This article has been retracted. See "Notice of Redundant Publication" in Volume 7 on page 152.
Abstract
Objective
Primary small cell carcinoma (SCC) is a rare aggressive malignancy of the urinary bladder, with identical histopathology to that of the lung. The treatment and prognosis of bladder SCC are somewhat different from those of more frequent transitional cell carcinoma. The purpose of this study was to analyze the CT and MR imaging findings of bladder SCC.
Materials and Methods
Six adult patients (five males and one female) with pathologically proven SCC of the urinary bladder who had undergone pelvic CT and/or MR imaging were included in this study. The radiologic findings were retrospectively evaluated in terms of tumor location, texture, calcification, depth of invasion, perivesical extension, lymph node involvement, and local or distant metastasis, by two radiologists, who established a consensus.
Results
CT and MR images depicted all tumors as large, ill-defined, relatively well enhancing, broad-based polypoid intramural masses with (n=3) or without (n=3) cystic portions. Their frequent location was posterior and trigonal (n=3). Calcification was found within one tumor, and lymphadenopathy in four. At T2-weighted MR images, the solid portion of the tumor was relatively hypointense. The stage at the time of diagnosis was C in three patients, and D1 in three. Follow-up imaging showed brain metastasis in one patient and liver metastasis in two.
Conclusion
On CT and MR images, SCC of the urinary bladder appeared as a large, enhancing, broad-based polypoid mass. It was stage C or higher, and lymph nodes and distant metastasis were frequent. T2-weighted MR images showed that the solid portion of the tumor was relatively hypointense. When radiologic examinations demonstrate a bladder tumor of this kind in adults, SCC of the urinary bladder should be included in the differential diagnosis.
Primary small cell carcinoma (SCC) of the urinary bladder, histopathologically analogous to that observed in the lung, is known to be a rare aggressive high-grade malignant neoplasm (1-8). Since the first report in 1981 by Cramer et al (1), approximately 150 cases were reported worldwide prior to November 2001 (2): the studies dealt mainly with the lesions' pathology, cytology, urology, or urologic oncololy. In contrast to the frequency of lung SCC, SCC of the urinary bladder accounts for only 0.48-1% of all bladder malignancies (3-6). Most patients with this bladder tumor have shown at least muscular invasion at the time of diagnosis and their clinical course has been highly aggressive, with early and widespread metastasis (1-7) and a poor overall survival rate (2). Transurethral resection, commonly applied in early-stage transitional cell carcinoma (TCC) of the bladder, is known to be ineffective in the treatment of patients with SCC of the bladder (6, 7, 9. 10). Published reports have described diverse trials, including systemic platinum or cisplatin-based chemotherapy, surgery (such as radical cystectomy or cystoprostatectomy), radiotherapy, and various combination therapies (2, 7-11).
In spite of the relatively well known histopathology and clinical outcome of this rare bladder SCC, radiologic reports describing its imaging features have not, to our knowledge, so far been published.
The purpose of this study was to describe the computed tomography (CT) and magnetic resonance (MR) imaging findings of six patients with SCC of the urinary bladder, encountered during a recent three-year period.
Between January 2000 and January 2003, six cases of pathologically proven SCC of the urinary bladder were retrospectively identified at our hospital and at other associated institutions. All patients were adults (M:F=5:1), and were aged between 44 and 66 (mean, 56.8) years. Preoper-ative CT was performed in all six patients, and supplementary MR imaging in two.
For CT or MR imaging, the bladder was not filled with air or fluid. For CT, a High Speed Advantage CTi Standard scanner(General Electric Medical Systems, Milwaukee, Wis., U.S.A) or a Somatom Plus VD30 (Siemens Medical Systems, Erlangen, Germany) was used. After pre-contrast pelvic CT, post-contrast CT was performed with 5-mm slice thickness and 3-5-mm collimation (1 pitch, helical CT) at 5-mm slice intervals, following the bolus injection of Ultravist 300ⓡ (Iopromide 0.6234 g/ml, 140-150 cc, Schering AG, Berlin, Germany). Using a GE Signa 1.5 T MR unit (General Electric Medical Systems), MR imaging was performed in two patients. After the intravenous injection of Magnevistⓡ (gadopentetate dimeglumine, 0.1 mmol/Kg, Schering AG), T1-weighted images (TR/TEeff 410-660/11-17 msec), fast spin-echo T2-weighted images (TR/TE 3,200-6,000/85-132 msec; echo train length=8, 12) and gadolinium-enhanced T1-weighted images were obtained in the axial, coronal, and sagittal planes, with parameters of 4-5 mm slice thickness with a 1-5-mm gap, a 22×22-cm field of view, 512×224 matrix and 1.5-4 excitations.
The patients underwent radical (n=3), partial (n=2), or total (n=1) cystectomy, and the radiologic findings were retrospectively evaluated by two radiologists who reached a consensus. Tumors were retrospectively evaluated in terms of their location, size, appearance or texture, margin, calcification, depth of invasion, perivesical extension, lymph node involvement, and local or distant metastasis. Staging was classified according to the Jewett-Strong-Marshall system (8).
The demographic, imaging and clinical findings of SCC of the urinary bladder are summarized in Table 1.
At the time of initial diagnosis, four of six patients presented with gross hematuria, one with bladder irritability, and one with suprapubic pain. Chest radiographs or chest CT revealed no mass-like lesion suggesting primary small cell lung carcinoma in any of the six patients.
