Abstract
Shaken baby syndrome (SBS) is a form of child abuse that can cause significant head injuries, of which subdural hematoma (SDH) is the most common manifestation. We report the MRI findings of chronic SDH in three cases of SBS, involving two-, three- and eight-month-old babies. The SDH signal was mostly low on T1-weighted images and high on T2-weighted images, suggesting chronic SDH. In chronic SDH, a focal high signal on T1-weighted images was also noted, suggesting rebleeding. Contrast-enhanced MRI revealed diffuse dural enhancement.
In child abuse victims, head injury is a major cause of morbidity and mortality (1-3). Shaken baby syndrome (SBS) is a form of abuse that can cause severe head injuries such as subdural hematoma, subarachnoid hemorrhage, hemorrhagic contusion, and/or diffuse axonal injury (4, 5). SBS, the most common pattern of child abuse, has been a medical and social issue in many developed countries and has recently become an issue in Korea. Because the clinical history is in many instances insufficient and SBS frequently leaves no external evidence of physical injury, imaging such as CT or MRI is very important. We describe three cases of SBS presenting as chronic subdural hematoma.
A three month-old baby girl was admitted to the emergency department because of a seizure which occurred the previous day. There was no fever, and no definite history of trauma. She was a term baby with no perinatal problems such as birth trauma, and the findings of physical and laboratory examinations were unremarkable. Simple skull and chest radiographs revealed no abnormality. MRI performed on the day of admission showed left frontal subdural hematoma (SDH). The SDH signal was heterogeneous (high and low) on T1-and T2-weighted images, suggesting rebleeding in chronic SDH. Contrast-enhanced MRI revealed diffuse dural enhancement in the left hemisphere (Fig. 1), and fundoscopic examination demonstrated the presence of bilateral retinal hemorrhage. There was no definite history of child abuse.
An eight-month-old baby boy was admitted to the emergency department with a seizure which occurred 40 minutes earlier. For three days he had shown symptoms of upper respiratory infection, and had mild fever. There was no definite history of trauma. He was a term baby with no perinatal problems, and the results of physical and laboratory examinations were unremarkable. Simple skull and chest radiographs showed no abnormality. MRI performed the following day revealed bilateral fronto-temporo-parietal SDH. This showed a mainly low signal on T1-weighted images and a high signal on T2-weighted images. On the right side, the hematoma showed a high focal signal on T1-weighted images, suggesting rebleeding. Contrast-enhanced MRI revealed the dura mater as faintly enhanced (Fig. 2), and fundoscopic examination performed the following day indicated bilateral retinal hemorrhage. There was no definite history of child abuse. On hospital day 22, subdural catheter drainage was performed and about 400cc of chronic hematoma was evacuated.
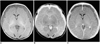
A two-month old baby girl was admitted to the emergency department on account of a seizure 16 hours earlier, and for three days she had had a fever. She was a term baby with no perinatal problems, and the findings of physical and laboratory examinations were unremarkable. Simple skull and chest radiographs indicated no abnormality. MRI performed on the day of admission showed SDH in both cerebral hemispheres and the posterior fossa. The hematoma showed a low signal on T1-weighted images and a high signal on T2-weighted images. A bilateral focal high signal was also noted on both T1- and T2-weighted images of occipital areas, suggesting rebleeding or hemorrhage of a different stage, and in addition, diffuse dural thickening and enhancement were observed (Fig. 3). Subdural catheter drainage was undertaken the following day, and chronic hematoma was evacuated. Fundoscopic examination was not performed. A meticulous interview with a social worker revealed that the child had been abused.
SBS was first described by Caffey in 1972 as whiplash baby syndrome, and acceleration-deceleration stress is known to be the cause of the injury (1). Approximately two-thirds of shaken babies suffer permanent brain damage or die (6). Violent shaking can produce significant damage, especially to the brain or head and neck; this includes intracranial hemorrhage, retinal hemorrhage, and hemorrhage in the high cervical cord (4, 5). Because their neck muscles are not strong enough to support their relatively large head compared with adults, and because their brains are not completely myelinated, infants are very susceptible to shaking (7).
SDH is the most common manifestation of head injury in SBS, and since SDH, especially chronic SDH, is a very rare cause of accidental injury among infants (3, 8, 9), radiologists should suggest the possibility of SBS and child abuse. In young babies, whose CSF space is larger than in adults, bridging veins can easily be torn during shaking (1). If repeated shaking leads to injury, SDH can be chronic and hemorrhage may occurr during both the acute and chronic stages, as in our cases (9). The presence of SDH of different ages is indicative of injuries from repeated abuse (2). Differentiation between acute and chronic SDH on the sole basis of a T1 or T2 signal can be difficult, and-as in our cases-dural enhancement observed at contrast-enhanced MRI and probably due to a granulation tissue membrane can be a helpful finding for diagnosing chronic SDH (9). Other manifestations, such as subarachnoid hemorrhage, cerebral contusion and diffuse axonal injury can also occur in SBS, but only SDH was noted in our three cases. Except for subarachnoid hemorrhage, MRI is superior to CT in diagnosing these head injuries (9).
