Abstract
Objective
To compare, in terms of their demonstration of tears of the anterior glenoid labrum, oblique axial MR arthrography obtained with the patient's shoulder in the abduction and external rotation (ABER) position, with conventional axial MR arthrography obtained with the patient's arm in the neutral position.
Materials and Methods
MR arthrography of the shoulder, including additional oblique axial sequences with the patient in the ABER position, was performed in 30 patients with a clinical history of recurrent anterior shoulder dislocation. The degree of anterior glenoid labral tear or defect was evaluated in both the conventional axial and the ABER position by two radiologists. Decisions were reached by consensus, and a three-point scale was used: grade 1=normal; grade 2=probable tear, diagnosed when subtle increased signal intensity in the labrum was apparent; grade 3=definite tear/defect, when a contrast material-filled gap between the labrum and the glenoid rim or deficient labrum was present. The scores for each imaging sequence were averaged and to compare conventional axial and ABER position scans, Student's t test was performed.
Results
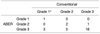
In 21 (70%) of 30 patients, the same degree of anterior instability was revealed by both imaging sequences. Eight (27%) had a lower grade in the axial position than in the ABER position, while one (3%) had a higher grade in the axial position. Three whose axial scan was grade 1 showed only equivocal evidence of tearing, but their ABER-position scan, in which a contrast material-filled gap between the labrum and the glenoid rim was present, was grade 3. The average grade was 2.5 (SD=0.73) for axial scans and 2.8 (SD=0.46) for the ABER position. The difference between axial and ABER-position scans was statistically significant (p<0.05).
Conclusion
MR arthrography with the patient's shoulder in the ABER position is more efficient than conventional axial scanning in revealing the degree of tear or defect of the anterior glenoid labrum. When equivocal features are seen at conventional axial MR arthrography, oblique axial imaging in the ABER position is helpful.
Partly because of the discrepancy in size between the large, round articulating surface of the humeral head and the small, shallow articulating surface of the glenoid fossa, the shoulder is intrinsically unstable. The reported incidence of shoulder dislocation is 1-2% (1), with dislocations in the anteroinferior direction accounting for about 95% of such occurrences (2). In young patients, dislocations may recur and cause major clinical disability. The diagnosis of anterior glenohumeral instability and anterior labral tears on the basis of acquired images may be particularly challenging.
There have been many attempts to accurately evaluate anterior glenoid labral tears (3-10). In contrast to the radiology literature, which has reported that they are accurately detected by MR imaging in over 90% of cases (3-7), the orthopedic literature has claimed that the accuracy of this same modality is between 59% and 75% (8-10). The role of MR imaging in the diagnosis of these tears has thus remained controversial. At first, the focus was on optimizing scanning protocols, and studies indicated that in depicting the labrum, multiplanar gradient-echo imaging provided better resolution than conventional spin-echo imaging (11). In a subsequent study by Chandnani et al. (3), MR arthrography was shown to be more accurate in evaluation of the glenoid labrum; they reported a sensitivity of 96% for this modality, compared with 93% and 73% for MR imaging and CT arthrography, respectively. Palmer et al. (12) later reported the sensitivity and specificity of MR arthrography as 91% and 93%, respectively. Studies have involved the use of both high-volume saline solution (13) and dilute gadolinium (3, 12).
To improve even further the accuracy of MR imaging in depicting the labrum and labral tears, reports have focused on the positioning of the shoulder and have suggested that abduction and external rotation (ABER) provide greater sensitivity than conventional basic scanning parameters with neutral shoulder positioning and nonrotation (14, 15). Tirman et al. (16) suggested that imaging of the shoulder in the ABER position was better for assessing suspected anterior labral tears.
In this study, we compared ABER MR arthrography with MR arthrography in the neutral non-rotated position in the evaluation of the antero-inferior glenoid labrum.
Thirty-five patients with a known history of recurrent anterior shoulder dislocation causing significant clinical disability underwent MR arthrography. Five were unwilling or unable to maintain the ABER position and so were excluded from the study. Of the 30 remaining, 25 were men and five were women, and their ages ranged from 15 to 31 (mean, 21.8) years. Eight patients received surgical treatment: five underwent arthroscopic examination and capsulorrhaphy, and in three, open Bankart repair was performed.
