This article has been
cited by other articles in ScienceCentral.
Abstract
Inflammatory breast disorders include a wide array of underlying causes, ranging from common benign infection, non-infectious inflammation and inflammation resulting from underlying breast malignancy. Because it is at times difficult to distinguish mastitis and breast cancer based on clinical features, awareness of detailed imaging features may be helpful for better management of inflammatory breast disorders. Therefore, this pictorial essay intends to demonstrate radiologic findings of a variety of inflammatory breast disorders, using selected cases with mammography, ultrasound and magnetic resonance images.
Go to :

Keywords: Breast, Inflammation, Cancer, Ultrasound, Mammography, Magnetic resonance imaging
INTRODUCTION
Mastitis refers to inflammation of the breast parenchyma, often presenting with pain, heat and redness that may be a debilitating illness with prolonged morbidity (
1). It may also present with a wide array of other nonspecific symptoms, that may lead to delayed diagnosis and inappropriate treatment (
2). Broadly, inflammatory disorders of the breast can be divided into three categories: infectious mastitis, non-infectious mastitis and mastitis related to underlying malignancy (
13). Clinical and radiological features of benign mastitis commonly overlap with breast malignancies, further adding to the diagnostic dilemma. Failure to respond to antibiotic therapy is usually an indication for a biopsy to rule out underlying malignancy (
134). This pictorial essay illustrates a variety of common and uncommon inflammatory breast conditions encountered at a busy breast imaging center.
Go to :

Radiological Signs of Breast Inflammation
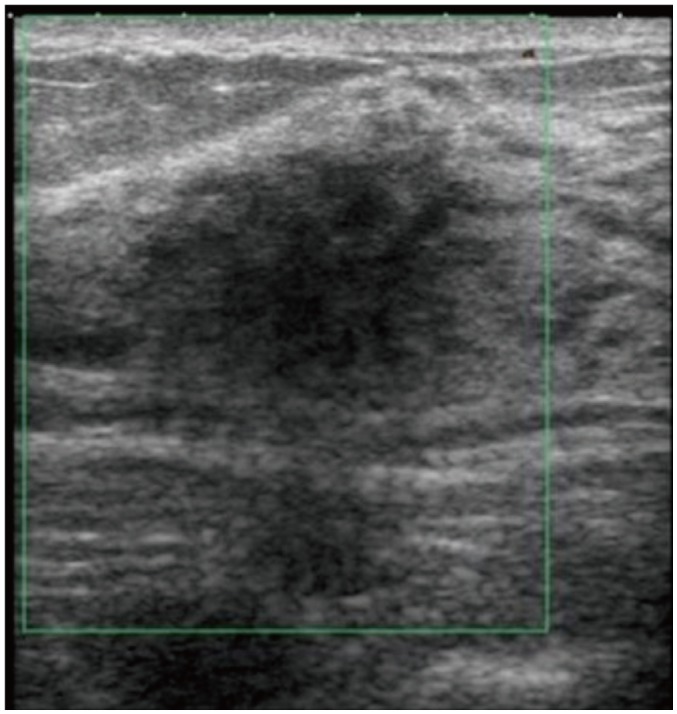
The breast is a superficial organ and often inflammation would involve the overlying skin. Features of cellulitis such as skin thickening and subcutaneous edema should be noted. Radiological imaging is more advantageous than clinical examination in evaluating skin thickening as it allows accurate delineation of its extent, measurement and comparison to surrounding skin and contralateral breast (
1). Subcutaneous edema is easily evaluated using Doppler US, revealing diffuse increase in thickening and echogenicity of the subcutaneous tissue and later accumulation of fluid in the subcutaneous tissue (
Fig. 1A). On mammogram, subcutaneous edema manifests as diffuse increase in breast density or increased interstitial markings (
5).
