Abstract
Objective
To evaluate the biodurability of the covering material in retrievable metallic stents covered with polycarbonate polyurethane.
Materials and Methods
Using a peristaltic pump at a constant rate of 1ml/min, bile was recirculated from a reservoir through a long tube containing four stents. Each of these was removed from the system every two weeks and a radial tensile strength test and scanning electron microscopy (SEM) were performed. Each stent, removed at 2, 4, 6 and 8 weeks, was compared with a control stent not exposed to bile juice.
Results
Gross examination showed that stents were intact at 2 weeks, but at 4, 6 and 8 weeks cracks were observed. The size of these increased gradually in accordance with the duration of exposure, and at 8 weeks several large holes in the polyurethane membrane were evident. With regard to radial tensile strength, extension and peak load at break were 84.47% and 10.030 N/mm, 54.90% and 6.769 N/mm, 16.55% and 2.452 N/mm, 11.21% and 1.373 N/mm at 0, 2, 4 and 6 weeks, respectively. Scanning electron microscopy at 2 weeks revealed intermittent pitting and cracking, and examination at 4, 6 and 8 weeks showed that the size of these defects was gradually increasing.
Metallic stent placement has been increasingly used for the palliation of obstructive jaundice due to malignant or benign disease. In a benign biliary stricture, long-term stent patency is the most important factor to be considered, as the patients have a long life expectancy(1). If metallic stents are placed in a patient with a benign biliary stricture, it is rather difficult to extract the stent transhepatically and, in addition, surgery is generally not feasible because of dense endoluminal or periductal fibrotic and adhesive changes (1, 2). According to previous reports, the main cause of recurrence is late stent occlusion due to tissue ingrowth (3, 4). In order to prevent late stent obstruction, covered self-expanding metallic stents have been designed. They not only have the potential to solve the problem of tissue ingrowth, but can also overcome the difficulties associated with the removal of a stent which is misplaced or becomes dysfunctional (5). We hypothesized that in a benign biliary stricture, removal of the covered stent when improvement was apparent would give good results and lead to improved long-term stent patency. To facilitate removal, the stent was covered with a polycarbonate polyurethane solution and a drawstring was positioned at its proximal end. We noticed that the biodurability of the covering material was a very important factor in retrieval. If the material is biodegraded, tissue will grow into the stent, making it difficult to remove.
The purpose of our study was to determine the biodurability of the covering material in retrievable metallic stents.
Stents used in our experiment were woven eight times from a single thread of 0.2-mm-diameter nitinol wire filament in a tubular configuration. The stent has eight points on the upper and lower end portions, the wire filament crossing spirally in an unengaged manner. One segment of the wire filament runs alternately on and under other segments, which are arranged in a direction opposite to that of the segment in such a way that a number of meshes are formed by the crossing points of the segments. To prevent tissue ingrowth through the stent wires, the stent was covered by dipping in a 12% polyurethane solution (Chronoflex; Cardiotech International, Woburn, Mass., U.S.A.). To provide a firmer covering on the ends of the stent, these were covered with 100% nylon mesh and then dipped in the polyurethane solution. To facilitate stent removable, a drawstring made of nylon monofilament was attached to its upper inner margin (Fig. 1).
The experimental perfusion system consisted of a bile reservoir, a long plastic tube including four stents, and a peristaltic pump (Fig. 2). The stents were placed in the tube using a 12-F home-made introducer set. Human bile was used for this study and 1,000 ml bile was replaced every day. Fresh bile was collected from one to three patients using T-tube or percutaneous transhepatic biliary drainage. Using a peristaltic pump, bile was circulated at a constant rate of 1ml/min.
The bile reservoir was cleansed using normal saline every two weeks. After 2, 4, 6 and 8 weeks, each stent was removed from the tube connected with the perfusion system using a home-made retrievable hook wire. A stent not exposed to bile (0-week stent) was used for control purposes. First, each stent was observed grossly, and patency and degree of cracking of the covering material was assessed. Second, a radial tensile strength test was performed using standard equipment and operating procedures. The test piece was 10 mm long and was threaded over a split pin assembly and loaded into the machine (Universal Testing Machine LRX, Lloyd Instruments, Ltd.). Jaw separation was 50mm/min, and extension and peak load at break were recorded. Third, a 5×5 mm section of each stent was cut, and this was coated with 200Å of platinium prior to scanning electron microscopy (SEM) (JEOL® JSM80A SEM, Tokyo, Japan). Magnification varied, but for objective comparison, each biliary stent was always observed at a constant magnification of ×1,600.
Insertion of the stents into the long tube was accomplished easily, and during the experimental period bile was circulated from the reservoir to the tube containing the stents at a constant rate of 1ml/min.
Gross examination showed that the stents were intact at 2 weeks, but showed cracks at 4, 6 and 8 weeks. These increased gradually according to the duration of exposure, and at 8 weeks several large holes were observed in the polyurethane membrane (Fig. 3).
