Abstract
Objective
To determine the incidence and etiologies of celiac axis stenosis in asymptomatic individuals.
Materials and Methods
This prospective study involved 400 consecutive patients (male: 319, female: 81) referred to us for celiac arteriography between April and July 1999. When celiac axis branches were opacified by collateral circulation during superior mesenteric arteriography, the presence of celiac axis stenosis was suspected; lateral projection celiac arteriography was performed and the pressure gradient was measured. The indicators used to determine whether or not celiac axis stenosis was significant were luminal narrowing of more than 50% and a resultant pressure gradient of at least 10 mmHg. Its etiology was determined on the basis of angiographic appearances and CT findings.
Results
Twenty-nine patients (7.3%) had celiac axis stenosis. The etiology of the condition was extrinsic compression due to the median arcuate ligament in 16 patients (55%) and atherosclerosis in three (10%), while in ten (35%) it was not determined. The incidence of celiac axis stenosis did not vary significantly according to sex, age and the presence of calcified aortic plaque representing atherosclerosis.
It is known that generalized atherosclerosis and other vascular diseases commonly involve the celiac axis (CA), and in certain clinical situations the recognition of abnormalities in this vessel is very important or critical. Where the management of hepatic tumors involves procedures such as chemoembolization and hepatic artery infusion chemotherapy, the first step in such a procedure is selective catheterization of the CA. If this is severely stenotic or occluded, particular skill is required to pass a catheter through it or along alternative collateral pathways without causing arterial injury, and the procedure may sometimes have to be abandoned (1). The right gastroepiploic artery has recently proven reliable for use in coronary artery bypass grafting, a procedure which depends for its success on evaluation of the hemodynamic and anatomic status of the CA (2): if graft ischemia is to be prevented, such evaluation in liver transplant recipients should be preoperative. Vascular compromise of the multiple splanchnic arteries, including severe CA stenosis, can cause abdominal angina, though this is not common (3-5).
Several studies have investigated the incidence and etiologies of CA stenosis. Derrick et al. (6) found that in 110 unselected autopsy cases, its incidence was 21%, while Bron and Redman (7) noted an incidence of 12.5% among 713 patients referred for abdominal aortography. They found that the most important etiology of CA stenosis was atherosclerosis. David and Harold (8) also reported the incidence and etiologies of CA stenosis, in particular in 50 asymptomatic individuals who underwent selective lateral aortography (8). In 12 (24%) of these, CA stenosis was 50% or more. In most cases in which the findings of lateral aortography were positive, the proximal CA showed a U-shaped configuration with compression along the superior aspect, a characteristic of impingement by the median arcuate ligament of the diaphragm (MAL) and/or the celiac plexus (8-10). Thus, most cases of CA stenosis in that series resulted from extrinsic compression due to MAL (8).
The incidence and etiologies of CA stenosis are still matters of some controversy, however. To our knowledge, hemodynamically significant CA stenosis has not been studied at all, and no study of CA stenosis has involved a Korean population. Measuring pressure and using pre/post-contrast CT and lateral projection angiography, we prospectively evaluated the incidence and etiologies of hemodynamically significant CA stenosis in asymptomatic individuals.
Between April and July 1999, we prospectively evaluated the incidence and etiologies of CA stenosis in 400 consecutive patients [M:F = 319:81; age, 17-85 (mean, 57) years] referred to us for chemoembolization of hepatic tumors (397 hepatocellular carcinomas and three cases of hepatic metastasis). For 139 patients it was the first session of chemoembolization, while the remaining 261 had undergone at least one such session. All were free from abdominal symptoms such as abdominal pain, change in bowel habitus and epigastric bruit.
All patients first underwent selective angiography of the CA and superior mesenteric artery (SMA) using a 6.5-F Rosch hepatic (RH) angiographic catheter (Cook, Bloomington, Ind., U.S.A.). Non-ionic contrast material [iopromide (ultravist); Schering, Berlin, Germany] was power injected using a mark-V plus device (Medrad, Pittsburgh, Pa., U.S.A.) at a rate of 6-7 mL/sec for 7 seconds during CA angiography and 4-6 mL/sec for 6 seconds during SMA angiography.
When SMA angiography revealed opacification of CA branches by collateral circulation, the presence of CA stenosis was suspected and lateral aortography or semi-selective CA angiography was performed on lateral projection, with the RH catheter located in front of the CA orifice. The pressure gradient between the abdominal aorta and CA was also measured. In patients who had previously undergone chemoembolization, the initial angiographic study was reviewed in order to exclude the possibility of iatrogenic CA stenosis associated with previous CA catheterization.
