Abstract
Phlegmonous enteritis is a rare infective inflammatory disease of the intestine, predominantly involving the submucosal layer. It is difficult to diagnose and often fatal. Its association with alcoholism and various liver diseases, although rarely reported, is well documented. We report a case of phlegmonous enteritis in a male patient with congestive heart failure and colon cancer, and describe the ultrasonographic and CT findings.
Phlegmonous gastritis and phlegmonous enterocolitis are rare types of gastrointestinal tract infection, and have been observed in association with alcoholism and hepatic cirrhosis (1-5). They may, however, also be found in healthy subjects (6). Although mucosal lesions can be present and inflammation may extend to the serosa, the constant feature of this disease entity is the intense purulent process that spreads throughout the submucosal layer (1-6).
Clinical diagnosis is difficult because the lesion is confined to the submucosa and easily misdiagnosed as submucosal edema or ischemic change. Thus, diagnosis has often relied on the presence of surgically resected or postmortem specimens (1-6). Except for one description of the CT findings of phlegmonous enteritis (6), the radiological imaging findings have not been reported in the literature.
We report a case of phlegmonous enteritis in a patient with congestive heart failure and colon cancer who underwent ultrasonographic and CT examinations followed by right hemicolectomy with distal ileal resection.
A 65-year-old man with intermittent, colicky periumbilical pain which first occurred two months earlier was admitted to hospital. He had an eight-year history of congestive heart failure caused by mitral valvular regurgitation and atrial fibrillation. He was nonalcoholic, and there was no history of diarrhea, hematochezia, or melena. Physical examination showed an increased bowel sound. Vital signs at admission were stable, and laboratory findings including white blood cell count, a liver function test and electrolytic balance were within the normal ranges. Electrocardiography revealed atrial fibrillation, and chest radiography demonstrated cardiomegaly (not shown). To exclude acute appendicitis, initial ultrasonography (US) was performed, and this demonstrated diffuse, segmental, concentric wall thickening of the terminal ileum just proximal to the ileocecal valve. The mucosal folds were blunted and there was low level echogenicity (Fig. 1A). Nonspecific ileitis, Crohn's disease, intestinal tuberculosis or ischemic enteritis were suggested as possible causes of the bowel wall thickening, and in order to evaluate the terminal ileum, colonoscopic examination was performed. The ascending colon was found to be completely obstructed by a circumferential mass lesion, and the colonoscopic fiber could not be advanced further. Subsequent CT scanning showed a markedly dilated small bowel and ascending colon, with concentric, hyperattenuating, focal wall thickening in the hepatic flexure of the ascending colon (Fig. 1B). In addition, the terminal ileum was dilated and showed diffuse, concentric wall thickening of its long segments with heterogeneous contrast enhancement. In the thickened wall, focal areas of poor contrast enhancement were also noted (Fig. 1C). There appeared to be several possible diagnoses, including ischemic enterocolitis caused by thromboembolism of mesenteric vessels arising from atrial fibrillation, inflammatory bowel disease involving the ascending colon and terminal ileum, and ischemic or infectious enteritis associated with colon cancer. Although surgery was recommended, the patient refused. Stool culture yielded lactose-fermenting Gram-negative bacillus, urine culture yielded Citrobacter freundii, and Gram staining of urine revealed the presence of Gram-negative rods; no organisms were isolated from blood cultures. In addition to conservative management of congestive heart failure, the patient underwent antibiotic therapy with amoxacillin, tobramycin or aztreonam for two weeks and ciprofloxacin for several days. Symptoms such as abdominal pain ameliorated, the level of bowel sound decreased, and laboratory findings continued to be within normal ranges. Vital signs were stable, except for intermittent fever of up to 38.2℃ until 30 days after admission. At this time, the patient complained of sudden abdominal pain and his clinical condition deteriorated. Emergency right hemicolectomy was performed, with resection of the distal ileum. At surgery, the hepatic flexure of the ascending colon was found to be completely obstructed by a hard concentric mass, and about 15 cm of the terminal ileum, just proximal to the ileocecal valve, was markedly dilated and diffusely thickened. About 500 ml of clear, yellowish ascites was also present. A cut section of the thickened terminal ileum revealed marked submucosal edema to a depth of approximately 10 mm, though there was no evidence of mucosal lesion. The colonic mass was confirmed microscopically as a poorly differentiated adenocarcinoma. Microscopic examination also showed that the mucosal folds of thickened ileal loop were blunted by submucosal edema and there was extensive inflammatory reaction, with infiltrations of neutrophils. In some areas of the thickened bowel wall, there was extensive destruction of underlying tissue by irregular-shaped abscesses. Neutrophil infiltration extended into the subjacent muscular layer and even to the serosa (Fig. 1D). The inflammatory reactions provided no evidence of granuloma formation, and the histologic findings were consistent with phlegmonous enteritis.
