Abstract
Objective
To evaluate the radiographic and MR appearance of idiopathic synovial osteochondromatosis of the hip.
Materials and Methods
Radiographs and MR images of 15 patients with idiopathic synovial osteochondromatosis of the hip were assessed. The former were analysed in terms of the presence of 1) juxta-articular calcified and/ or ossified bodies, 2) osteophytes, 3) bone erosion, 4) juxta-articular osteopenia, and 5) joint space narrowing, while for the latter, analysis focused on 1) the configuration of intra-articular bodies, 2) bone erosion, 3) synovial thickening, 4) conglomeration of intra-articular bodies, and 5) extra-articular extension.
Results
At hip radiography, juxta-articular calcified and/ or ossified bodies were seen in 12 of the 15 patients (80%), bone erosion in eight (53%), osteophytes in seven (47%), juxta-articular osteopenia in five (33%) and joint space narrowing in five (33%). In eight patients (53%), MR imaging depicted intra-articular bodies of focal low signal intensity at all pulse sequences, and areas of iso-intensity at T1WI and hyperintensity at T2WI. In three (20%), intra-articular bodies of focal low signal intensity and areas of hyperintensity at all pulse sequences were observed, with areas of iso-intensity at T1WI and hyperintensity at T2WI, while in four (27%), intra-articular bodies of only focal low signal intensity at all pulse sequences were apparent. Synovial thickening was present in 13 patients (87%), bone erosion in 11 (73%), conglomeration of the intra-articular bodies in 11 (73%), and an extra-articular herniation sac in six (40%).
Conclusion
The most common radiographic finding of synovial osteochondromatosis of the hip was the presence of juxta-articular calcified and/ or ossified bodies. MR imaging depicted intra-articular bodies of focal low signal intensity at all pulse sequences, with areas of iso-intensity at T1WI and hyperintensity at T2WI. In addition, the presence of an extra-articular herniation sac was not uncommon.
Idiopathic synovial osteochondromatosis is an uncommon benign monoarticular disorder of unknown cause characterized by proliferation and metaplastic transformation of the synovium, where there is cartilage formation (1-3). The knee is the most commonly affected joint, followed by the elbow, hip, and shoulder, although any other joint may be involved (3-15). Patients usually present with pain, swelling, and restricted movement, symptoms which often progress slowly for several years (3). The age range of affected patients is wide, but most present in the fourth or fifth decade of life; men are affected two to four more times frequently than women (3, 11). The condition is usually progressive and leads to early osteoarthritis. Currently accepted surgical treatment involves the removal of any free intra-articular bodies and complete resection of the involved synovium, although local recurrence is not uncommon (1-5, 13, 15).
The radiologic appearance of idiopathic synovial osteochondromatosis depends on the stage of the disease and the extent of calcification or ossification of the cartilaginous nodule (3, 5, 11). Synovial osteochondromatosis that develops within a bursa overlying an osteochondroma may simulate malignant transformation of the osteochondroma (12).
There are scattered reports of idiopathic synovial osteochondromatosis of the hip (13-16), but to more fully characterize the radiologic findings of this condition, with emphasis on the appearance at MRI, the MRI findings of 15 patients were retrospectively analysed.
Fifteen patients with histopathologically proven synovial osteochondromatosis of the hip were involved in this study. Previously described criteria (2, 3, 5, 17), including the greater number and uniformity in size of intra-articular bodies, and the absence of significant arthritic change, were used to differentiate between idiopathic and secondary synovial osteochondromatosis. The clinical symptoms were hip pain in 14 patients and a painful inguinal mass in one; the duration of these ranged from 6 months to 8 (mean, 3.9) years. Clinical records, pathologic results, and the radiologic findings were reviewed.
The patients [11 men and 4 women aged 20-59 (mean 37) years] underwent hip radiography and MR imaging. For the latter, a 1.5-T (Signa; General Electric Medical Systems, Milwaukee, Wis., U.S.A.) or a 1.0-T imager (Magnetom Impact; Siemens, Erlangen, Germany) was used. Spin-echo T1-weighted (400-700/10-40 [TR/TE]) and fast spin-echo T2-weighted (1500-5000/70-112 [TR/TE]) or turbo spin-echo T2-weighted MR images (3500-4500/80-95 [TR/TE]) were obtained in the axial, coronal, and sagittal planes. Using a field of view of 18-38 cm, two signals were acquired. Section thickness was 5-6 mm and section gap, 1-2 mm.
