Abstract
Papillary tumor of the bile duct is characterized by the presence of an intraductal tumor with a papillary surface comprising innumerable frondlike infoldings of proliferated columnar epithelial cells surrounding slender fibrovascular stalks. There may be multiple tumors along the bile ducts (papillomatosis or papillary carcinomatosis), which are dilated due to obstruction by a tumor per se, by sloughed tumor debris, or by excessive mucin. Radiologically, the biliary tree is diffusely dilated, either in a lobar or segmental fashion, or aneurysmally, depending on the location of the tumor, the debris, and the amount of mucin production. A tumor can be depicted by imaging as an intraductal mass with a thickened and irregular bile duct wall. Sloughed tumor debris and mucin plugs should be differentiated from bile duct stones. Cystically or aneurysmally, dilated bile ducts in mucin-hypersecreting variants (intraductal papillary mucinous tumors) should be differentiated from cystadenoma, cystadenocarcinoma and liver abscess.
Papillary tumor of the bile ducts is a distinctive pathologic entity characterized by the presence of intraluminal papillary tumors of the intra- and/or extrahepatic bile ducts, and is associated with bile duct obstruction and dilatation (1-4). The latter may be lobar, segmental, generalized, or cystic in appearance depending upon the location of a tumor (Fig. 1). Intraductal papillary tumor of the bile ducts is rare, but probably because of recent developments in diagnostic technology, clinicians and radiologists have encountered increasing number of cases (1). Since it is often misdiagnosed as stones, or remains unrecognized for long periods, the true incidence of the condition is perhaps underestimated (1). In this essay, we describe the radiological manifestations of this disease based on the pathologic findings.
The clinical symptoms and signs of intraductal papillary tumor of the bile ducts are caused by partial or complete biliary obstruction either by a tumor per se, by sloughed tumor debris, or by a copious amount of mucus (1, 5). Diagnosis is usually based on the findings of imaging studies demonstrating bile duct dilatation and intraductal tumors. Because papillomatous tumors are low-grade malignancies, are usually limited to the mucosa, and can invade the ductal wall at a late stage, early diagnosis is important. After surgical resection, a benign course and long survival can be expected (1, 3, 5).
An intraductal papillary tumor is nodular or flat and is characterized by the presence of innumerable, papillary, frondlike infoldings consisting of proliferation of the columnar epithelial cells surrounding the slender fibrovascular stalks supported by connective tissue from the lamina propria (Fig. 2). The tumor often spreads along the mucosal surface but may invade the ductal wall, including its outer surface (1, 3-5). Along the bile ducts, tumors are usually multiple (papillomatosis), involving a fairly wide area of both the intra- and extrahepatic bile ducts (1, 2, 5-7). Histologically, the lesion may be an intraductal papillary adenocarcinoma, adenoma or dysplasia, and various histologic patterns frequently coexist (2, 5). The tumor is friable and sloughs easily, and sometimes produces a profuse amount of mucus, resulting in partial biliary obstruction (5-7).
At sonography, CT or MR cholangiography, the bile ducts of the involved hepatic segment, hepatic lobe or entire biliary tree are seen to be dilated. When the tumor involves a segment or one hepatic lobe, the degree of bile duct dilatation is thus particularly severe, and the dilated bile duct appears crowded (Fig. 3). At ultrasonography, an introductal mass is usually echogenic (Figs. 3-5). As it is confined within the bile ducts, the echogenic walls remain intact (2). At CT, an intraductal papillary tumor can appear as a hypo- or isoattenuating soft tissue mass within the dilated duct relative to the hepatic parenchyma, or as segmental thickening of the wall of the bile ducts (3, 4) (Figs. 3 and 4). At contrast enhanced CT, attenuation may be increased, and the outer margin of the thickened bile duct wall is smooth and clear. When it is small and isoattenuating to adjacent hepatic parenchyma, or when complex orientation of the dilated bile ducts obscures the presence of a mass, a tumor is not always depicted (3, 4). At endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography, the biliary tree is diffusely dilated, and biliary obstruction is usually partial. A tumor may be small and flat, and the ductal wall is sometimes irregular (2-4). A mass reveals fine surface irregularities, either in the form of a velvety or serrated contour, representing the tumor's papillary surface (Figs. 4 and 5). The gallbladder and cystic duct may also be involved (Fig. 5). It is impossible to differentiate benign from malignant papillary tumors solely on the basis of the radiological findings.
Some papillary tumors of the bile ducts produce a large amount of mucin (5-7) and may occasionally impede the flow of bile juice, leading to obstructive jaundice. Endoscopy may demonstrate a mucin plug protruding from the patulous orifice of the duodenal papilla (5). In terms of its histopathology and pathophysiology, and the production of excess mucin, this tumor has a striking similarity to intraductal papillary tumor of the pancreas.
Sonography, CT, and MR cholangiopancreatography demonstrate severe dilatation of the intra- and extrahepatic ducts (Fig. 6); both proximal and distal to a tumor are dilated because mucin may obstruct the papilla of Vater. At CT, a tumor may appear as a small, flat mass, isoattenuating to adjacent liver tissue, while mucus is not visible. At sonography, a mucus plug usually echofree but may appear as a masslike, echogenic focus. It is difficult but not impossible to differentiate between a papillary tumor and mucus plugs or stones. Endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography may demonstrate that the dilated bile ducts contain large or small, multiple, amorphous filling defects caused by mucus plugs (3, 5). The tumor may or may not be visible.
Intraductal papillary tumors are very friable and slough spontaneously (1). When a tumor grows to a certain size, it sloughs and floats in the bile duct or implants at other sites (papillomatosis) (Fig. 7). The floating tumor may then reside within the bile ducts, imbibing nutrients from bile juice and growing substantially. These sizable, floating tumors may occlude the papillary orifice or escape from the bile duct through the duodenal papillary orifice and then disappear radiologically and clinically. The term, 'Laputa tumor' has thus been coined.
Because both diseases caused bile duct dilatation and intraluminal masses or filling defects, intraductal papillary tumors of the bile ducts may be misdiagnosed as recurrent pyogenic cholangitis with bile duct stones. At sonography and cholangiography, mucus plugs or a sloughed (Laputa) tumor may be confused with stones (Fig. 7). Where recurrent pyogenic cholangitis involves focal bile duct stricture, the condition may be misdiagnosed as papillary tumor of the bile duct: both diseases may involve segmental or lobar bile duct dilatation in the absence of an identifiable mass or stone (Fig. 8). Mucinous cystadenoma and cystadenocarcinoma may be mucin hypersecreting and may communicate with the bile duct and may thus be difficult to differentiate from a papillary tumor, especially one that is cystic (7).
Figures and Tables
Fig. 1
Schematic drawing of intraductal papillary tumors of the biliary tract (A: carcinoma; B: adenoma; C: dysplasia; m: mucus).