At CT and MR imaging, all six tumors appeared as large, broad-based polypoid masses (Figs. 1-3). Their location within the urinary bladder was posterior and trigonal in three patients (Figs. 1 and 3), and anterior and trigonal (Fig. 2), anterior and right lateral, and anterior and left lateral, respectively, in the other three. The maximal diameter of the six tumors ranged from 3.0 to 8.2 (mean, 5.0) cm. All were enhanced at post-contrast CT [four were well enhanced (70-90 HU) and the other two were slightly enhanced (40-60 HU)] and at post-contrast MR imaging. Unenhanced cystic or necrotic portions, occupying less than one third of the whole tumor volume, were noted in three tumors (Figs. 2 and 3). Calcification within the tumor was found in one patient (Fig. 3). At the time of diagnosis, whole-layer muscular invasion with perivesical extension had occurred in all six cases (Figs. 1-3). Three tumors were Jewett-Strong-Marshall stage C (Fig. 2), and the other three were D1 (Figs. 1 and 3). Among the three patients with a tumor at this latter stage, there was involvement of both seminal vesicles and the left distal ureter in one male (Fig. 1), of the anterior vagina wall and both ureters in one female (Fig. 3), and of the right seminal vesicle in the other male. In two patients who underwent MR imaging studies, the signal intensity of the solid portions of the tumors was low at T1-weighted imaging and relatively low or similar to those of pelvic muscles at T2-weighted imaging (Fig. 3). Pelvic lymph node involvement was found in three patients at presentation (Figs. 2 and 3); and during follow-up, distant lymph node metastasis was noted in two patients, brain metastasis in one (Fig. 2), and liver metastasis in two. These three last-mentioned all expired within one year of initial diagnosis.
A rare primary SCC of the urinary bladder is, like SCC of the lung, highly aggressive, and involves early and widespread metastasis (1-10). The five-year survival rate for patients with SCC of the bladder is 8.1% (9) compared to 5-10% for lung cancer (2); in those whom this cancer attacks, the tumor is usually at an advanced stage by the time of diagnosis (11). Most frequently, there is metastasis to local or distant lymph nodes, the liver, bone, the lung, brain, adrenal gland, spleen, or abdominal cavity (10). In our study, the maximal diameter of six tumors ranged from 3.0 to 8.2 (mean, 5.0) cm, suggesting that at presentation, a bladder SCC is larger than a TCC, though the latter is more frequent. Initial CT or MR imaging revealed that in all tumors, whole-layer muscular invasion, with perivesical extension, had occurred (stage C in three patients and stage D1 in another three), and three of the six patients succumbed to brain or liver metastasis within one year of initial diagnosis.
SCC of the urinary bladder is a rare tumor occurring typically in older men who present with gross hematuria (7), which is the most frequent clinical symptom (11). Abbas et al. (10) found that among 97 males and 27 females with bladder SCC, the median age at presentation was 66.1 years. Among six patients in our study, four presented with gross hematuria, one with bladder irritability, and one with suprapubic pain. The mean age of the six was 56.8 years, slightly younger than reported by Abbas et al. Our study also demonstrated male predominancy, i.e. five of six patients were male.
An SCC has a characteristic microscopic appearance, namely sheets and nests of small round tumor cells containing hyperchromatic nuclei. Most show immunohistochemical staining with neuroendocrine differentiation markers (2), a result consistent with the pathologic findings detailed in our study. The histogenesis of SCC of the bladder remains unclear, with three possible explanations (12). First, the tumor may arise from a neuroendocrine stem cell present in the urothelium of the bladder. The second possibility is that these tumors arise from poorly defined submucosal or muscularis cells of neural crest origin. Finally, SCC may result from a metaplastic transformation of TCC, a possibility which would explain the coexistence of TCC in up to two thirds of patients diagnosed with SCC (13). In our study, however, we found no such coexistence.
For treatment of SCC of the urinary bladder, various approaches have been tried: systemic platinum- or cisplatin-based chemotherapy, surgery (such as radical cystectomy or cystoprostatectomy), radiotherapy, and various combination therapies (2, 6-10). All our patients underwent adjuvant chemotherapy and/or radiotherapy in addition to cystectomy.
In our study, CT and MR imaging depicted all the tumors as large, broad-based polypoid masses, at stage C or higher, and with or without cystic or necrotic portions. All were relatively well enhanced at post-contrast CT and MR imaging. At the time of their diagnosis, they had already penetrated the whole layer of the bladder wall, with or without invasion of adjacent organs (such as a seminal vesicle, the ureter, or vagina) or lymph nodes. In two patients who underwent MR imaging, the solid portions of the tumors were hypointense on both T1- and T2-weighted images (Fig. 3), though why the tumor should have shown relatively low signal intensity, especially on T2-weighted images, is not clear. We suggest, however, that the high cellularity of bladder SCC may play a role in this.
The differential diagnosis of primary SCC of the urinary bladder includes metastasis from a SCC outside of the bladder (an SCC of the prostate, for example), a poorly differentiated TCC, and primary or secondary lymphomas (7). Clinically, SCC of the lung seldom metastasizes symptomatically to the urinary bladder (14). Prostatic SCC, with a worse prognosis than bladder SCC (14), contains an adenocarcinomatous component in more than 50% of cases, and this shows a positive reaction for prostate-specific antigen and prostatic acid phosphatase (15). Grossly, SCC of the urinary bladder, unlike TCC, appears as a polypoid intramural mass with a broad base (5). Thus, when such a mass is observed in the urinary bladder at imaging studies, a rare SCC - as well as more frequent TCC - should be considered as the differential diagnosis. In our study, however, all cases were falsely diagnosed as TCC: in none of our patients did chest radiographs or chest CT indicate the presence of a mass lesion suggesting primary SCC of the lung.
In conclusion, the CT and MR images obtained in our study depicted SCC of the urinary bladder as a large, broad-based polypoid mass, at stage C or higher. On T2-weighted MR images, the solid portion of the tumor tended to be relatively hypo- or isointense to adjacent muscle. When radiologic examinations demonstrate a bladder tumor of this kind in adults, SCC of the urinary bladder should be included in the differential diagnosis.
References
1. Cramer SF, Aikawa M, Cebelin M. Neurosecretory granules in small cell invasive carcinoma of the urinary bladder. Cancer. 1981; 47:724–730. PMID: 6261916.

