CT findings for the evaluation of the fracture details in the cervical spinal injuries and non-contiguous injuries. Overt fracture was defined as when cortical breakage was noted on the CT or MR. Anterior or posterior longitudinal ligament injury was defined as when discontinuity was noted in the normally low signal intensity ligament. Interspinous ligament injury was defined as high T2 signal intensity within the ligaments because of edema (22-23). Disc herniation was defined as tissue signal intensity that was consistent with the nucleus pulposus protruding posteriorly to a vertical line drawn along the posterior cortical border of the inferior vertebral body (24). Spinal cord injury was defined by focal or diffuse signal changes within the spinal cord.
The incidence of the non-contiguous CTJ injury or upper thoracic spinal injury was compared among the axial compression injury group, the hyperflexion injury group and the hyperextension injury group. Fisher's exact test was used for statistical analysis.
Twenty-one of 75 cases (28%) showed non-contiguous marrow contusions (n=14, 18.7%) or overt fractures (n=7, 9.3%) in the CTJ or upper thoracic spines (C7 to T5), those were separated from the cervical spinal injury site on cervical spinal MR. The mean number of intervening vertebrae was 4.2 (range: 1-8). The types of fractures in the CTJ or upper thoracic spines were four burst fractures and three wedge compression fractures. Although these non-contiguous fractures in the CTJ or upper thoracic spines did not show any posterior element fracture, in three of them, there were non-contiguous ligament injuries found at the injured levels (anterior longitudinal ligament injury in two and posterior longitudinal ligament injury in one). Traumatic disc herniation and spinal cord injury were found in one and two cases of them, respectively.
As for the mechanism of cervical spinal injury, the incidence of the non-contiguous spinal injury in the CTJ or upper thoracic spines was higher in the axial compression injury group (35.3%) than in the hyperflexion (26.9%) or hyperextension (25%) injury groups. However, this result was not statistically significant (p > 0.05). The incidence of the non-contiguous spinal fracture was also higher in the axial compression injury group (17.6%) than in the hyperflexion (7.7%) injury group or the hyperextension (6.3%) injury group. However, there was no statistical significance for this either (p > 0.05). The incidences of non-contiguous ligament injury and spinal cord injury were also higher in axial compression injury group (11. 8% and 5.9%, respectively) than in the hyperflextion injury group (3.8% and 3.8%, respectively) or hyperextension injury group (3.1% and 0%, respectively). However a case of non-contiguous traumatic disc herniation was noted in the hyperflexion injury group.
For the 17 axial compression injuries, six (35.3%) had non-contiguous CTJ or upper thoracic spinal injuries, and marrow contusions and overt fractures were found in three of them (17.6%). These injuries were shown in two of the Jefferson fractures (Fig. 1) and in four of the vertical compression injuries of the lower cervical spines. Overt fractures in the CTJ or upper thoracic spines were associated with one Jefferson fracture and two vertical compression injuries of the lower cervical spines. In the last two cases, non-contiguous ligament injuries (11.8%) were also found at the non-contiguously injured sites (Fig. 2). Non-contiguous spinal cord injury (5.9%) was also found in one of those cases. In the 26 hyperflexion injuries, seven of them (26.9%) had non-contiguous CTJ injury or upper thoracic spinal injuries; there were marrow contusions in five (19.2%) and overt fractures in two (7.7%). The non-contigous injuries were shown in one of the type III dens fractures, three of the compressive flexion injuries, and three of the distractive flexion injuries of the cervical spines. Overt fractures in the CTJ or upper thoracic spines were associated with one type III dens fracture and with one of the distractive flexion injuries of the lower cervical spine. In the case of the type III dens fracture, disc herniation with posterior longitudinal ligament tearing and focal spinal cord injury were also found in the CTJ as well as a non-contiguous wedge compression fracture (Fig. 3). Therefore, the incidence of the non-contiguous disc herniation, ligament or spinal cord injury in the hyperflexion injuries was 3.8%, respectivery. In the 32 hyperextension injuries, eight of them (25%) had non-contiguous CTJ or upper thoracic spinal injuries; six (18.8%) had marrow contusions and two (6.3%) had overt fractures. The above injuries were shown in one of the hangman's fractures, in four of the distractive extension injuries, in two of compressive extension injuries, and in one of the compressive and distractive extension injuries of the lower cervical spines. Overt fractures in the CTJ or upper thoracic spine were associated with two distractive extension injuries of the lower cervical spines. In one case of distractive extension injury of lower cervical spine, non-contiguous ligament injury (3.1%) was found in the CTJ (Fig. 4).
