Abstract
Materials and Methods
A stent-like electrode was knitted from a single thread of nitinol wire and interconnected to a generator using similar wire. In order to gauge the extent of radiofrequency ablation (RFA), we measured the depth of the ablated area in cow liver using a combination of 180-sec time intervals and 20-watt power increments. For data processing, Cox regression analysis was used. RFA was also applied to the small intestine of rabbits using this stent-like electrode under six different sets of conditions: 10 watts for 1 min, 10 watts for 2 mins, 20 watts for 1 min, 20 watts for 2 mins, 30 watts for 1 min, and 30 watts for 2 mins. To determine the gross and microscopic findings, six animals were sacrificed immediately after the procedure and the results obtained under the different sets of conditions were correlated. Eight rabbits were monitored for 4 weeks prior to sacrifice.
Results
For both ex-vivo and in-vivo ablations, the depth of the thermal lesion showed linear correlation with both the duration of RFA and the power applied. RFA of the duodenum was technically successful in all 14 rabbits. The acute changes occurring in the rabbits' small intestine included color change, cytoplasmic denaturation, fibrin deposition and hemorrhage, among which hemorrhage of the mucosal layer was the earliest finding. RF ablation for 2 mins at 30 watts caused serosal hemorrhage. The gross and histologic changes occurring showed close correlation under all six sets of conditions.
During recent years, minimally invasive treatment modalities have been an area of considerable interest, and one of the technologies involved is radiofrequency ablation (RFA). Over the past decade, encouraging clinical results have been reported regarding the use of radiofrequency energy for the treatment of benign lesions such as osteoid osteomas and benign prostatic hyperplasia, as well as primary and secondary malignant tumors of the brain, head and neck, liver, and prostate gland (1-12).
To our knowledge, the gastrointestinal tract has not yet been a target for interstitial thermotherapy, despite the fact that gastrointestinal tract carcinoma is a leading cause of cancer-related deaths and there are few local treatment methods that can be used in inoperable patients (13).
In radiofrequency ablation of the gastrointestinal tract, the target organ is not solid but hollow, and a specially designed electrode, suitable for use where time and power parameters are restricted, is required. We devised a stent-like electrode for the radiofrequency ablation of hollow viscera such as the gastrointestinal, biliary, and urinary tract.
The objectives of this study were to evaluate the technical feasibility of this stent-like electrode and to assess the histological change occurring in small bowel in instances in which it is used. Thus, we performed an ex-vivo study involving cow liver and an in-vivo study in which rabbit duodenum was used.
We developed a stent-like electrode that consisted of four parts: an introductory sheath, a stent, a tube through which a guide wire is passed, and an adaptor (Fig. 1). The sheath was made from 8-F teflon tubes, and the tube through which the guide wire is passed was made from 3-F polyethylene tubes, with a tapered dilator attached to the tip of the guide wire tube. The stent itself was knitted from a single thread of 0.22-mm nitinol wire in a tubular configuration and with an interlocking, diamond-shaped pattern. One end of the stent was collapsed and fixed with a polyethylene tube, using nitinol wire. The free end of the this wire, connected to the stent, was used as a connector, and insulated with a 3-F polyethylene tube (Figs. 1, 2).
In order to gauge the extent of RFA, we measured the depth of ablation in cow liver. Using the stent-like electrode and an RF generator (RF2000, Radiotherapeutics Corporation, Calif., U.S.A.), radiofrequency energy was applied to excised cow liver through the parenchymal tract at 3-min-intervals (3, 6, 9, 12, and 15 mins) and in 20-watt increments (10, 30, 50, 70, and 90 watts) (Fig. 3). During the procedure, impedance, power output, and elapsed time were recorded at 15-sec-intervals until full system impedance was realized.
After the completion of RFA, the liver was sectioned serially across the ablation zone, either perpendicular to the electrode or parallel to the needle track, and the maximal transverse diameter of each lesion was measured.