Retinal hemorrhage is one of the characteristic signs of SBS and is known to result from an abrupt rise in intracranial pressure during shaking (7). Birth trauma can cause retinal hemorrhage, though this resolves quickly (10). Subacute bacterial endocarditis, anemia or thrombocytopenia can also lead to retinal hemorrhage, but these can be ruled out by clinical findings such as the results of laboratory tests (10). Bilateral retinal hemorrhage was found in two of three cases in this report; in neither was there a history of birth trauma, and nor were the laboratory findings remarkable. Conditions which can cause retinal hemorrhage, such as subacute bacterial endocarditis, anemia or thrombocytopenia, were ruled out by the clinical and laboratory findings in all our three cases. Many reports have indicated that in the absence of any disease process, retinal hemorrhage is indicative of SBS (1). In case three, fundoscopic examination was not performed, but a history of child abuse was revealed by the interview with the social worker; adequate counseling of the patient and her family was thus possible. In none of the three cases was there a history of trauma and the infants' parents or carers did not admit to any physical insults to the patients. Many people do not know, however, that shaking a baby can cause severe injury, and thus fail to mention it during history taking; in many instances, unless there is external evidence of injury, a diagnosis of SBS may therefore be delayed or even impossible. In detecting abnormal injuries and suggesting to the clinician the possibility of SBS, the radiologist's role is thus very important and he or she can help prevent further damage due to repeated shaking.
In summary, we have described three cases of SBS shown by MRI to be chronic SDH. When radiologists interprete the images in cases involving head injuries to young basies, they should bear in mind the possibility of SBS, and by suggesting to the clinician that a particular case may involve this and child abuse, may be able to prevent further harm to a patient.
Figures and Tables
Fig. 1
Chronic subdural hematoma (SDH) in a three-month-old female patient.
A. T1-weighted image shows mainly low-signal SDH, with a high signal focus in the left frontal area.
B. On a T2-weighted image the signal intensity of the chronic SDH is mainly high, with a focal area of low intensity.
C. Contrast-enhanced T1-weighted image shows overlying linear dural enhancement.
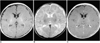
Fig. 2
Chronic SDH in an eight-month-old male patient.
A. T1-weighted image shows low-signal SDH in both frontal areas.
A high signal area, suggesting subacute hemorrhage, may also be observed in the right frontal area (arrow).
B. On a T2-weighed image, the signal intensity of the SDH is mainly high, though there is a focal area of low intensity (arrow).
C. Contrast-enhanced T1-weighted image shows diffuse linear dural enhancement.
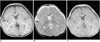
Fig. 3
Chronic SDH in a two-month-old female patient.
A. T1-weighted image shows low (though higher than CSF)-signal SDH in both cerebral hemispheres and the posterior fossa. In addition, a high signal area, suggesting subacute hemorrhage, can be seen in the occipital areas (arrows).
B. T2-weighted image reveals high signal intensity SDHs in both frontoparietal and occipital areas (arrows).
C. Contrast-enhanced T1-weighted image demonstrates diffuse linear dural enhancement.
References
1. Cox LA. The shaken baby syndrome: diagnosis using CT and MRI. Radiol Technol. 1996. 67:513–520.
2. Petitti N, Williams DW III. CT and MR imaging of nonaccidental pediatric head trauma. Acad Radiol. 1998. 5:215–223.
3. Sato Y, Yuh WTC, Smith WL, Alexander RC, Kao SCS, Ellerbroek CJ. Head injury in child abuse: evaluation with MR imaging. Radiology. 1989. 173:653–657.
4. Duheime AC, Gennarelli TA, Tiubault LE, Bruce DA, Margulies SS, Wiser R. The shaken baby syndrome: A clinical, pathological and biochemical study. J Neurosurg. 1987. 66:409–415.
5. Hearley MN, Sonntag VKH, Rekate HL, Murphy A. The infant whiplash-shake injury syndrome: a clinical and pathologic study. Neurosurgery. 1989. 24:536–540.
6. Couser S. Shaken baby syndrome. J Pediatr Health Care. 1993. 7:238–239.
7. Brown GR, Runyan DK. Diagnosing child maltreatment. N C Med J. 1994. 55:404–408.
8. Kleinman PK. Diagnostic imaging in infant abuse. AJR. 1990. 155:703–712.
9. Osborn AG. Diagnostic neuroradiology. 1994. St. Louis: Mosby;205–212.
10. Budenz DL, Farber MG, Mirchandani HG, Park H, Rorke LB. Ocular and optic nerve hemorrhages in abused infants with intracranial injuries. Ophthalmology. 1994. 101:559–565.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download