We also evaluated the incidence of the non-contiguous spinal injury in the CTJ or upper thoracic spines, and we divided the cases into the upper (C1-2) and lower (C3-7) cervical spine injuries. In the 18 upper cervical spine fractures, four (22%) had non-contiguous spinal lesions in the CTJ or upper thoracic spines. In 57 lower cervical spine fractures, 17 of them (29.8%) had non-contiguous spinal lesions in the CTJ or upper thoracic area. There is no statistical significant difference in the incidence of the multilevel injury combined with cervical spinal and CTJ or upper thoracic spinal injury between the high (22%) and lower (29.8%) cervical spinal fracture patients (p > 0.05).
Non-contiguous spinal injury is defined as a lesion separated by at least one normal intervening vertebra from the cervical spine fracture or subluxation/dislocation (4). Hadden and Gillespie (13) reported an incidence of 24% and Henderson et al. (12) have reported that 15.2% of multilevel spinal fractures of the entire column contained non-contiguous injuries. These studies were based on the radiographic findings only. Qaiyum et al. (16) have reported high incidence of non-contiguous spinal injuries (18 in a group of 110 spinal injury patients) as well as a high incidence (41%) of bone bruising, which was an unsuspected invisible injury, by using MR.
Gupta and el Masri (1) have found that multilevel injuries observed on radiographs most commonly involved the lower cervical and cervicothoracic levels, and this finding was also reported on by Qaiyum et al. (16). In our study, we found that 28% of the patients with cervical spinal injuries were accompanied with non-contiguous CTJ or upper thoracic spinal injuries on the cervical spinal MR. It is a higher incidence than had previously been observed by Shear et al. (14) and Ryan et al. (4) (their studies were based on the plain radiographs), and even higher than the results that were observed by Qaiyum et al. (16) that were based on MR (21.2%). These results makes us suspect that various forms of stress could be inflicted on the CTJ or upper thoracic area in the cases of cervical spinal fracture more often than has been previously reported. We surmised that these results were caused by two reasons. First, MR imaging provides a higher sensitivity concerning the marrow contusion, which could not be depicted on plain radiographs or CT. Second, we used a MR protocol with a large FOV (28 cm). The FOV of cervical spinal MR imaging is usually 24 cm (25) or 28 cm (26). A large FOV made it possible that the upper thoracic spines were included in the field of view on the sagittal MR images. Thoracic vertebrae were individually included on sagittal MR image from T4 to T7 in this study (mean level: 4.5). When the FOV is enlarged, the pixels size will also be increased, which can lead to poorer spatial resolution. However, on the contrary, a large FOV can improve the signal/noise ratio.
There have been several reports about the mechanisms of non-contiguous spinal lesion associated with cervical spinal fracture (3, 27). However, this non-contiguous spinal injury could be expected to have various features and locations depending on the mechanism of injury, the alignment of cervical spine, the strength and state of the supporting ligaments and muscles, and the orientation of the facets at the instant of the injury (14). In our results, non-contiguous spinal injuries in the CTJ or the upper thoracic spine are particularly associated with axial compression injury of the cervical spine more commonly than with hyperflexion or hyperextension injuries of the cervical spine, although this was not statically significant. In addition, the non-contiguous fracture types in the CTJ or the upper thoracic spines were also axial compression injuries (burst fractures in four cases and wedge compression fractures in three cases) rather than other types of fractures.