2. Fujita K, Nishimura K, Nonomura N, Hirota S, Okuyama A. Early stage small cell carcinoma of the urinary bladder. Int J Urol. 2001; 8:643–644. PMID: 11903694.

3. Trias I, Algaba F, Condom E, et al. Small cell carcinoma of the urinary bladder. Presentation of 23 cases and review of 134 published cases. Eur Urol. 2001; 39:85–90. PMID: 11173944.
4. Blomjous CEM, Vos W, de Voogt HJD, Valk PVD, Meijer CJLM. Small cell carcinoma of the urinary bladder: a clinicopathologic, morphometric, immunohistochemical, and ultrastructural study of 18 cases. Cancer. 1989; 49:1347–1357. PMID: 2548704.

5. Lopez JI, Angulo JC, Flores N, Toledo JD. Small cell carcinoma of the urinary bladder: a clinicopathological study of six cases. Br J Urol. 1994; 49:43–49. PMID: 7507782.

6. Holmang S, Borghede G, Johansson SL. Primary small cell carcinoma of the bladder: a report of 25 cases. J Urol. 1995; 153:1820–1822. PMID: 7752326.

7. Nejat RJ, Purohit R, Goluboff ET, Petrylak D, Rubin MA, Benson MC. Cure of undifferentiated small cell carcinoma of the urinary bladder with M-VAC chemotherapy. Urol Oncol. 2001; 6:53–55. PMID: 11166621.

8. Marshall VF. The relation of the preoperative estimate to the pathologic demonstration of the extent of vesical neoplasm. J Urol. 1952; 68:714. PMID: 12991380.
9. Farhat A, Francisco C, Pasquale B, Soloway MS. Small cell carcinoma of the bladder and prostate. Urology. 1995; 46:617–630. PMID: 7495110.

10. Abbas F, Civantos F, Benedetto P, et al. Small cell carcinoma of the bladder and prostate. Urology. 1995; 46:617–629. PMID: 7495110.

11. Grignon DJ, Ro JY, Ayala AG, et al. Small cell carcinoma of the urinary bladder: a clinicopathologic analysis of 22 cases. Cancer. 1992; 49:527–536. PMID: 1309435.