Correlation between the thickness of the thermal lesion and (a) elapsed time to full system impedance, and (b) power applied was determined using Cox regression analysis (SPSS for Windows, version 10.01; Chicago, Ill., U.S.A.).
On the basis of a protocol approved by the animal research committee at Chosun University, 14 male white New Zealand rabbits, weighing between 2.0 and 3.2 kg, were anesthetized via intramuscular injection using a mixture of Rompun (Bayer, Seoul, Korea) and Ketamin (Yuhan, Seoul, Korea), both at a concentration of 1mg per kg of body weight. After the thighs and abdomen of each rabbit were shaved, the animals were placed in the supine position within a fixation device, and two 3×5-cm ground pads (each with conductive gel applied to their surface) were placed bilaterally on each thigh. Under fluoroscopic guidance, the anterior wall of the stomach was sutured to the abdominal wall in a purse-string fashion using Blue Nylon 3.0 (AiLee, Pusan, Korea). Next, the stomach was punctured at the center of the purse string suture using an 18-gauge peripheral catheter (Angiocath, Becton Dickinson, Seoul, Korea) and a guide-wire was advanced through the sheath of the catheter until it reached the duodenum. The stent-like electrode was advanced over the guide-wire as far as the distal duodenum.
Three different levels of RF energy were applied to three different sites of the duodenum in a retrograde sequence, moving from distal to proximal positions (Fig. 4), and during each application, impedance (in ohms) was documented every 15 sec. Energy was applied under six sets of conditions: 10 watts for 1 min, 10 watts for 2 mins, 20 watts for 1 min, 20 watts for 2 mins, 30 watts for 1 min, and 30 watts for 2 mins. Higher levels of RF energy (40, 50, and 60 watts for 1 and 2 mins) were applied to additional rabbits.
Six rabbits were sacrificed immediately after the application of RF energy and the gross and microscopic pathological findings were correlated with the twelve different power and time settings used. Eight rabbits were monitored for 4 weeks following the procedure, during which time they were pathologically examined.
A total of 40 ablations were performed in the excised livers, showing that the dimensions of the thermal lesions increased both with elapsed time and increased RF energy levels. Cox regression analysis demonstrated that the thickness of the resultant lesion showed linear correlation with both elapsed time (Fig. 5) and the power applied (Fig. 6). The regression equation used was as follows: diameter of the thermal lesion= -11.436+1.57 elapsed×time+0.315×watts (p value < .001; r2 , 82%).
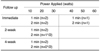
RF ablation using the stent-like electrode was technically successful in all 14 rabbits. During ablation of the duodenum, impedance of between 60 and 120 ohms was maintained. During the 4-week follow-up period, three of eight rabbits in the 2-min group died. In two rabbits, impedance increased rapidly (within 75 to 90 sec) and both animals died within one day of the procedure. One rabbit to which we applied RFA at power levels of 10, 20, and 30 watts for 2 min died 7 days after the procedure. Three animals (two in the 1-min group and one in the 2-min group) were sacrificed at the end of the 2nd week after ablation, and two more (both in the 1-min group) at the end of the 4th week (Table 1). During the RF procedure, three sites were perforated and the duodenum was seen to adhere to adjacent organs such as the liver, abdominal wall, and colon (Fig. 7).
The acute changes apparent in the rabbits' small intestine following RF ablation included color change, cytoplasmic denaturation, fibrin deposition and hemorrhage, among which hemorrhage of the mucosal layer was the earliest finding. Ablation for 2 min at 30 watts caused serosal hemorrhage (Fig. 8).
Sequential histologic findings correlated well with the six different power and elapsed time parameters used in this part of the study (Table 2). Animals subjected to one minute of RF ablation manifested no histologic change either 2 or 4 weeks after the procedure, irrespective of the power applied.