The importance of identifying all the injuries lies in the unique problems that each of these cases present for their management (14). Two stable non-contiguous fractures in the cervical spine can be considered as one. One stable and one unstable injury can be considered as a single unstable injury. However, two unstable non-contiguous injuries in the cervical spine create a potentially mobile intermediate segment that requires the physician's special consideration. Calenoff et al. (10) have also stressed the clinical significance of early recognition of non-contiguous spinal lesions to prevent any extension of neurologic deficit, the pain pattern, spinal instability and/or deformity. From these points of view, awareness of the possibility of non-contiguous spinal injuries in the CTJ and upper thoracic spines in the patients with cervical spine trauma is important for the management of these lesions. However, fractures of the posterior element of the spine, which could suggest potential osseous instability, may be difficult to accurately evaluate on MR only. Therefore, if unstable non-contiguous spinal injuries are suspected, then further evaluation with CT may be needed for the assessment of the occult fracture and the posterior element injury.
This study has limitations from several aspects. First, the clinical correlation and significance corresponding to the CTJ or upper thoracic spinal injury could not be established in most of the cases. Second, the short time inversion recovery (STIR) sequence, which is the most sensitive sequence for the detection of verterbral body bone bruises, was not undertaken in our study. Sagittal STIR images of the whole spine have been recommended for acute cervical spinal traumas by several previous reports (15-16). We also advocate that when MR is indicated for acute cervical spinal injury, it should include he CTJ, the upper thoracic spine, and even the full vertebral column, and particularly, the STIR sequences could be very helpful. Third, as stated above, posterior element fractures in the cervical spine may be difficult to accurately evaluate just using MR. Therefore all acute spinal injuries may not be identified and visualized properly with MR alone.
Although a future study concerning the mechanism of injury and clinical correlation with a larger population will be needed, we can conclude that the occurrence of the cervical spinal injury combined with non-contiguous CTJ or upper thoracic spinal injury could be quite common on cervical spine MR. In addition, awareness of the possibility of the non-contiguous spinal injury might be important, and particularly in the cases of axial compression injury of the cervical spine.
Figures and Tables
 | Fig. 1T2-weighted sagittal MR image reveals band-like bone marrow contusions (arrowheads) in the upper thoracic spines (T2-4) as well as a prevertebral hematoma (arrows) that resulted from a Jefferson fracture (not shown) in the upper cervical level. |
 | Fig. 2
A. T1-weighted sagittal MR image shows vertical compression injuries of C5 and C6 (large arrows, CT is not shown) and a burst fracture of T3 (open arrow). Note the discontinuity of the anterior longitudinal ligament (small arrow).
B. T2-weighted MR image shows a large prevertebral hematoma (arrowheads) that was caused by injuries in C5-6 and a non-contiguous fracture in T3 (open arrow).
|
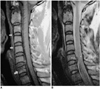 | Fig. 3T1- (A) and T2- (B) weighted sagittal MR images in a patient with type III dens fracture (not shown).
A. T1-weighted MR image shows compression fracture of C7 (large arrow) and linear prevertebral hemorrhage (small arrows) that resulted from C2 fracture.
B. Note the traumatic disc herniation (open arrow) and a focal compressive myelopathy (arrowhead) at the disc level of C7-T1.
|
 | Fig. 4Non-contiguous ligament injury in a hyperextension cervical spinal injury. T2-weighted MR image reveals a traumatic disc herniation (arrowhead) and anterior longitudinal tear (solid arrow) and interspinous (black arrows) ligament tear in C5-6 due to the distractive extension injury. Note the non-contiguous ligament injury in the anterior longitudinal ligament at the disc level of C7-T1 (open arrow). |
References
1. Gupta A, el Masri WS. Multilevel spinal injuries. Incidence, distribution and neurologic patterns. J Bone Joint Surg Br. 1989. 71:692–695.
2. Huelke DF, Nusholtz GS. Cervical spine biomechanics: a review of the literature. J Orthop Res. 1986. 4:232–245.
3. Lee C, Rogers LF, Woodring JH, Goldstein SJ, Kims KS. Fractures of the craniovertebral junction associated with other fractures of the spine: overlooked entity? AJNR Am J Neuroradiol. 1984. 5:775–781.
4. Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992. 23:38–40.
5. Nichols CG, Young DH, Schiller WR. Evaluation of cervicothoracic junction injury. Ann Emerg Med. 1987. 16:640–642.
6. Beldekos A, Korres DS, Nikolakakos G. A Chance's fracture in a double level fracture of the spine. Injury. 1981. 13:34–36.
7. Blahd WH Jr, Iserson KV, Bjelland JC. Efficacy of the post-traumatic crosstable lateral view of the cervical spine. J Emerg Med. 1985. 2:243–249.
8. Harrington T, Barker B. Multiple trauma associated with vertebral injury. Surg Neurol. 1986. 26:149–154.
9. Korres DS, Katsaros A, Pantazopoulos T, Hartofilakidis-Garofalidis G. Double or multiple level fractures of the spine. Injury. 1981. 13:147–152.
10. Calenoff L, Chessare JW, Rogers LF, Toerge J, Rosen JS. Multiple level spinal injuries: importance of early recognition. AJR Am J Roentgenol. 1978. 130:665–669.
11. Vaccaro AR, An HS, Lin S, Sun S, Balderston RA, Cotler JM. Noncontiguous injuries of the spine. J Spinal Disord. 1992. 5:320–329.
12. Henderson RL, Reid DC, Saboe LA. Multiple noncontiguous spine fractures. Spine. 1991. 16:128–131.
13. Hadden WA, Gillespie WJ. Multiple level injures of the cervical spine. Injury. 1985. 16:628–633.
14. Shear P, Hugenholtz H, Richard MT, et al. Multiple noncontiguous fractures of the cervical spine. J Trauma. 1988. 28:655–659.
15. Saifuddin A. MR of acute spinal trauma. Skeletal Radiol. 2001. 30:237–246.
16. Qaiyum M, Tyrrell PN, McCall IW, Cassar-Pullicino VN. MR detection of unsuspected vertebral injury in acute spinal trauma: incidence and significance. Skeletal Radiol. 2001. 30:299–304.
17. Kliewer MA, Gray L, Paver J, et al. Acute spinal ligament disruption: MR imaging with anatomic correlation. J Magn Reson Imaging. 1993. 3:855–861.
18. Terk MR, Hume-Neal M, Fraipont M, Ahmadi J, Colletti PM. Injury of the posterior ligament complex in patients with acute spinal trauma: evaluation by MR imaging. AJR Am J Roentgenol. 1997. 168:1481–1486.
19. Shimada K, Tokioka T. Sequential MR studies of cervical cord injury: correlation with neurological damage and clinical outcome. Spinal Cord. 1999. 37:410–415.
20. Goldberg AL, Rothfus WE, Deeb ZL, et al. The impact of magnetic resonance of the diagnostic evaluation of acute cervicothoracic spinal trauma. Skeletal Radiol. 1988. 17:89–95.
21. Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982. 7:1–27.
22. Hoffman JR, Schriger DL, Mower W, Luo JS, Zucker M. Low-risk criteria for cervical-spine radiography in blunt trauma: a prospective study. Ann Emerg Med. 1992. 21:1454–1460.
23. Cornelius RS. Imaging of acute cervical spine trauma. Semin Ultrasound CT MR. 2001. 22:108–124.
24. Vaccaro AR, Falatyn SP, Flanders AE, Balderson RA, Northrup BE, Cotler JM. Magnetic resonance evaluation of the intervertebral disc, spinal ligament, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine. 1999. 24:1210–1217.
25. Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine. 2001. 26:1866–1872.
26. Yousry I, Forderreuther S, Moriggl B, et al. Cervical MR imaging in postural headache: MR signs and pathophysiological implications. AJNR Am J Neuroradiol. 2001. 22:1239–1250.
27. Nusholtz GS, Huclke DF, Lux P, Alem NM, Montalvo F. Cervical spine injury mechanisms. 1983. 27 th Sta. In : Car Crash Conference Proceedings; Warredale, PA: Society of Automotive Engineers;179–198.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download