In all patients, contrast-enhanced CT as well as precontrast abdominal CT was performed using a HiSpeed Advantage scanner (GE Medical Systems, Milwaukee, Wis., U.S.A.) or a Somatom Plus-4 (Siemens Medical Systems, Erlangen, Germany) with a bolus injection of 120 ml of nonionic contrast material [iopromide (ultravist); Schering, Berlin, Germany] at a rate of 3 ml/sec. All scans were obtained through the abdomen in a craniocaudal direction with 7-mm collimation and 7-mm/sec table speed during a single breath-hold helical acquisition of 25-30 sec, and a 7-mm reconstruction interval.
CT and angiographic images were analyzed by three radiologists (CMP, JWC, and HBK) and decisions regarding the findings were reached by consensus. If SMA angiography suggested the presence of CA stenosis, the severity of collateral circulation from the SMA to the CA was determined. The use of lateral CA angiography or lateral aortography permitted analysis of the degree of CA stenosis and the morphology of the proximal CA. The former was recorded as a percentage, calculated by determining the ratio between the stenotic and normal distal CA lumen and multiplying by 100. CA stenosis was deemed significant if luminal narrowing of the CA orifice exceeded 50% and there was a resultant pressure gradient of 10 mmHg or more.
Etiology was determined according to the finding of lateral celiac arteriography and of CT. When the former showed superior notching and acute downward angulation of the proximal CA and the latter demonstrated CA compression by MAL, extrinsic compression by MAL was diagnosed. When lateral projection study indicated concentric luminal narrowing of the CA orifice and CT scanning revealed that this orifice was obstructed by atheromatous plaque, atherosclerosis was diagnosed. Under other circumstances, no conclusions as to the etiology of CA stenosis were reached.
Using the chi-square test, differences in the incidence and etiologies of CA stenosis according to age, sex and aortic calcification were analyzed. The total study population (n=400) was divided into two groups, younger and older, each consisting of 200 patients. The cut-off point was 68 years.
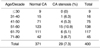
Tables 1 and 2 summarize the incidence and etiologies of significant CA stenosis according to age, sex, and the presence or absence of calcified aortic plaque.
SMA angiography visualized CA branches opacified by collateral circulation in 33 patients. In four of these, lateral celiac arteriography did not show significant luminal narrowing of the CA and pressure gradients were absent or less than 10 mmHg. The incidence of significant CA stenosis was 7.3% (29 of 400 patients). In all these cases, the angiographic configuration of collateral circulation from the SMA did not differ from that seen during the first session of SMA angiography, suggesting that in our study there was no iatrogenic CA stenosis associated with CA catheterization.
In nine of the 29 patients with CA stenosis (2.3% of the study population of 400), SMA angiography opacified all CA branches including the celiac trunk (Fig. 1A), indicating near-total or total hemodynamic occlusion of the CA orifice. In six of the nine, the angiographic catheter passed through the occluded segment and the pressure gradient was measured; thus, pressure gradients were determined in 26 of the total of 29 patients. The mean reading was 26.8 (range, 10-59) mmHg, with no significant difference between the near-totally or totally occluded group (28.1 mmHg) and the other celiac stenosis group (26.4 mmHg).
The age distribution of patients with CA stenosis [range, 36-79 (mean, 58) years] is shown in Table 1. In the younger group, the incidence of the condition was 8.5% (17 of 200 patients), while in the older group it was 6% (12 of 200). The difference was statistically insignificant (p > 0.05).
Among the 29 patients, the gender distribution of CA stenosis was M: F = 23:6. Its incidence was thus 7.2% in males and 7.4% in females, a difference that was also statistically insignificant (p > 0.05).
Calcified aortic plaque representing atherosclerosis was identified in 176 patients, 12 (6.8%) of whom had CA stenosis. Seventeen (7.6%) of 224 patients without such plaque had significant CA stenosis, and thus there was no statistically significant difference between the two groups (p > 0.05).
In 16 patients (4% of the study population), acute downward angulation with superior notching of the proximal CA was demonstrated by lateral CA angiography or lateral aortography, and this was a characteristic feature of extrinsic compression of the CA by MAL (Fig. 1B), a feature identified by CT in these 16 cases (Fig. 1C). The incidence of CA stenosis involving MAL was independent of age, sex, and the presence or absence of calcified aortic plaque (p > 0.05). Details are shown in Table 2.