Phlegmonous enterocolitis is a rare inflammatory bowel disease with a high mortality rate of at least 60%. The literature in English has reported about 60 cases. The association between this disease entity and a variety of liver diseases has been well documented (1-3), though cases associated with lobar pneumonia, pharyngitis, infected peritoneojugular venous shunt and septicemia have been reported, and it has also occurred in healthy individuals (1, 4-6). Pathologically, it is defined as diffuse inflammation localized in the submucosa. Several kinds of pathognomic bacteria have been demonstrated in culture or histologically (1-6): Gram staining of intestinal lesions has revealed a variety of entities such as streptococci, Gram-positive cocci, and Gram-negative or -positive rods.
The mortality rate associated with this disease continues to be high due to delayed diagnosis (1-5). Thus, most cases reported in the literature were discovered at autopsy or after the examination of surgical specimens following surgery (1-6). Some reports have suggested that earlier diagnosis and surgical resection of diseased bowel, together with the use of broad- spectrum antibiotics, has led to a good outcome (1, 6).
The pathogenesis of this disease entity is not clear: Ito et al. (2) suggested a possible association with alcoholism. First, the direct toxic effect of alcohol may affect the gastrointestinal tract, and prolonged alcohol ingestion leading to changes in the intestinal mucosa, with increased intestinal permeability; subsequent penetration of the lamina propria by antigens (organisms) from the intestinal lumen results in a local antibody response. Second, in chronic alcoholism, the systemic and mucosal immune mechanisms are impaired, and this may exacerbate bacterial infection.
It is not known why the organisms involved in phlegmonous enteritis are confined to the submucosa. Bowel wall edema associated with portal hypertension has been described in liver cirrhosis, and the loose connective tissue in the submucosa can be excellent soil for the rapid and diffuse spread of the organisms involved in an episode of bacteremia (5).
Our case demonstrated certain features different from those of previously reported cases. First, the patient was not alcoholic and had no evidence of liver disease or septicemia. He had a long-standing heart problem, with obstructive colon cancer. Second, his clinical course was silent for a long period, being discovered only at surgery; previously reported cases, on the other hand, manifested an acute and serious clinical course, one which led even to sudden death. In our case, the early use of broad-spectrum antibiotics might have helped his condition to persist.
The literature in English includes only one case report dealing with the radiologic findings pertaining to this disease. Mooney et al. (6) reported the CT findings in one case, in which only nonspecific small bowel wall thickening with a small amount of ascites was noted. In our case, the terminal ileum showed marked wall thickening, and thumbprinting and blunted mucosal folds were revealed by ultrasonography. CT scanning demonstrated concentric thickening of the ileal wall, with heterogeneous contrast enhancement. The hypoattenuating focal areas in this thickened wall, shown at microscopic examination to be submucosal abscesses, are, in our case, thought to provide a clue to the diagnosis of phelgmonous enteritis. The investigation of further cases is, however, required.
Figures and Tables
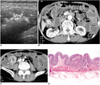 | Fig. 1A 65-year-old man with adenocarcinoma of the ascending colon and phlegmonous enteritis involving the terminal ileum.
A. Ultrasonogram shows marked, diffuse, segmental wall thickening of up to 10 mm in the terminal ileum. The mucosal folds are blunted (arrows).
B. Contrast-enhanced CT scan reveals colonic obstruction, with a well- enhanced concentric mass lesion visible in the hepatic flexure of the colon (arrows).
C. Contrast-enhanced CT scan at the lower level shows concentric thickening of the terminal ileum (arrowheads) along with diffuse dilatation of the ascending colon and small bowel loops. The thickened wall in the terminal ileum shows heterogeneous contrast enhancement and a small, poorly enhanced lesion (arrow).
D. Microscopic examination shows marked edematous thickening of the submucosa, with dense infiltrations of neutrophils and the formation of small irregular abscesses (arrows). The mucosa is intact, with extension of neutrophilic infiltration of submucosa into the muscular layer and serosa.
|
References
1. Miller AI, Smith B, Rogers AI. Phlegmonous gastritis. Gastroenterology. 1975. 68:231–238.
2. Ito M, Hashiguchi J, Fujimoto C, Sekine I, Tsuji K. Phlegmonous enteritis in alcoholic fatty liver. Am J Gastroenterol. 1991. 86(10):1535–1538.
3. Rosen Y, Won OH. Phlegmonous enterocolitis. Am J Dig Dis. 1978. 23:248–256.
4. Mendeloff J, Wenger J. Liver disease, phlegmonous colitis, and Gram-negative sepsis. South Med J. 1975. 68:507–510.
5. Blei ED, Abrahams C. Diffuse phlegmonous gastroenterocolitis in a patient with an infected peritoneojugular venous shunt. Gastroenterology. 1983. 84:636–639.
6. Mooney WW, Serpell JW, Scelwyn M. Phlegmonous enteritis: an unusual cause of abdominal pain. Australas Radiol. 1997. 41:173–175.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download