Abstract
Objective
To determine the usefulness of tissue harmonic imaging (THI) and pulse-inversion harmonic imaging (PIHI) in the evaluation of normal and abnormal fetuses.
Materials and Methods
Forty-one pregnant women who bore a total of 31 normal and ten abnormal fetuses underwent conventional ultrasonography (CUS), and then THI and PIHI. US images of six organ systems, namely the brain, spine, heart, abdomen, extremities and face were compared between the three techniques in terms of overall conspicuity and the definition of borders and internal structures.
Among technical advances in US during the past decade, those achieved in the fields of contrast and harmonic imaging are most prominent. Owing to improved spatial and contrast resolution and the occurrence of fewer artifacts than with conventional US (CUS), tissue harmonic imaging (THI), known to be particularly useful in patients in whom imaging is difficult, is utilized for the examination of various organ systems, often in conjunction with US contrast imaging (1). Reports have described the superiority of THI to CUS for examinations of the heart (2-5), brain (6-7), liver (8-12), and kidney (13-17). Pulse-inversion harmonic imaging (PIHI) is a newer technique that generates a pure harmonic signal by setting off fundamental signals, and is known to provide very high spatial resolution (10).
For the evaluation of fetal abnormalities, US is the primary diagnostic modality (18-19). Sometimes, however, diagnosis is difficult due to maternal obesity, uterine myomas, or oligohydramnios (20-22), and in these situations, THI can be helpful. To our knowledge, however, no published report has compared the ability of CUS, THI, and PIHI to evaluate fetal structures.
Although the use of US contrast imaging might also be helpful, this cannot be justified on account of possible fetal damage. THI and PIHI, however, which utilize low-amplitude harmonic signals generated in the body, seem, in theory, to be safe for the fetus, though this has not been formally investigated.
The purpose of this study was to assess the ability of THI and PIHI to delineate fetal structures in various organ systems of normal or abnormal fetuses, and to determine interobserver agreement.
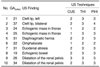
A prospective study conducted at our hospital involved 41 pregnant women who bore a total of 41 fetuses and visited our department for level-II obstetric US. Gestational age ranged from 12 to 37 (mean, 25) weeks: for nine, it was 10-20 weeks; for 23, 21-30 weeks; and for the remaining nine, more than 30 weeks. Among these 41 women, the findings of fetal US were normal in 31 and abnormal in the remaining ten. Abnormalities included facial cleft (2), echogenic thoracic mass (2), diaphragmatic hernia (1), omphalocele (1), duodenal atresia (1), echogenic bowel (1) and dilatation of the renal pelvis (2). The diagnosis was confirmed at delivery or autopsy in five of these ten patients, two were followed-up for five months, and the remaining three were lost to follow-up. In two fetuses with a dilated renal pelvis, postnatal renal US findings were normal.
All images were obtained using a 2-5 MHz convex transducer (HDI 5000; Advanced Technology Laboratories, Bothell, Wash., U.S.A.), and CUS, THI, and PIHI techniques. CUS was used first, followed, successively, by THI and PIHI, and for each technique, standard institutional US protocols were applied and between 20 and 30 images were obtained; in each instance, the same depth, magnification and focus were used, and gray-scale gain was adjusted to optimize image quality.
All CUS, THI, and PIHI images obtained were evaluated by two radiologists using a 2×2K picture archiving and communication system monitor (General Electric Medical Systems Integrated Imaging Solutions, Mt. Prospect, Ill., U.S.A.). One or two representative images for each of six organ systems, namely the brain, spine, heart, abdomen, extremities and face, were selected for review (Table 1). After reviewing the given standard planes obtained using the three techniques, the overall conspicuity of each organ system was subjectively assigned one of four grades (4 - excellent, 3 - good, 2 - fair, or 1- poor), depending on the definition of borders and internal structures. The grades were averaged between the readers, and CUS, THI, and PIHI were compared. During the review, each reader was blinded to the other's evaluation.
In the ten fetuses whose US findings were abnormal, the conspicuity of these anomalies was graded by one radiologist, using the same system. Grades for the three different techniques were then compared.
For multiple statistical comparison between the three techniques, Friedman's test was used; a p value of less than 0.05 was considered statistically significant. To establish interobserver agreement, individual data sets from the two readers were compared. CUS, THI and PIHI were quantified using their weighted kappa value, with a 95-percent confidence interval.