12. Oesterling JE, Brendler CB, Burgers JK, et al. Advanced small cell carcinoma of the bladder. Successful treatment with combined cystoprostatectomy and adjuvant methotrexate, vinblastine, doxorubicin, and cisplatin chemotherapy. Cancer. 1990; 65:1928–1936. PMID: 2164873.
13. Kuroda N, Hayashi Y, Nishida Y, Itoh H. Combined small and transitional cell carcinoma of the urinary bladder with CA19-9 production. Pathol Int. 1999; 49:462–467. PMID: 10417692.

14. Mackey JR, Au HJ, Hugh J, Venner P. Genitourinary small cell carcinoma: determination of clinical and therapeutic factors associated with survival. J Urol. 1998; 159:1624–1629. PMID: 9554367.

Fig. 1
A 56-year-old male with stage-D1 SCC of the urinary bladder (Case 2).
Post-contrast pelvic CT images (A and B) depict a broad-based polypoid mass (m) with nonenhancing cystic or necrotic portions in the left posterior and trigonal area of the urinary bladder. Note the aggressiveness with which this tumor invades seminal vesicles (s), and obliteration of the left ureter.
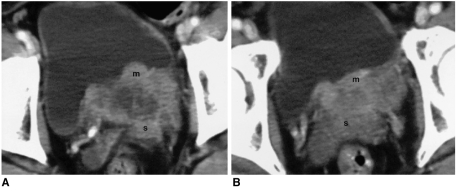
Fig. 2
A 44-year-old male with stage-C bladder SCC metastasizing to the brain (Case 1).
Pre-contrast (A and B) and post-contrast pelvic CT images (C and D) demonstrate a well-enhancing intramural mass in and beyond (arrow) the anterior wall of the urinary bladder and bilateral iliac lymph nodes (n). Another mass in the trigonal area, and multiple distant lymph nodes, are not shown here. Postoperative follow-up brain CT (E) revealed the presence of multiple metastatic nodules (arrowheads), and this patient eventually succumbed to this widespread metastasis (stage D2).

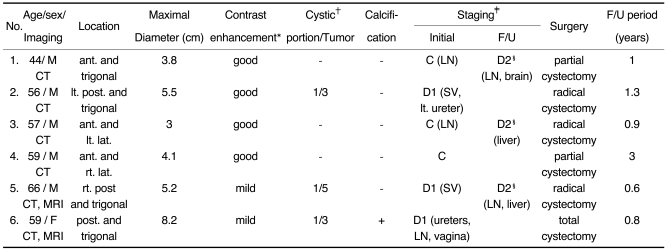
Fig. 3
A 59-year-old female with stage D1 SCC of the urinary bladder (Case 6).
A, B. Pre-contrast (A) and post-contrast (B) pelvic CT reveals a heterogeneously enhancing irregular mass in and beyond the posterior wall of the urinary bladder. At the anterior aspect of the mass, there is calcification (arrowhead). Note the exophytic posterior portion of the tumor beyond the bladder wall (arrow), and left pelvic lymphadenopathy (n).
C-E. Axial T1-weighted (C), T2-weighted (D), and post-contrast T1-weighted (E) pelvic MR images reveal that the tumor, which invades the anterior vaginal wall (v) and pelvic lymph nodes (n), has both enhancing solid portions and non-enhancing cystic or necrotic portions. A Foley catheter (f) is seen within the bladder. The T2-weighted image shows that the peripheral solid portions of the tumor (arrows) are relatively hypo- or isointense compared with the anterior bladder wall.
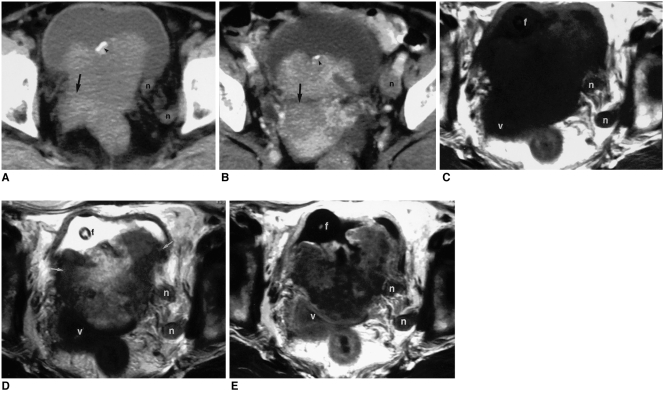
Table 1
Summary of the Imaging and Clinical Findings of Small Cell Carcinoma of the Urinary Bladder
Note.-M=male, F=female, *=HU at post-contrast CT scanning (good = 70 90 HU, mild = 40-60 HU), †=volume of cystic portion / volume of whole tumor ‡=Staging according to Jewett-Strong-Marshall system, F/U=follow-up period, rt=right, lt=left, ant.=anterior, post.=posterior, CT=computed tomography MRI=magnetic resonance imaging, SV=seminal vesicle, LN=lymph node involvement, §= expired patients