In 12 patients with CA stenosis, the presence of calcified aortic plaque was demonstrated by CT, but in only three was calcified atheromatous plaque obstructing the CA orifice similarly revealed (Fig. 2C) and concentric luminal narrowing of the CA simultaneously demonstrated by angiography (Fig. 2B). In these three cases it was decided that atherosclerosis was the cause of CA stenosis.
In the remaining ten patients, typical radiologic findings that supported a specific etiology were not demonstrated. In five, mild cephalad indentation -which was not characteristic of extrinsic compression by MAL- was visible on lateral CA arteriographs but compression of the CA orifice by MAL was not identified by CT. In the other five patients, cephalad indentation was not revealed by lateral CA angiography and obstruction of the CA orifice by calcified aortic plaque was not demonstrated by CT.
In summary, the etiology of CA stenosis was extrinsic compression due to MAL in 16 patients (55%), atherosclerosis in three (10%), and undetermined in ten (35%).
The previously reported incidence of CA stenosis was higher than ours, ranging from 12.5 to 24% (6-8,11). Targeting western populations, those reports focused on luminal narrowing of the CA, as seen on lateral abdominal aortographs, as a diagnostic criterion of CA stenosis; the hemodynamic significance of CA stenosis was not proven, however, and miscellaneous cases of hemodynamically normal CA stenosis might therefore have been included. David and Harold (8), for example, reported that lateral aortography demonstrated CA stenosis in 12 of 50 asymptomatic individuals, but SMA angiography revealed this in only 3 of the 12 (6% of the population). As for the incidence of CA stenosis in which there was collateral circulation, the findings of David and Harold correlate with ours. Our study included only patients with hemodynamically significant CA stenosis in whom SMA angiography demonstrated collateral circulation and in whom anatomical CA stenosis and significant pressure gradient were also noted. It was thus found that 7.3% of the study population had significant CA stenosis, and that in 2.3% CA occlusion was near total or total. The lower incidence of CA stenosis in our study may be partly due to the lower incidence of atherosclerosis among the Korean population than in western countries. We found that the incidence of CA stenosis did not vary significantly according to sex and age, suggesting that atherosclerosis plays a minor role in CA stenosis in Korea.
Our study involved patients with hepatic tumors and a certain degree of liver cirrhosis. Some authors have insisted that in cases of arteriovenous fistula of the liver, primary hepatic tumor or liver cirrhosis, blood flow is diverted from the SMA and collateral circulation similar to that seen in moderate cases of CA stenosis is induced, and the degree of CA stenosis thus exaggerated (11). In our series, four patients in whom SMA angiography demonstrated the existence of collateral circulation had no significant CA stenosis. In these four, who also showed some degree of liver cirrhosis, a positive injection pressure and/or minimal luminal narrowing might have revealed collateral circulation. Because we used diagnostic criteria of collateral circulation, anatomical stenosis of more than 50% (as revealed by lateral CA angiography) and a significant pressure gradient, it was possible to eliminate these false-positive cases.
Most CA stenosis is induced by extrinsic compression by MAL or atherosclerosis, and in previously reported studies lateral aortography was used to investigate these etiologies. Our experience has shown that in a large proportion of patients it is difficult to classify the etiology of CA stenosis on the basis of lateral aortography alone. In our study, 48% of CA stenosis patients would not have been correctly evaluated etiologically if lateral aortography or lateral projection CA angiography alone had been used. In order to reveal direct evidence of extrinsic compression by MAL, and of atherosclerotic plaque and intimal calcification in atherosclerosis, we included CT findings in our diagnostic criteria.
In contrast to the general belief that atherosclerosis is the major cause of CA stenosis, this study revealed that in asymptomatic patients, extrinsic compression by MAL is the principal cause. This extrinsic compression is a kind of congenital abnormality and the onset of atherosclerosis is an age-dependent event. Thus, the proportion of the two etiologies in the group with CA stenosis varies according to the age and sex of the study population and the incidence of atherosclerosis in the general population. The low incidence of atherosclerotic CA stenosis we found can be explained by the low incidence of atherosclerosis in both the general Korean population and the asymptomatic study population.