A comparison of overall conspicuity and definition of the borders and internal structures of the six organ systems, as seen at CUS, THI, and PIHI, appears in Table 2. For the brain, heart, abdomen and face, the overall conspicuity of fetal organs was significantly better at THI and PIHI than at CUS (Fig. 1) (p < 0.05), though there was no significant difference between THI and PIHI. For the spine (Fig. 2) and extremities, THI and PIHI were not significantly different from CUS. In two first-trimester fetuses, THI and PIHI delineated internal structures better than CUS (Fig. 3), though this small number of fetuses made statistical analysis impossible.
In the ten abnormal fetuses, the abnormality was more clearly delineated at both THI and PIHI than at CUS (p < 0.05) (Table 3). This was so, for example, for a body-wall defect and a liver-containing sac in the fetus with omphalocele. The dilated renal pelvis present in two fetuses was clearly depicted using all three techniques, though soft-tissue contrast was slightly better and the near-field artifact was smaller at THI and PIHI than at CUS (Fig. 4). In the two fetuses with echogenic thoracic masses, the lesions contrasted better with surrounding normal lung at THI and PIHI than at CUS. In the two fetuses with a facial cleft, the lesions were clearer at THI and PIHI than at CUS.
The overall kappa value was 0.845 (very good agreement), with a 95 percent confidence interval of 0.831-0.888. For the three techniques, all kappa values calculated ranged between 0.711 and 1.000 (Table 4).
Owing to the presence of a natural sonic window of amniotic fluid, US is the most suitable modality for the diagnosis of fetal abnormalities, and its safety and availability have facilitated its wide use in nearly all pregnancies. CUS is, however, of limited utility for the evaluation of obese patients and those with poly- or oligohydramnios, uterine anomalies, or multiple myomas (20-21).
THI is a US technique in which the US beamformer transmits at one frequency and the transducer receives at twice that frequency (harmonic frequency). Using a filter to process the received signal, only the returning second harmonic signal is used to produce the image. The use of a narrow US beam width provides better lateral resolution and improved depiction of the details of small anatomic structures (24-25). Additionally, because of the smaller dynamic range involved, tissue contrast resolution is accentuated, and since nonlinear propagation causing waveform distortion and the diffraction effect is less, THI produces fewer artifacts than CUS (25).
PIHI is a newer technique free of the bandwidth limitation of THI (9). By transmitting two mirror-imaged pulses of alternating phases, the fundamental signals are cancelled out, generating a pure harmonic signal (26), and very high spatial resolution is known to result. While THI uses a narrow receiving filter, PIHI uses broader transmitting and receiving bandwidths, and resolution is thus improved (24). The well-known disadvantages of PIHI are its slow frame rate and flashing artifacts, though in fetal imaging these do not seem to often cause problems.
Soft tissues, including the skin, subcutaneous tissue and musculature, seem to be more conspicuous at THI than at CUS. In our study, THI and PIHI were superior to CUS for the brain, heart, and abdomen, but PIHI was better than CUS for evaluation of the face. In contrast, bony structures were not clearly delineated at THI or PIHI; they were more often obscured by clear posterior sonic shadowing of bones than at CUS (Fig. 2), a fact which may explain the lower grades of conspicuity seen at THI and PIHI of the spine and extremities. For these areas, there were no statistically significant differences between the three techniques.
The conspicuity of all six organ systems and overall image quality were similar at PIHI and at THI, though among the three techniques, near-field artifacts in fetal brain beneath the calvarium and in fetal abdomen beneath the abdominal wall were smallest at PIHI (Fig. 4).
Published reports have not addressed the question of the safety of THI and PIHI in fetal imaging. Although Egerton et al. (27) reported possible increases in tissue temperature during harmonic imaging, THI and PIHI without contrast appear, in theory, to be safe in an ordinary clinical setting. THI obtains weak harmonic signals generated in the body, and except for the selection of a narrower bandwidth frequency, the transmitted sound beam remains the same as with CUS. PIHI uses two sound pulses per scan line, resulting in more sound energy per line; as the frame rate is halved, however, average sound energy over time is the same. For this reason, both the thermal and mechanical indices encountered in clinical practice, using either technique, usually remain the same as with CUS.