For MR arthrography, a 24-gauge spinal needle was inserted into the glenohumeral joint under fluoroscopic guidance, and a solution comprising 0.1 mL of gadopentate dimeglumine (Magnevist; Schering, Berlin, Germany) and 25 mL of saline was injected. The patient's arm and shoulder were moved through a full range of positions, and to ensure good joint distention with adequate gadolinium concentration, imaging was performed within one hour.
For this, a 1.5-T scanner (Magnetom Vision; Siemens, Erlangen, Germany) with a small flex coil was used, and fat-suppressed, T1-weighted axial, oblique coronal, and oblique sagittal images were obtained with the patient's shoulder in the neutral, non-rotated position ( TR/TE: 615-855/12-20 msec, 3 mm section thickness, 1 mm intersection gap, 256 × 192 matrix, 14-16cm field of view, two excitations). For the ABER position, patients were instructed to place the hand of the affected extremity posterior to the contralateral aspect of the head or neck with the elbow flexed (17). In this position, a T1-weighted coronal localizer sequence was performed prior to T1-weighted oblique axial imaging parallel to the shaft of the humerus.
The MR imaging findings were reviewed by two radiologists specialized in musculoskeletal radiology, who reached a consensus regarding each sequence. For each position, the degree of tear or defect of the anterior glenoid labrum (AGL) was recorded independently using a three-point scale: grade 1 for normal (when evidence of an AGL tear was equivocal); grade 2 for probable tear (diagnosed when subtle increased signal intensity of the labrum was observed, Fig. 1); and grade 3 for definite tear/defect (when a definite contrast material-filled gap between the labrum and the glenoid rim or deficient labrum was apparent, Fig. 2). Scores for each imaging sequence were added and averaged, and to compare the efficacy of axial and ABER imaging sequences, Student's t test was performed. Additionally, a record of any accompanying findings (Hill-Sachs defect, osseous Bankart lesions, SLAP lesions, for example) was kept, and clinical records were reviewed for surgical findings.
The sign of tearing of the anterior glenoid labrum, as revealed by MR arthrography, was the presence of a contrast material-filled gap between the labrum and the glenoid rim. The results are summarized in Table 1.
The average grade was 2.5 (SD=0.73) for axial images and 2.8 (SD=0.46) for ABER position images; Student's t test showed that the difference between the two modalities was statistically significant (p<0.05).
ABER positioning during MR arthrography aided in the visualization of AGL tears(Fig. 3, 4). Detachments of the anterior inferior glenoid labrum were usually visible on axial MR arthrograms, but were more clearly depicted when patients were in the ABER position. In all cases, ABER positioning during MR arthrography indicated that the taut inferior glenohumeral ligament (IGHL) exerted a tensile force on the anterior labral ligament complex.
Additional findings were as follows: compression fracture of the superolateral aspect of the humeral head (i.e. Hill-Sachs defect) was present in 25 cases; osseous Bankart lesion, seen as a fragment of labrum attached to the anterior band of the IGHL, in seven; superior labral anterior and posterior (SLAP) lesions in four; complete tear of the supraspinatus tendon in one.
Stability of the glenohumeral joint, the most common site of dislocation in the body, is maintained by various mechanisms. One is the anterior capsular mechanism, comprising the glenohumeral ligaments, anterior portion of the labrum, anterior joint capsule, scapular periosteum, synovial membrane and related recesses, subscapularis muscle and tendon, and bursa. Another is the posterior capsular mechanism, composed of the posterior labrum, posterior joint capsule, scapular periosteum, synovial membrane, recesses, and supraspinatus, infraspinatus, and teres minor muscles and tendons (14).
Conventional MR imaging, which allows direct visualization of major anatomic structures, has been traditionally used in the examination of patients with shoulder instability, though it has been pointed out that accurate interpretation of glenohumeral joint structures is beset with pitfalls (18). To improve the evaluation of smaller intra-articular structures such as the glenoid labrum and glenohumeral ligaments, several reports have suggested that the diagnostic accuracy of MRI is improved if the glenohumeral joint is distended with fluid prior to imaging (19-23).
In efforts to improve visualization of the glenoid labrum and the detection of tears in the AGL, MR imaging has been complemented by MR arthrography, traditionally performed with the shoulder in the neutral position and without rotation. Generally, this position has proven adequate in revealing these tears, though because the IGHL is relaxed and redundant, some tears may be anatomically closed and not visualized (15). In the ABER position, however, traction is placed on the inferior glenohumeral labral-ligamentous complex, and an occult labral tear may thus be demonstrated (14, 15). Most AGL injuries occur at the point of labral-ligamentous attachment to the glenoid rim and are due to injury to an abducted and externally rotated shoulder. Placing the shoulder in the ABER position stresses the inferior glenohumeral labral-ligamentous complex, with tension on the anterior band of the IGHL, and the visualization of small tears or detachments of the AGL after contrast material has extended into the tear or defect during MR arthrography is more likely.