In our study, CT scanning demonstrated calcified aortic plaque in 176 (44%) of 400 patients, twelve (6.8%) of whom had significant CA stenosis. Even among these twelve, the etiology of CA stenosis was extrinsic compression by MAL in six cases; in only three patients did pre/post-contrast CT scanning reveal definitive evidence of obstructing atheromatous plaque at the orifice of the CA. These results suggest that extrinsic compression by MAL is still the dominant etiology of significant CA stenosis in asymptomatic patients with atherosclerosis. The incidence of CA stenosis due to extrinsic compression by MAL is 4% of the general population (Table 2).
In three of the nine patients with hemodynamically total occlusion of the CA, in whom it was not possible to pass the RH catheter through the CA orifice and thus determine the etiologies of CA stenosis on the basis of the angiographic and CT findings, the orifice of the CA was anatomically near totally or totally occluded. In the remaining six, in whom the RH catheter could be passed through the CA orifice, however, the etiology of CA stenosis was found to be extrinsic compression by MAL, and stenosis of the CA orifice could be reversed by respiration.
Extrinsic compression of the CA by MAL has been evaluated by several authors (9, 10, 13) and lateral abdominal aortography has demonstrated acute downward angulation of the CA with cephalad notching of the proximal CA (7, 8, 10, 12); CA branches have been filled by retrograde collateral flow from vessels including the dorsal pancreatic and pancreaticoduodenal artery (1). Laparotomy has shown that the origin of the CA was abnormally high in relation to the aortic hiatus, and that the vessel was compressed by MAL (8).
In conclusion, the incidence of hemodynamically significant celiac stenosis in an asymptomatic Korean population was 7.3% and the most important etiology was extrinsic compression by MAL. Atherosclerosis was only a minor cause of celiac axis stenosis.
Figures and Tables
 | Fig. 1A 50-year-old man with hemodynamically total or near-total occlusion of the CA due to extrinsic compression by MAL.
A. Angiogram of the SMA reveals the celiac trunk and all CA branches including the common hepatic, splenic and left gastric artery (arrow) indicating hemodynamically total or near-total occlusion of the CA.
B. Angiogram of the lateral CA reveals acute downward angulation with superior notching of the proximal CA (arrow).
C. Enhanced abdominal CT scan reveals compression of the proximal CA by MAL (white arrows).
|
 | Fig. 2A 54-year-old man with significant CA stenosis due to atherosclerosis.
A. Angiogram of the SMA reveals the proper hepatic artery (arrow), seen through the pancreaticoduodenal arcade (small arrows).
B. CT scan indicates the presence of calcified atheromatous plaque (white arrow) obstructing the CA orifice.
C. Concentric luminal narrowing of the CA orifice (arrow) is demonstrated by lateral projection angiogram of the CA.
|
References
1. Soo CS, Chuang VP, Wallace S, et al. Treatment of hepatic neoplasm through extrahepatic collaterals. Radiology. 1983. 144:485–494.
2. Yasuura K, Takagi Y, Ohara Y, et al. Theoretical analysis of right gastroepiploic artery grafting to right coronary artery. Ann Thorac Surg. 2000. 69:728–731.
3. Lansing AM, McLarty TD. Mesenteric vascular insufficiency. CMAJ. 1962. 87:315–318.
4. Morris GC. Abdominal angina. Heart Bull. 1961. 10:5–7.
5. Berger RL, Byrne JJ. Intestinal gangrene associated with heart disease. Surg Gynecol Obstet. 1961. 112:529–533.
6. Derrick JR, Pollard HS, Moore RM. The pattern of arteriosclerotic narrowing of the celiac and superior mesenteric arteries. Ann Surg. 1959. 149:684–689.
7. Bron KM, Redman HC. Splanchnic artery stenosis and occlusion: Incidence, arteriographic and clinical manifestations. Radiology. 1969. 92:323–328.
8. David CL, Harold AB. High incidence of celiac axis narrowing in asymptomatic individuals. AJR. 1972. 116:426–429.
9. Dunbar JD, Molnar W, Beman FF, Marable SA. Compression of the celiac trunk and abdominal angina. AJR. 1965. 95:731–743.
10. Reuter S. Accentuation of celiac compression by the median arcuate ligament of the diaphragm during deep expiration. Radiology. 1971. 98:561.
11. Stewart RR, Oclin T. Stenosis of the celiac artery. Radiology. 1965. 85:616–627.
12. Cornell SH. Severe stenosis of the celiac artery: analysis of patients with and without symptoms. Radiology. 1971. 99:311–316.
13. Lindner HH, Kemprud E. A clinicoanatomic study of the arcuate ligament of the diaphragm. Arch Surg. 1971. 103:600–605.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download