Interobserver agreement in our study was very good, with close correlation between the findings of the two reviewers, an overall weighted kappa value of 0.845, and a 95-percent confidence range of 0.831-0.888. There was very close agreement (0.711-1.000 of the weighted kappa value) between the two observers for both normal and abnormal fetuses, and all six organ systems. This result demonstrates, we believe, that both THI and PIHI are consistently superior to CUS and can thus serve as useful tools for imaging of the fetus.
Our study suffers certain limitations. First, since the image characteristics of the three different techniques were recognizably different, the readers were not blinded, during their analysis, to which had been employed. Second, we included in this study only patients who visited our department for level-II fetal US, and for this reason, the gestational age of the fetuses varied, and was not well controlled. Fetal imaging findings are strongly influenced by gestational age, and our THI and PIHI findings may, for this reason, have been affected. Third, only ten abnormal fetuses were studied, and to determine the usefulness of these techniques and the applicability of our findings, further investigation by means of a well-designed prospective study is warranted.
In conclusion, both THI and PIHI are superior to CUS for the evaluation of normal and abnormal fetuses, particularly for assessment of the brain, heart, abdomen, and face. Because it provides high tissue contrast resolution and artifacts are fewer, harmonic imaging may be particularly useful in the evaluation of internal fetal organs.
Figures and Tables
 | Fig. 1Transverse views of fetal abdomen: (A) CUS, (B) THI, (C) PIHI. Soft-tissue contrast is better at B and C than at A. Artifactual hypoechoic areas in the right lobe of the liver near the transducer (arrowheads) are smaller at B and C than at A, and smallest at C. |
 | Fig. 2Longitudinal scans of fetal cervical spine: (A) CUS, (B) THI, (C) PIHI. The margins of bony structures are clearer at A, since the posterior sonic shadowing of the individual bones is less prominent. Soft tissue contrast, however, seems to be higher at B and C. Layers of suboccipital scalp (arrowheads) are clearly demonstrated at B, and the spinal cord (arrows) is clearly visible at C. |
 | Fig. 3Transverse scan of the fetal head at 12 weeks' gestation: (A) CUS, (B) THI, (C) PIHI. The choroid plexuses (arrows) present in lateral ventricles are clearly visible at C, but internal structures are not clearly depicted at A. |
 | Fig. 4Transverse scan through fetal kidneys: (A) CUS, (B) THI, (C) PIHI. The dilated renal pelvis (arrows) is clearly demonstrated by all three techniques, though soft tissue contrast is clearest at PIHI. Note the presence of the smallest near-field artifact (arrowheads) at PIHI. |
Table 2
Comparison of the Conspicuity of the Six Organ Systems, as Seen at Conventional US, Tissue Harmonic Imaging, and Pulse-Inversion Harmonic Imaging

Table 3
Comparison of the Overall Conspicuity of Abnormal Organs, as seen at Conventional US, Tissue Harmonic Imaging, and Pulse-Inversion Harmonic Imaging
References
1. Tranquart F, Grenier N, Eder V, et al. Clinical use of ultrasound tissue harmonic imaging. Ultrasound Med Biol. 1999. 25:889–894.
2. Caidahl K, Kazzam E, Lidberg J, et al. New concept in echocardiography: harmonic imaging of tissue without use of contrast agent. Lancet. 1998. 352:1264–1270.
3. Lindner JR, Villanueva FS, Dent JM, et al. Assessment of resting perfusion with myocardial contrast echocardiography: theoretical and practical considerations. Am Heart J. 2000. 139:231–240.
4. Spencer KT, Bednarz J, Rafter PG, et al. Use of harmonic imaging without echocardiographic contrast to improve two-dimensional image quality. Am J Cardiol. 1998. 82:794–799.
5. Schwarz KQ, Chen X, Steinmetz S, et al. Harmonic imaging with Levovist. J Am Soc Echocardiogr. 1997. 10:1–10.
6. Postert T, Federlein J, Weber S, et al. Second harmonic imaging in acute middle cerebral artery infarction: preliminary results. Stroke. 1999. 30:1702–1706.