Fig. 2
Microphotograph of papillary carcinoma demonstrates papillae comprising a fibrovascular core and a covering of columnar epithelial cells. The term 'papillary' derives from the frondlike papillary infoldings (arrows) (H & E staining, ×100).

Fig. 3
A 64-year-old man with papillary carcinoma arising in the left intrahepatic bile duct.
A. Transverse sonogram of the left lobe of the liver reveals a fairly well-defined oval echogenic mass measuring 1.5 cm in its lateral segment (arrows), as well as markedly dilated bile ducts.
B. CT image shows an intraluminal mass (arrow) and dilated peripheral bile ducts.
C. Photomicrograph of a gross specimen depicts intraductal papillary carcinoma. Note the presence of myriads of frondlike papillary infoldings into the lumen of the bile ducts (arrows) (H & E staining, ×10).

Fig. 4
A 63-year-old man with papillary adenomatosis in the common hepatic duct.
A. Sonogram reveals dilated extrahepatic bile ducts and an echogenic cast filling the common hepatic duct (curved arrows). Note the presence of a slit-like defect in the cast (arrow).
B. Post-contrast CT image shows the thickened wall of the extrahepatic bile duct (open arrow). Note that in the center of the duct, a slit-like lumen is present.
C. Endoscopic retrograde cholangiogram depicts a papillary tumor in the common hepatic duct (arrows) and severe dilatation of the intra- and extrahepatic bile ducts. Note the velvety appearance, serrated margin, and nodular filling defects of the involved segment.

Fig. 5
A 56-year-old woman with papillary adenomatosis in which multifocal foci of carcinomatous change are seen in the gallbladder and cystic duct.
A. Sonogram of the gallbladder reveals an echogenic mass with a ragged surface (arrows).
B. Post-contrast CT image depicts an enhancing mass (arrows) in the gallbladder.
C. Endoscopic retrograde cholangiogram indicates that the gallbladder mass has a nodular and velvety appearance (arrows).
D. Photograph of resected gallbladder depicts an irregular mass, velvety in appearance, comprised of myriads of papillary projections.