With regard to radial tensile strengths, extension and peak load at break were 84.47% and 10.030 N/mm, 54.90% and 6.769 N/mm, 16.55% and 2.452 N/mm, 11.21% and 1.373N/mm at 0, 2, 4 and 6 weeks, respectively. Because of the large holes observed in the membrane at week 8, the radial tensile strength test was not performed at that time (Fig. 4).
Initial SEM of the stent showed no pitting or cracking, but SEM at two weeks revealed that these phenomena were already present and subsequent periodic examination showed that the size of the pits and cracks was gradually increasing. For comparison, a constant magnification of 1,600× was used (Fig. 5).
Iatrogenic injuries are the most common cause of benign biliary stricture (6, 7). Although the incidence of post-laparoscopic cholecystectomy stricture in experienced centers is less than 1%, there has nevertheless been a 5- to 10-fold increase in the incidence of strictures when compared with the open cholecystectomy era (8). In cases not involving surgery, the stricture may be secondary to inflammatory obstruction, gallstone erosion into the main bile duct, a pericholedochal abscess, external blunt trauma, or a complication of pancreatitis (9).
For benign biliary strictures, surgical repair is the treatment of choice. For the experienced surgeon, the 'first attempt' success rate is 78-88%; the procedures offering the greatest chance of success are choledoco- or hepaticojejunostomy with a Roux-en-Y jejunal loop (7). Balloon dilatation of biliary strictures represents a natural evolution of percutaneous transhepatic biliary drainage and has developed as a curative procedure when surgery fails to prevent obstructive jaundice caused by recurrent stenosis. Balloon dilatation, however, is usually not effective where benign biliary stricture is due to other causes, especially where chronic inflammatory processes such as pancreatitis and sclerosing cholangitis are involved (8). Rossi et al. reported that 70 of their patients with benign biliary strictures underwent percutaneous balloon dilatation and stenting (9). The reported patency rate in patients without sclerosing cholangitis was 96%, while for those with secondary sclerosing cholangitis, the rate was 33%. The average follow-up was 23 (range 3-72) months. Patients with anastomotic strictures (n=44), iatrogenic strictures (n=28), and strictures associated with sclerosing cholangitis (n=17) who had undergone percutaneous balloon dilatation showed patency rates after 36 months or more of 67%, 76% and 42%, respectively (10).
Many researchers have attempted the insertion of biliary endoprostheses, including expandable metallic stents, in patients with benign biliary stricture. Metallic stenting in 18 patients with post-surgical benign biliary strictures was performed by Maccioni et al., who reported that the overall patency rate after three-year follow up was 68.7% (1). They concluded that when surgical correction is no longer recommended, balloon dilatation and catheter stenting is the treatment of choice. The only indication for the use of metallic stents is failure to respond to percutaneous treatment, and in this group of patients, metallic stents have been the only remaining way of maintaining patency of the biliary tree without a permanent drainage catheter. Yoon et al. used metallic stents in the treatment of 23 patients with benign biliary strictures associated with recurrent pyogenic cholangitis (2). Primary stent patency rates for all patients at 6, 12, 24 and 36 months were 92%, 75%, 67% and 46%, respectively. They concluded that metallic stents in patients with biliary strictures associated with recurrent pyogenic cholangitis often have a high occlusion rate and that for long-term treatment, stents are not usually successful. Because of dense endoluminal or periductal fibrotic and adhesive changes, surgery is usually more difficult for patients who have undergone stent placement than for those who have not previously undergone this procedure, and in such cases, bypass rather than curative surgery is thus usually necessary. In patients with some probability of future curative surgery, metallic stenting is an option which must be carefully weighed, but if the metallic stents are retrievable, problems such as poor results of long-term patency and the difficulty of surgery after stent placement may be surmounted (2).
The ideal prosthesis must be completely biocompatible and stable within the biologic environment and must have a diameter similar to that of the stented segment, though small enough to be easily inserted. Self-expandable metallic stents best meet these requirements but are limited by the impossibility of removal should the stent be misplaced or become dysfunctional, and are subject to ingrowth of the tumor or reactive tissue from the stented wall. Many reports have suggested mucosal hyperplasia and inflammatory reactive change in the ductal wall as possible causes of late stent obstruction in patients with benign biliary strictures (1, 2), and in order to overcome these limitations, different synthetic plastic coverings have been proposed (5, 12). Polyurethanes, with their extensive structure/property diversity, are one of the most bio- and blood-compatible materials known today. These materials played a major role in the development of many medical devices ranging from catheters to total artificial heart, but are affected by certain in-vivo degradation mechanisms. Poly(ester)urethanes, for example, are subject to hydrolytic degradation and are no longer used in long-term implanted devices. While hydrolytically stable, they are subject to oxidative degradation in several forms, including environmental stress cracking and metal ion oxidation. In in-vitro qualification tests and in-vivo experiments, recently developed polycarbonate polyurethane was more biostable than poly(ether)urethanes (11).