Hip radiographs and MR images were evaluated by two experienced musculoskeletal radiologists, who reached a consensus. Radiographs were analysed in terms of the presence of 1) juxta-articular calcified and/ or ossified bodies, 2) osteophytes, 3) bone erosion, 4) juxta-articular osteopenia, and 5) joint space narrowing.
For MR images, attention was focused on 1) the configuration of intra-articular bodies, 2) bone erosion, 3) synovial thickening, 4) conglomeration of the intra-articular bodies, and 5) extra-articular extension.
Idiopathic synovial osteochondromatosis was present in the right hip in eight patients, and in the left, in seven. At hip radiography, juxta-articular calcified and/ or ossified bodies were seen in 12 patients (80%) (Figs. 1A, 2A), bone erosion in eight (53%) (Fig. 3A), osteophytes in seven (47%) (Figs. 1A, 2A), juxta-articular osteopenia in five (33%) (Fig. 4A), and joint space narrowing in five (33%) (Fig. 4A). In one patient with bone erosion, this was extensive and circumferential, with scalloping of the femoral neck (Fig. 3).
In our series, no radiographic findings were normal. In the three patients with no juxta-articular calcified and/ or ossified body, other findings such as bone erosion, juxta-articular osteopenia or joint space narrowing were observed, a fact which may be related to the long duration of the disease (mean, 3.9 years).
In eight patients (53%), MR imaging depicted intra-articular bodies of focal low signal intensity at all pulse sequences, with areas of iso-intensity at T1WI and hyperintensity at T2WI. In three (20%), intra-articular bodies of focal low signal intensity and areas of hyperintensity at all pulse sequences were observed, with areas of iso-intensity at T1WI and hyperintensity at T2WI. In four (27%), intra-articular bodies of only focal low signal intensity at all pulse sequences were demonstrated. MR imaging revealed synovial thickening in 13 patients (87%) (Figs. 3, 4), bone erosion in 11 (73%) (Fig. 3), conglomeration of the intra-articular lesion in 11 (73%) (Fig. 1), and an extra-articular herniation sac in six (40%) (Figs. 1, 3).
Synovial osteochondromatosis is the term used to describe the conversion of synovial connective tissue to cartilage (1, 3, 16). The term idiopathic synovial osteochondromatosis has been used to describe a specific pathological process presenting in otherwise normal joints (3, 16, 20).
The radiographic features of idiopathic synovial osteochondromatosis include calcified and/ or ossified bodies in a joint free of arthritis. If the cartilaginous bodies are neither calcified nor ossified, radiographs may fail to suggest the presence of abnormality, creating a problem in the diagnosis of this condition (4). Associated radiographic features are bone erosion (4), occasional osteoarthritis (4, 16), and regional osteoporosis (4).
In the present study, juxta-articular calcified and/ or ossified bodies, bone erosion, osteophytes, juxta-articular osteopenia, and joint space narrowing were found to be present. In patients with idiopathic synovial osteochondromatosis of the hip, no radiographic findings were normal, though juxta-articular calcified and/ or ossified bodies were absent in three cases, a fact which may be related to the long duration of the disease (mean, 3.9 years). The presence of osteophytes, juxta-articular osteopenia, and joint space narrowing in our series reflects the early osteoarthritic changes occurring in this disorder. In one patient with bone erosion, extensive circumferential erosion with scalloping was found; this aggressive radiographic appearance was related to the presence of a large cartilaginous lesion (Fig. 3).
Our results showed that MR imaging is useful in the diagnosis of synovial osteochondromatosis of the hip, especially in cases in which juxta-articular calcified and/ or ossified bodies are not present.
As expected, the MR characteristics of synovial osteochondromatosis depend on the pulse sequence used and the presence and extent of calcification and/ or ossification (2). Reports have described the MR imaging appearance of hyaline cartilage-containing lesions as distinct, stating that a lobulated lesion of low-to-intermediate signal intensity at T1WI and high signal intensity at T2WI is present (2, 21).