Radiofrequency ablation systems are comprised of three components: a radiofrequency generator, an active electrode, and dispersive electrodes. RF energy (alternating current) is introduced into tissue via the active electrode, and as it moves from there to the dispersive electrode (i.e. the electrosurgical return pad), and back again, ions within the tissue oscillate as they attempt to follow this change in direction. This movement results in frictional heating of the tissue, and as its rises above 60℃, cells begin to die. It is this phenomenon that leads to necrosis in the region surrounding the electrode.
RF thermal ablation using high-frequency electrical current is now an accepted procedure for the control of certain tumors. For both sexes, carcinoma of the gastrointestinal tract was the leading cause of cancer death in the United States in the year 2000, with a 5-year relative survival rate of only 5%. In about 58% of patients with esophageal cancer and 40% of those with gastric cancer, curative resection is not feasible and palliative anastomotic surgery is the usual option. In patients with inoperable cholangiocarcinoma, several authors have reported that intracavitary radiation therapy can be an effective local treatment and has a positive effect on patient survival (13-15). Using currently available RF ablation technology, zones of necrosis of up to 5 cm in diameter can be created in a single application, and tumors of larger diameter can be addressed with multiple applications of RF energy from different deployment sites (16-19).
There are several possible differences between radiofrequency ablation of a gastrointestinal tract lesion and other solid organs such as the liver. First, we found it impossible to apply maximal power for an extended period, so estimation of the ablation depth required was essential prior to RFA. The gastrointestinal tract is adjacent to the common bile duct and other structures, and to avoid possible injury, care thus needs to be taken if the tract undergoes RFA for the maximum possible time and at maximal power. Secondly, if the center of the target lesion contains a fluid- or air-filled space, the dimensions of the resultant thermal lesion may be affected due to heat conduction and convection within that tissue. In our study, two rabbits in the 2-min group experienced a rapid increase in the level of impedance during RF ablation and both died the next day. We surmise that the duodenum of these animals was seriously injured by RF ablation, indicating that bowel circumstances could affect the procedure. Thirdly, it is very hard to monitor ablation while it is on-going, and the plan for RFA must thus be decided in advance, according to the size of the target lesion, after determining this by means of CT, MRI, or ultrasound, for example.
Although the regression equation for depth of a thermal lesion due to elapsed time and applied power derived from the ex-vivo study had a high correlation value, correlation was low when the equation was used in our in-vivo study. Prior to its use in a clinical situation, the equation should be refined to a higher probability through additional ex-vivo studies. Two factors present in our ex-vivo study may affect the extent of a thermal lesion: tissue composition and the lack of perfusion. The first of these is the principal factor that can alter the extent of coagulation following RF ablation. Since heat is conducted through different tissues at various rates, the power settings for RF ablation vary according to the tissue involved. In addition, heat transfer through excised cow liver is undoubtedly different from that through the bowel tissue of a living rabbit. Equally as important to the development of a thermal lesion is the degree of perfusion within tissue. The movement of blood or other fluids through tissue has been reported to reduce heat generation during thermal ablation, a phenomenon labeled the heat-sink effect (20). In this way, ablation near major blood vessels can require either longer periods of time or higher levels of power, or both, if the resultant lesions are to encompass the areas of tissue to the desired degree. Since perfusion-mediated tissue cooling reduces the extent of coagulation necrosis produced by thermal ablation, tissue that is not perfused (such as excised cow liver) will exhibit larger zones of ablation than are normally seen in perfused tissue. As a result, the correlation noted in the ex-vivo study is less clinically useful than in an in-vivo or tumor study; however, it certainly provides the basis for developing a clinical model for use in perfused tissue.
The stent-like electrode developed for this work has some advantages over currently configured needle electrodes used in soft tissue coagulation, providing easy control of the extent of the thermal lesion induced. Its shape, furthermore, permits its use in any tubular structure, including the esophagus, gastric outlet, bile duct, and vessels. More importantly, in this study the stent-like electrode did not directly perforate the gastrointestinal tract, and because it has no sharp end or point, perforation during future applications is unlikely. In addition, when applied to the duodenum, it was easily expanded and retracted within the tissue. Because the bowel changes its shape and location during RFA with this electrode, real-time ultrasonographic guidance could well be useful.