Fig. 6
A 54-year-old woman with a mucin-producing, intraductal mucosal-spreading, papillary adenocarcinoma causing cystic and tubular dilatation of the intrahepatic bile ducts, complicated by abscess and rupture. (illustrations referred to in reference 7, and have been used with the authors' permission.)
A. Contrast-enhanced CT scan of the left lobe obtained during the equilibrium phase shows balloon-like dilatation of the left lobar and segmental bile ducts (asterisk), as well as severe dilatation of surrounding peripheral bile ducts (arrows).
B. CT scan 9 cm caudal to A demonstrates cyst-like (asterisk) and tubular dilatation of the bile ducts of the caudate lobe. Note that in the right hepatic lobe, the bile duct is slightly dilated.
C. Endoscopic retrograde cholangiogram indicates that the extrahepatic bile ducts contain thread-and-streak-like multiple linear filling defects, representing mucus. The left hepatic duct is completely obstructed, and the right, partially so. In the right hepatic lobe, the bile duct is again slightly dilated.
D. Photomicrograph of a resected specimen depicts balloon-like dilatation of the bile ducts, which are covered with diffusely thickened fibrotic wall. The luminal surface of one duct is lined by short papillary infoldings (star) but on other surfaces, papillary infoldings are denuded (asterisks). The arrow points to tumor growth at Glisson's capsule, due to perforation of the cystic tumor (H & E staining, ×10).
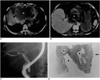
Fig. 7
A 59-year-old woman with papillary carcinomatosis in the left hepatic ducts and extrahepatic ducts.
A. CT image of the liver during the equilibrium phase shows markedly dilated, tortuous, crowded bile ducts in the left hepatic lobe. The percutaneous transhepatic catheter present in the extrahepatic duct is displaced posteriorly due to the intraluminal mass (arrow).
B. Percutaneous transhepatic cholangiogram demonstrates multiple nodular filling defects in the extrahepatic ducts (arrows), simulating multiple stones. Due to obstruction, the left hepatic duct is not opacified.

Fig. 8
A 62-year-old man with recurrent pyogenic cholangitis and resultant bile duct stricture.
A. Sonogram of the right hepatic lobe reveals substantially dilated posterior segmental bile ducts. There is no visible mass or stone.
B, C. Computed tomogram (B) and MR cholangiogram (C) depict dilated posterior segmental bile ducts with no identifiable mass or stone.

Acknowledgments
The authors wish to thank Bonnie Hami, of the Department of Radiology, University Hospitals of Cleveland for her copy-editing, and Young Joo Moon, Samsung Medical Center, for his assistance in manuscript preparation.
References
1. Kim YS, Myung SJ, Kim SY, et al. Biliary papillomatosis: clinical, cholangiographic and cholangioscopic findings. Endoscopy. 1998. 30:763–767.
2. Kawakatsu M, Vilgrain V, Zins M, Vullierme M-P, Belghiti J, Menu Y. Radiologic features of papillary adenoma and papillomatosis of the biliary tract. Abdom Imaging. 1997. 22:87–90.
3. Lee JW, Han JK, Kim TK, et al. CT features of intraductal intrahepatic cholangiocarcinoma. AJR. 2000. 175:721–725.
4. Yoon K-H, Ha HK, Kim CG, et al. Malignant papillary neoplasms of the intrahepatic bile ducts: CT and histopathologic features. AJR. 2000. 175:1135–1139.
5. Kim HJ, Kim MH, Lee SK, et al. Mucin-hypersecreting bile duct tumor characterized by a striking homology with an intraductal papillary mucinous tumor (IPMT) of the pancreas. Endoscopy. 2000. 32:389–393.
6. Hubens G, Delvaux G, Willems G, Bourgain C, Kloppel G. Papillomatosis of the intra- and extrahepatic bile ducts with involvement of the pancreatic duct. Hepatogastroenterology. 1991. 38:413–418.
7. Lim JH, Kim YI, Park CK. Intraductal mucosal-spreading, mucin-producing, peripheral cholangiocarcinoma of the liver. Abdom Imaging. 2000. 25:89–92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download