7. Seidel G, Greis C, Sonne J, et al. Harmonic gray scale imaging of the human brain. J Neuroimaging. 1999. 9:171–174.
8. Hann LE, Bach AM, Cramer LD, et al. Hepatic sonography: comparison of tissue harmonic and standard sonography techniques. AJR Am J Roentgenol. 1999. 173:201–206.
9. Kono Y, Moriyasu F, Nada T, et al. Gray scale second harmonic imaging of the liver: a preliminary animal study. Ultrasound Med Biol. 1997. 23:719–726.
10. Jang HJ, Lim HK, Lee WJ, Kim SH, Kim KA, Kim EY. Ultrasonographic evaluation of focal hepatic lesions: comparison of pulse-inversion harmonic, tissue harmonic, and conventional imaging techniques. J Ultrasound Med. 2000. 19:293–299.
11. Shapiro RS, Wagreich J, Parsons RB, et al. Tissue harmonic imaging sonography: evaluation of image quality compared with conventional sonography. AJR Am J Roentgenol. 1998. 171:1203–1206.
12. Desser TS, Jeffrey RB Jr, Lane MJ, Ralls PW. Tissue harmonic imaging: utility in abdominal and pelvic sonography. J Clin Ultrasound. 1999. 27:135–142.
13. Sehgal CM, Arger PH, Pugh CR, Kirchofer JI, Kotlar EY, Bovee KC. Comparison of power Doppler and B-scan sonography for renal imaging using a sonographic agent. J Ultrasound Med. 1998. 17:751–756.
14. Claudon M, Barnewolt CE, Taylor GA, et al. Renal blood flow in pigs: changes depicted with contrast-enhanced harmonic US imaging during acute urinary obstruction. Radiology. 1999. 212:725–731.
15. Taylor GA, Barnewolt CE, Claudon M, et al. Depiction of renal perfusion defects with contrast-enhanced harmonic sonography in a porcine model. AJR Am J Roentgenol. 1999. 173:757–760.
16. Schmiedl UP, Carter S, Martin RW, et al. Sonographic detection of acute parenchymal injury in an experimental porcine model of renal hemorrhage: gray-scale imaging using sonographic contrast agent. AJR Am J Roentgenol. 1999. 173:1289–1294.
17. Kim B, Lim HK, Choi MH, et al. Detection of parenchymal abnormalities in acute pyelonephritis by pulse-inversion harmonic imaging with or without microbubble US contrast agent: correlation with CT. J Ultrasound Med. 2001. 20:5–14.
18. Callen PW. Callen PW, editor. The obstetric ultrasonographic examination. Ultrasonography in obstetrics and gynecology. 2000. 4th ed. Philadelphia, Pensylvania, U.S.A.: W. B. Saunders Company;1–16.
19. Lee SH, Cho JY, Song MJ, et al. Prenatal ultrasound findings of fetal neoplasms. Korean J Radiol. 2002. 3:64–73.
20. Ozkutlu S, Saraclar M. The accuracy of antenatal fetal echocardiography. Turk J Pediatr. 1999. 41:349–352.
21. Barnhard Y, Bar-Hara I, Divon MY. Accuracy of intrapartum estimates of fetal weight: effect of oligohydramnios. J Reprod Med. 1996. 41:907–910.
22. Sivit CJ, Hill MC, Larsen JW, et al. The sonographic evaluation of fetal anomalies in oligohydramnios between 16 and 30 weeks gestation. AJR Am J Roentgenol. 1986. 146:1277–1281.
23. Cohen J. A coefficient of agreement for nominal scales. Educational Psychological Measurement. 1960. 20:37–39.
24. Powers J, Averkiou M, Hope-Simpson D. Contrast imaging methods. 1998. In : Proceedings of the First Annual Symposium on Ultrasound Contrast for Radiological Diagnosis; 2-3 October; Toronto, Canada. –18.
25. Senior R, Soman P, Khattar RS, et al. Improved endocardial visualization with second harmonic imaging compared with fundamental two-dimensional echocardiographic imaging. Am Heart J. 1999. 138:163–168.
26. Bauer A, Hauff P, Lazenby J, et al. Wideband harmonic imaging: a novel contrast ultrasound imaging technique. Eur Radiol. 1999. 9:Suppl 3. S364–S367.
27. Egerton IB, Vella G, Barnett S. Experimental test of harmonic contribution to the thermal index for soft tissue. J Ultrasound Med. 1999. 18:81–86.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download