The changes noted in the duodenum following RF ablation in this study correspond closely with these reported in other studies involving soft tissues (1, 10, 17). The resultant thermal lesions were comprised mainly of coagulation necrosis and fibrosis, and any changes in the mucosal layer had healed completely within two weeks. However, long application times and/or high power applications resulted in submucosal and serosal injuries that lead to peritonitis or ulcer formation and eventual bowel perforation. We believe that RFA procedures that combine lower power with shorter elapsed time will, in future, be the preferred manner of using RFA to address gastrointestinal malignancies, including biliary caner.
While the results of this experimental study are encouraging, determination of a more accurate algorithm for applying radiofrequency energy to tissue within the gastrointestinal tract will require further investigation and long-term follow-up in animals. In addition, the effect of bowel circumstances on RF ablation should be investigated before its application in cases involving unresectable gastrointestinal lesions.
Figures and Tables
Fig. 1
Photograph of the stent-like electrode, showing connection between the nitinol wire and adaptor (A); expanded stent-like electrode (B); connecting wire between the stent and generator, with insulation of this wire by a polyethylene tube (C).

Fig. 3
Whole cow liver (A) was used for ex-vivo study. The stent-like electrode was introduced through the parenchymal tract (B); the electrode after ablation (C); sectioned liver shows an ovoid zone of ablation along the parenchymal tract (D).

Fig. 4
Conventional film obtained during RF ablation of the duodenum.
A. First ablation, at distal duodenum.
B. Second ablation, at more proximal duodenum.
C. Third ablation, at proximal duodenum.
Fig. 5
Graph of time vs. depth of ablation, showing linear correlation between these two parameters.
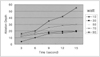
Fig. 6
Graph of power applied vs. depth of ablation, showing linear correlation between these two parameters.
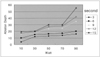
Fig. 7
Gross findings just after RF ablation.
A. Minimal change is noted after 10 W / 1-min ablation (arrow).
B. Dark-colored hematoma is noted after 20 W / 1-min ablation (arrow).
C. Larger hematoma is noted after 30 W / 1-min ablation (arrow).
D. Two-week follow-up after 20 W / 2-min ablation. The duodenum was perforated at three different sites, at which it adhered to adjacent organs such as the liver (large arrow), abdominal wall (arrowhead), and colon (small arrow).

Fig. 8
Histologic findings after ablation using various combinations of power and elapsed time.
A. 30 W / 1-min. Hemorrhagic necrosis occurred in the lumen, but the lamina propria and serosa are intact.
B. 60 W / 2-min. Hemorrhagic necrosis of the mucosa, lamina propria and serosa has occurred.
C. Four-week follow-up, 20 W /1-min. A regenerated mucosal layer is apparent.
D. Two-week follow-up, 20 W / 2-min. Granulation tissue, fibrinoid necrosis, neovascularization and inflammatory cell infiltration indicate ulcer formation. The bowel was perforated.

Acknowledgements
The authors wish to thank Thomas Lawson, PhD, Department of Research and Development, Radiotherapeutics Corporation, for his reading and revising of the manuscript, and Lee Yoon-Ki, Ph D, Department of Automobile Engineering, Chosun College of Science and Technology, for providing the illustration of the stent-like electrode system.
References
1. Goldberg SN, Gazelle GS, Mueller PR. Thermal ablation therapy for focal malignancy: a unified approach to underlying principles, techniques, and diagnostic imaging guidance. AJR Am J Roentgenol. 2000. 174:323–331.
2. Rossi S, Buscarini E, Garbagnati F, et al. Percutaneous treatment of small hepatic tumors by an expandable RF needle electrode. AJR Am J Roentgenol. 1998. 170:1015–1022.