In our study, MR imaging was more sensitive than radiography in the detection of both bone erosion and juxta-articular bodies. The high frequency of synovial thickening at MR imaging, caused by proliferative change in synovial membrane in idiopathic synovial osteochondromatosis (1), was pronounced.
Strikingly, MR imaging depicted conglomeration of the intra-articular lesion in 73% of patients, and the presence of herniation sacs in 40%, findings which were confirmed at surgery. These results are related, we believe, to the fact that the hip joint has a tighter capsule than other joints in the extremity, leading to marked compression of the intra-articular body and increased intra-articular pressure in affected hip joints. Appropriate surgical planning depends on an awareness of this MRI finding.
The present study has several potential limitations. First, radiographic and MR images were interpreted by two observers, via consensus; thus interobserver variability could not be determined. Second, although the methods used by earlier investigators were modified for our study, our analysis of synovial thickening did not involve measurement of the synovium (18, 19). Finally, due to the retrospective nature of the present study, detailed histologic reports that would have allowed better radiographic-pathologic correlation were not available.
In summary, our most common radiographic finding of idiopathic synovial osteochondromatosis of the hip was the presence of juxta-articular calcified and/ or ossified bodies. The MR imaging finding which suggested this diagnosis was the presence of intra-articular bodies of focal low signal intensity at all pulse sequences, with areas of iso-intensity at T1WI and hyperintensity at T2WI. In addition, the presence of an extra-articular herniation sac was not uncommon. These appearances should permit differentiation between idiopathic synovial osteochondromatosis and other causes of intra-articular pathology of the hip joints.
Figures and Tables
Fig. 1
A 52-year-old woman with idiopathic synovial osteochondromatosis of the left hip.
A. Anteoposterior radiograph of the left hip depicts juxta-articular calicified and/ or ossified bodies (arrowheads), and an osteophyte (straight arrow). Note that superior to the iliopubic line, a calcified and/or ossified body (curved arrow) is also present, suggesting intrapelvic extension of the lesion.
B. T1-weighted coronal MR image of the same patient shows an intra-articular lesion of low signal intensity (curved arrows), signal intensity which corresponds to an area of fat (straight arrow), and a conglomerated lesion (open arrow). Note that intrapelvic extension of the iliopsoas bursa has occurred (arrowheads).
C. T2-weighted image, obtained at the same level as in B, shows intra-articular bodies of focal low signal intensity (curved arrows), and a conglomerated lesion (straight arrow). Note that intrapelvic extension of the iliopsoas bursa is again apparent (arrowheads).
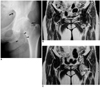
Fig. 2
A 37-year-old man with idiopathic synovial osteochondromatosis of the right hip.
A. Anteoposterior radiograph of the right hip demonstrates the presence of juxta-articular calicified and/or ossified bodies (arrowheads), and an osteophyte (arrow).
B. T1-weighted axial MR image of the same patient depicts intra-articular bodies of focal low signal intensity (open arrow) and areas of fat (straight arrow).
C. T2-weighted image, obtained at the same level as in B, shows intra-articular bodies of focal low signal intensity and central areas of hyaline cartilage (arrows).

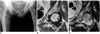
Fig. 3
A 31-year-old woman with idiopathic synovial osteochondromatosis of the right hip.
A. Anteoposterior radiograph of the right hip reveals extensive circumferential bone erosion and scalloping of the right femoral neck (arrows).
B. T1-weighted axial MR image of the same patient depicts extensive bone erosion (arrows).
C. T2-weighted image, obtained at the same level as in B, shows extensive bone erosion (arrowheads), intra-articular bodies without hyaline cartilage or fat (slender arrow), and an intra-articular body with central areas of hyaline cartilage (curved arrows).
D. T2-weighted image of the same patient demonstrates extensive bone erosion (arrowheads) around the femoral neck, and the presence of intra-articular bodies (straight arrows). Note that thickening of the synovium (open arrows) has also occurred.
E. T2-weighted image of the same patient shows an extra-articular herniation sac (arrowheads) filled with intra-articular bodies (arrows).

Fig. 4
A 59-year-old man with idiopathic synovial osteochondromatosis of the left hip.