Several researchers have investigated the biodurability of polycarbonate polyurethane, finding that due to the oxidative stability of the carbonate linkage, biodegradation in polycarbonate polyurethanes after 10 weeks of in-vivo treatment was less than in polyether polyurethanes (13). After an in-vivo study, Severini et al. described the biocompatibility, efficacy and stability of the metallic, self-expanding Gianturco-Rosch biliary Z-stent covered with polycarbonate polyurethane. Stents were implanted in the common bile duct of pigs, and after 1, 3 and 6 months, both their metallic structure and polymeric coating were intact (12).
We designed experiments to determine whether polycarbonate polyurethane is really bio-compatible or bio-stable in a biliary environment, and our findings differed from those of Severini et al. At 8 weeks there were several large holes in the polyurethane membrane, indicating that if a large rupture of the membrane occurred in a clinical situation, tissue ingrowth into the stent lumen would develop after 8 weeks. Radial tensile strength testing showed rapidly decreasing extension and peak load at break after the first two weeks, thus indicating that biodegradation of the polyurethane membrane began early after exposure to bile. In addition, SEM showed that the amount of pitting and cracking increased gradually with exposure to bile. Our experiments suffer from several limitations, however. First, an in-vitro model was used. Second, other factors affecting the biodegradation of polyurethane membrane, such as physical stress or infection, were not considered. Third, the point at which tissue ingrowth into the stent lumen occurred was not determined.
In conclusion, our experimental study showed that polycarbonate polyurethane membrane was not biostable in a biliary environment. We suggest two possible causes of biodegradation of the membrane. First, bile salts, with a pH of 7.8-8.6, are alkaline, and this may have led to changes in the chemical composition of the polycarbonate polyurethane membrane and its subsequent biodegradation. Second, bile salts in the intestinal tract act as emulsifiers or detergents, decreasing the surface tension of fat particles in the food and allowing the agitation in the intestinal tract to break the fat globules into minute particles. This emulsifying or detergent action of bile salts might have contributed to the biodegradation of the polycarbonate polyurethane membrane. It remains unclear, however, whether the experimental finding can be transferred to the clinical situation of benign biliary obstruction. To transfer these results clinically, more experimental and clinical studies must be performed.
Figures and Tables
 | Fig. 2Experimental settings of a perfusion system composed of a bile reservoir (1), long plastic tube (2) and peristaltic pump (3). |
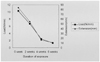 | Fig. 4Graph shows peak load and extension at break of covered material according to the duration of exposure to bile. |
 | Fig. 5SEM photomicrographs of polyurethane-covered, retrievable expandable metallic stent after exposure to bile (1,600×) (A: 0 week, B: 2 weeks, C: 4 weeks, D: 6 weeks, E: 8 weeks). Comparison between each specimen at constant magnification showed that the pits and cracks which developed became gradually larger in accordance with the duration of exposure. |
References
1. Maccioni F, Rossi M, Salvatori FM, et al. Metallic stents in benign biliary strictures: three -year follow-up. Cardiovasc Intervent Radiol. 1992. 15:360–366.
2. Yoon HK, Sung KB, Song HY, et al. Benign biliary strictures associated with recurrent pyogenic cholangitis. AJR. 1997. 169:1523–1527.
3. Alvarado R, Palmaz JC, Garcia OJ, Tio FO, Rees CR. Evaluation of polymer-coated balloon-expandable stents in bile ducts. Radiology. 1989. 170:975–978.
4. Coons HG. Self-expandible stainless steel biliary stents. Radiology. 1989. 170:979–982.
5. Tsang TK, Pollack J, Chodosh HB. Silicone-covered metal stents: an in-vitro evaluation for biofilm formation and patency. Dig Dis Sci. 1999. 44:1780–1785.
6. Citron SJ, Martin LG. Benign biliary stricures: treatment with percutaneous cholangioplasty. Radiology. 1991. 178:339–341.
7. Vos PM, VanBeek EJ, Smiths NJ, et al. Percutaneous balloon dilatation for benign hepaticojejunostomy strictures. Abdom Imaging. 2000. 25:134–138.
8. Gore RM, Levine MS. Textbook of gastrointestinal radiology. 2000. 2nd edition. Philadelphia: WB Saunders Company;1349.
9. Rossi P, Salvatori FM, Bezzi M, et al. Percutaneous management of benign biliary strictures with balloon dilation and self-expanding metallic stents. Cardiovasc Intervent Radiol. 1990. 134:231–239.
10. Mueller PR, VanSonnenberg E, Ferrucci JT Jr, et al. Biliary stricture dilatation: multicenter review of clinical management in 73 patients. Radiology. 1986. 160:17–22.
11. Edwards A, Carson RJ, Szycher M, Bowald S. In-vitro and in-vivo biodurability of a compliant microporous vascular graft. J Biomater Appl. 1998. 13:23–45.
12. Severini A, Mantero S, Tanzi MC, et al. In vivo study of polyurethane-coated Gianturco-Rosch biliary Z-stents. Cardiovasc Intervent Radiol. 1999. 22:510–514.
13. Mathur AB, Collier TO, Kao WJ, et al. In-vivo biocompatibility and biostability of modified polyurethanes. J Biomed Mater Res. 1997. 36:246–257.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download