Our findings are consistent with those of other researchers who have shown that MR arthrography of the shoulder in the ABER position allows better visualization of tears in the AGL (14, 15). In our study, however, we also determined the efficacy of ABER MR arthrography in revealing the degree of tear or defect of the AGL by grading the degree of tear. Our results indicate that this modality was indeed more efficient. Preliminary reports also suggest that the ABER position is valuable in the detection of partially healed labral tears, in which the surface of the tear becomes resynovialized even though the labral-ligamentous anchor remains competent. These tears may not be filled with contrast solution at neutral axial MR arthography, but because the labrum is more likely to become displaced from the glenoid rim, may be depicted on ABER images (15).
ABER imaging is subject to certain limitations. Approximately 20% of patients may be unwilling or unable to assume the ABER position because of shoulder pain or apprehension (15), circumstances which in our study led to the exclusion of five patients. Even experienced technicians require substantial extra time for positioning, as well as for coil placement and ABER image acquisition, and the ABER technique can thus be time consuming, adding at least ten minutes to the routine MR protocol.
The limitations of our study are the small number of cases and the fact that only eight patients underwent surgical intervention. We were therefore unable to compare the sensitivity, specificity and accuracy of axial and ABER MR arthrography. However, all 30 patients had a clinically documented history of recurrent anterior shoulder dislocation causing significant clinical disability, and in most, additional findings such as Hill-Sachs defect or osseous Bankart lesion were highly suggestive of prior dislocation. Our study could be criticized because our patient population was confined to those with anterior instability, shoulder pain thus being excluded as a selection criterion, and one reason for the lower prevalence of nondetached tears we report may be this selection basis.
In conclusion, when equivocal features such as subtle increased signal intensity in the labrum or no evidence of tear are seen on conventional axial MR arthrograms, in spite of definite clinical disability, an oblique axial imaging sequence should be performed with the patient's shoulder in the ABER position. Additional imaging sequences in this position may be especially helpful to radiologists who are not fully experienced in the interpretation of images of AGL tears. Furthermore, accurate evaluation of the degree of tear or defect of the AGL may help in the planning of surgical intervention in patients with anterior shoulder instability.
Figures and Tables
 | Fig. 1In a 20-year-old man with a history of recurrent anterior shoulder dislocation, a grade-2 anterior glenoid labral tear is revealed by both axial and abduction and external rotation images.
A. Axial fat-suppressed T1-weighted MR arthrogram reveals subtle increased signal intensity in the anterior glenoid labrum (arrow).
B. Abduction and external rotation oblique axial fat-suppressed T1-weighted MR arthrogram of this same region shows similar findings (arrow).
|
 | Fig. 2In a 24-year-old man with a history of recurrent anterior shoulder dislocation, a grade-3 anterior glenoid labral tear is seen on both axial and abduction and external rotation images.
A. Axial fat-suppressed T1-weighted MR arthrogram shows contrast material filling the tear (arrow) in the anterior glenoid labrum.
B. Abduction and external rotation oblique axial fat-suppressed T1-weighted MR arthrogram also reveals contrast material filling the gap between the anterior glenoid labrum and glenoid rim, showing a Bankart lesion (arrow).
|
 | Fig. 3In a 20-year-old man with a history of recurrent anterior shoulder dislocation, axial scanning demonstrates a grade-2 anterior glenoid labral tear. Abduction and external rotation scanning, however, indicates that this is grade 3.
A. Axial fat-suppressed T1-weighted MR arthrogram shows slightly increased signal intensity of the anterior glenoid labrum.
B. Abduction and external rotation oblique axial fat-suppressed T1-weighted MR arthrogram reveals a contrast material-filled gap between the labrum and the glenoid rim (arrow).
|
 | Fig. 4In a 19-year-old man with a history of recurrent anterior shoulder dislocation, axial scanning demonstrates a grade-1 anterior glenoid labral tear, but an abduction and external rotation-position scan indicates that this is grade 3.