A. Anteoposterior radiograph of the left hip shows juxta-articular osteopenia and joint-space narrowing of the left hip joint (arrowhead).
B. T1-weighted coronal MR image of the same patient depicts an iso-intense intra-articular lesion (arrows).
C. T2-weighted image, obtained at the same level as in B, shows an intra-articular body of low signal intensity (curved arrow). Note that another intra-articular body has peripheral low signal intensity (arrowhead), and the central area has the signal characteristics of hyaline cartilage.
References
1. Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. J Bone Joint Surg Am. 1977. 59:792–801.
2. Kramer J, Recht M, Deely DM, et al. MR appearance of idiopathic synovial osteochondromatosis. J Comput Assist Tomogr. 1993. 17:772–776.
3. Llauger J, Palmer J, Roson N, Bague S, Camins A, Cremades R. Nonseptic monoarthritis: imaging features with clinical and histopathologic correlation. RadioGraphics. 2000. 20:S263–S278.
4. Norman A, Steiner GC. Bone erosion in synovial chondromatosis. Radiology. 1986. 161:749–752.
5. Crotty JM, Monu JUV, Pope TL. Synovial osteochondromatosis. Radiol Clin North Am. 1996. 34:327–342.
6. Tuckman G, Wirth CZ. Synovial osteochondromatosis of the shoulder: MR findings. J Comput Assist Tomogr. 1989. 13:360–361.
7. Blandino A, Salvi L, Chirico G, et al. Synovialosteochondromatosis of the ankle: MR findings. Clin Imaging. 1992. 16:34–36.
8. Vrdoljak J, Irha E. Synovial osteochondromatosis of the sternoclavicular joint. Pediatr Radiol. 2000. 30:181–183.
9. Burrafato V, Campanacci DA, Franchi A, Capanna R. Synovial chondromatosis in a lumbar apophyseal joint. Skeletal Radiol. 1988. 27:385–387.
10. Mubashir A, Bickerstaff D. Synovial osteochondromatosis of the cruciate ligament. Arthroscopy. 1998. 14:627–629.
11. Boles CA, Ward WG. Loose fragments and other debris, miscellaneous synovial and marrow disorders. Magn Reson Imaging Clin N Am. 2000. 8:371–390.
12. Peh WCG, Shek TWH, Davies AM, Wong JWK, Chien EP. Osteochondroma and secondary synovial osteochondromatosis. Skeletal Radiol. 1999. 28:169–174.
13. Freidman B, Nerubay J, Blankstein A, Kessker A, Horoszowski H. Synovial chondromatosis (osteochondromatosis) of the right hip: hidden radiologic manifestations (case report 439). Skeletal Radiol. 1987. 16:504–508.
14. Gilbert SR, Lachiewicz PF. Primary synovial osteochondromatosis of the hip: report of two cases with long-term follow-up after synovectomy and a review of the literature. Am J Orthop. 1997. 26:555–560.
15. Pai VR, van Holsbeeck M. Synovial osteochondromatosis of the hip: role of sonography. J Clin Ultrasound. 1995. 23:199–203.
16. Friedman B, Caspi I, Nerubay J, Huszar M, Ganel A, Horoszowski H. Synovial chondromatosis of the hip joint. Orthop Rev. 1988. 17:994–998.
17. Madewell JE, Sweet DE. Resnick D, editor. Tumors and tumor-like lesions in or about joints. Diagnosis of bone and joint disorders. 1998. 3rd ed. Philadelphia: WB Saunders;3956–3963.
18. Bredella MA, Tirman PF, Wischer TK, Belzer J, Taylor A, Genant HK. Reactive synovitis of the knee joint: MR imaging appearance, with arthroscopic correlation. Skeletal Radiol. 2000. 29:577–582.
19. Fernandez-Madrid F, Karvonen RL, Teitge RA, Miller PR, Negendank WG. MR features of osteoarthritis of the knee. Magn Reson Imaging. 1994. 12:703–709.
20. Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol. 1979. 10:439–451.
21. Sundaram M, McGuire MH, Fletcher J, Wolverson MK, Heiberg E, Shields JB. Magnetic resonance imaging of lesions of synovial origin. Skeletal Radiol. 1986. 15:110–116.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download