3. Livraghi T, Goldberg SN, Meloni F, Solbiati L, Gazelle GS. Hepatocellular carcinoma: comparison of efficacy between percutaneous ethanol instillation and radiofrequency. Radiology. 1999. 210:655–663.
4. Seki T, Wakabayashi M, Nakagawa T, et al. Ultrasonically guided microwave coagulation therapy for small hepatocellular carcinoma. Cancer. 1994. 74:817–825.
5. Anzai Y, Lufkin R, Desalles A, Hamilton DR, Rarahani K, Black KL. Preliminary experience with MR-guided thermal ablation of brain tumors. AJNR Am J Neuroradiol. 1995. 16:39–48.
6. Zlotta AR, Wildschutz T, Raviv G, et al. Radiofrequency interstitial tumor ablation (RITA) is a possible new modality for treatment of renal cancer : in-vivo and in-vivo experience. J Endourol. 1997. 11:251–258.
7. Lewin JS, Connell CF, Duerk JL, et al. Interactive MRI-guided radiofrequency interstitial thermal ablation of abdominal tumors: clinical trial for evaluation of safety and feasibility. J Magn Reson Imaging. 1998. 8:40–47.
8. Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gephart MC, Mankin JH. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am. 1998. 80-A:815–821.
9. Dupuy DE, Goldberg SN. Image-guided radiofrequency tumor ablation: challenges and opportunities, part II. J Vasc Interv Radiol. 2001. 12(10):1135–1148.
10. Choi DI, Lim HK, Park JM, et al. An experimental study on hepatic ablation using an expandable radio-frequency needle electrode. J Korean Radiol Soc. 1999. 41:1127–1132.
11. Lee JD, Lee JM, Kim SW, Kim CS, Mun WS. MR imaging-histopathologic correlation of radiofrequency thermal ablation lesion in a rabbit liver model: observation during acute and chronic stage. Korean J Radiol. 2002. 2(3):151–158.
12. Lim HK. Radiofrequency thermal ablation of heptocellular carcinomas. Korean J Radiol. 2000. 1(4):175–184.
13. Park HS, Do YS, Suh SW, et al. Upper gastrointestinal tract malignant obstruction: initial results of palliation with a flexible covered stent. Radiology. 1999. 210:865–870.
14. Park GH, Cho SG, Kang SG, et al. Intraluminal brachytherapy after metallic stent placement in primary bile duct carcinoma. Korean J Radiol. 2001. 44:675–682.
15. Kim IH, Lee DH, Yoo JG, et al. The efficacy of intraluminal radiotherapy after metallic stent insertion in malignant biliary tract obstruction. Korean J Gastrointest Endosc. 2000. 20:449–455.
16. Solbiati L, Goldberg SN, Lerace T, Livraghi T, Sironi S, Gazelle GS. Hepatic metastases: percutaneous radiofrequency ablation with cooled-tip electrodes. Radiology. 1997. 205:367–374.
17. Siperstein AE, Gitomirski A. History and technological aspect of radiofrequency thermoablation. Cancer J. 2000. 6:supp.4. s293–s303.
18. Goldberg SN, Gazelle GS, Solbiati L, Rittman WJ, Mueller PR. Radiofrequency tissue ablation : increased lesion diameter with a perfusion electrode. Acad Radiol. 1996. 3:636–644.
19. Yeh MM, Trembly BS, Douple EB, et al. Theoretical and experimental analysis of air cooling for intracavitary microwave hyperthermia application. IEEE Trans Biomed Eng. 1994. 41:874–882.
20. Lu DS, Raman SS, Vodopich DJ, Wang M, Sayre J, Lassman C. Effect of vessel size on creation of hepatic radiofrequency lesions in pigs: assessment of the "heat-sink" effect. AJR Am J Roentgenol. 2002. 178(1):47–51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download