A. On this axial fat-suppressed T1-weighted MR arthrogram, the presence of an anterior glenoid labrum tear is seen.
B. Abduction and external rotation oblique axial fat-suppressed T1-weighted MR arthrogram reveals detached labral tear with periosteal stripping (arrow).
|
References
1. Mohtadi NG. Advances in the understanding of anterior instability of the shoulder. Clin Sports Med. 1991. 10:863–870.
2. Chandnani VP, Gagliardi JA, Murnane TG, et al. Glenohumeral ligaments and shoulder capsular mechanism: evaluation with MR arthrography. Radiology. 1995. 196:27–32.
3. Chandnani VP, Yeager TD, DeBerardino T, et al. Glenoid labral tears: prospective evaluation with MR imaging, MR arthrography, and CT arthrography. AJR. 1993. 161:1229–1235.
4. Zlatkin MB, Iannotti JP, Esterhai JL, et al. Evaluation of rotator cuff disease and glenohumeral instability with MR imaging: correlation with arthroscopy and arthrotomy in a large population of patients (abstr.). Magn Reson Imaging. 1990. 8:S. 78.
5. Legan JM, Burkhard TK, Goff WB II, et al. Tears of the glenoid labrum: MR imaging of 88 arthroscopically confirmed cases. Radiology. 1991. 179:241–246.
6. Gusmer PB, Potter HG, Schatz JA, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology. 1996. 200:519–524.
7. Seeger LL, Gold RH, Bassett LW. Shoulder instability: evaluation with MR imaging. Radiology. 1988. 168:695–697.
8. Liu SH, Henry MH, Nuccion S, Shapiro MS, Dorey F. Diagnosis of glenoid labral tear: comparison between magnetic resonance imaging and clinical examinations. Am J Sports Med. 1996. 24:149–154.
9. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior instability. Am J Sports Med. 1994. 22:493–498.
10. Imhoff A, Hodler J. Arthroscopy and MRI of the shoulder: a comparative retrospective analysis. Z Orthrop Ihre Grenzgeb. 1992. 13:188–196.
11. McCauley TR, Pope CF, Jokl P. Normal and abnormal glenoid labrum: assessment with multiplanar gradient-echo imaging. Radiology. 1992. 183:35–37.
12. Palmer WE, Brown JH, Rosenthal DI. Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology. 1994. 190:645–651.
13. Willemsen UF, Wiedemann E, Brunner U, et al. Prospective evaluation of MR arthrography performed with high-volume intraarticular saline enhancement in patients with recurrent anterior dislocations of the shoulder. AJR. 1998. 170:79–84.
14. Kwak SM, Brown RR, Trudell D, Resnick D. Glenohumeral joint: comparison of shoulder positions at MR arthrography. Radiology. 1998. 208:375–380.
15. Cvitanic O, Tirman PFJ, Feller JF, Bost FW, Minter J, Carroll KW. Using abduction and external rotation of the shoulder to increase the sensitivity of MR arthrography in revealing tears of the anterior glenoid labrum. AJR. 1997. 169:837–844.
16. Tirman PFJ, Applegate GR, Flannigan BD, Stauffer AE, Crues JV III. Magnetic resonance arthrography of the shoulder. Magn Reson Imaging Clin N Am. 1993. 1:125–142.
17. Tirman PFJ, Bost FW, Steinbach LS, et al. MR arthrographic depiction of tears of the rotator cuff: benefit of abduction and external rotation of the arm. Radiology. 1994. 192:851–856.
18. Kaplan PA, Bryans KC, Davick JP, Otte M, Stinson WW, Dussault RG. MR imaging of the normal shoulder: variants and pitfalls. Radiology. 1992. 184:519–524.
19. Flannigan B, Kursunoglu-Brahme S, Snyder S, Karzel R, Del Pizzo W, Resnick D. MR arthrography of the shoulder: comparison with conventional MR imaging. AJR. 1990. 155:829–832.
20. Tirman RM, Janecki CJ, Eubanks RG, Nelson CL. Shoulder arthrography. Contemp Orthop. 1970. 1:26.
21. Tirman PFJ, Stauffer AE, Crues JV, Turner RM, Schobert WE, Nottage WM. Saline MR arthrography in the evaluation of glenohumeral instability. Arthroscopy. 1993. 9:141–146.
22. Palmer WE, Caslowitz PL, Chew FS. MR arthrography of the shoulder: normal intraarticular structures and common abnormalities. AJR. 1995. 164:141–146.
23. Palmer WE, Caslowitz PL. Anterior shoulder instability: diagnostic criteria determined from prospective analysis of 121 MR arthrograms. Radiology. 1995. 197:819–825.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download