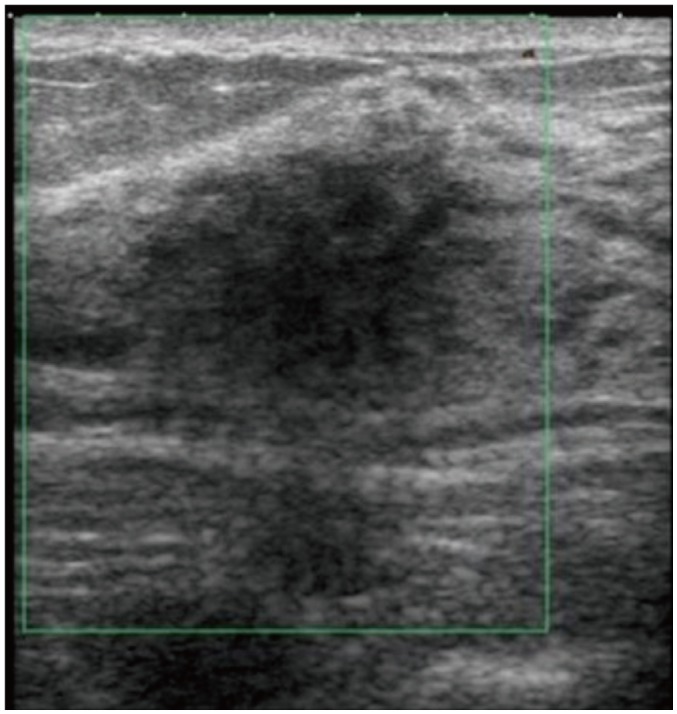
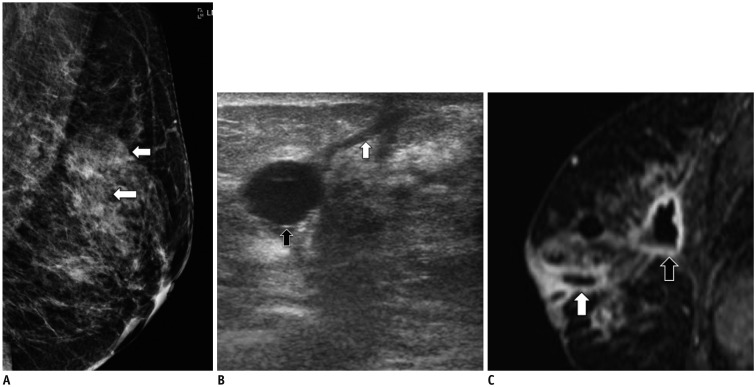
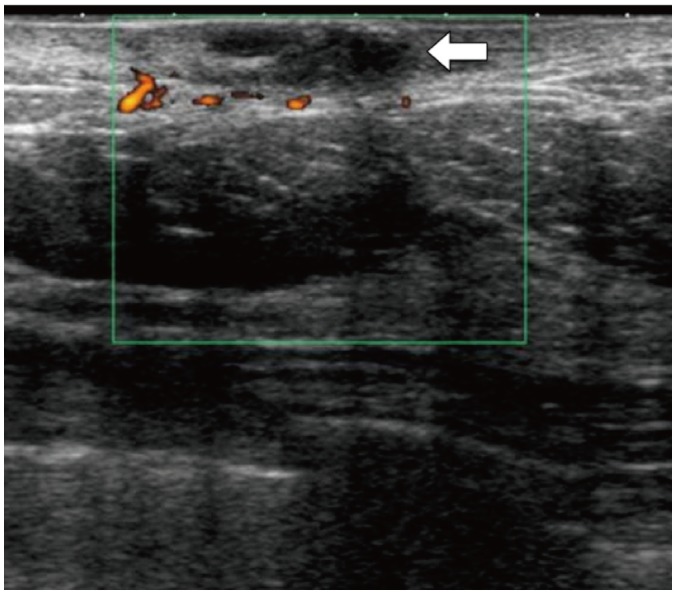
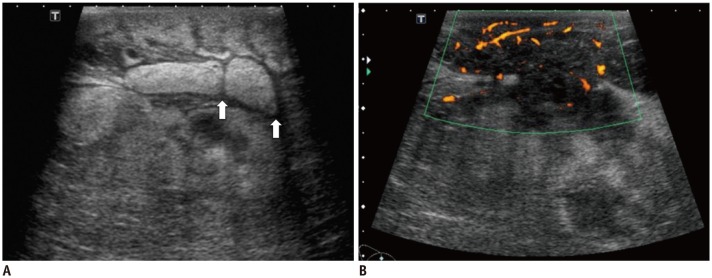 | Fig. 1
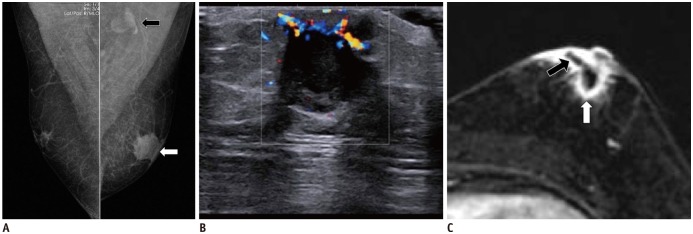
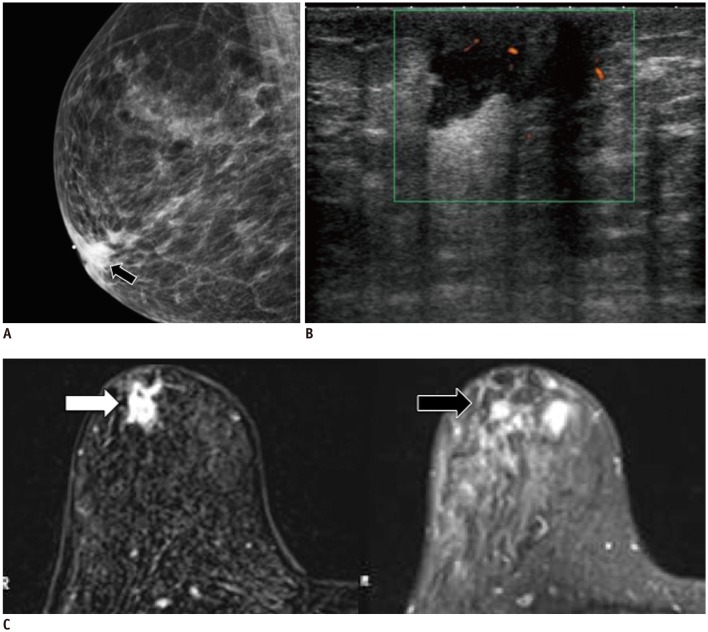
Pueperal Mastitis in 29-year-old female.
A. Ultrasound reveals features of subcutaneous edema with skin thickening with increase in echogenicity of subcutaneous tissue. Fluid is observed as intervening hypoechoic lines (white arrows) in subcutaneous tissue. B. Ultrasound with color Doppler also reveals ill-defined hypoechoic fluid collection with heterogeneous content within site of inflammation. Hyperemia of subcutaneous tissue surrounding collection is noted.

|
Hyperemia (increased vascularity) of the breast tissue is another sign of inflammation. This can be evaluated using Doppler US, revealing increased arterial and venous structures (
1) (
Fig. 1B). Lactiferous duct abnormalities such as duct dilatation, thickened walls and presence of contents within the ducts should be investigated as some inflammatory conditions are related to lactiferous duct involvement. One should also notice possible fluid collections within the site of inflammation. These commonly demonstrate hypoechoic and heterogeneous content and may show irregularly thickened walls. Collections may fistulate into the skin or intra-mammary ducts (
1).
Breast inflammation may involve the axillary lymph nodes and cause reactive enlargement. Differentiating benign reactive lymphadenopathy from malignant lymphadenopathy based on imaging features alone can be challenging. Benign reactive lymph nodes generally demonstrate smooth thickening of the cortices with preservation of normal fatty hilum (
Fig. 2A). In contrast, tumor involved lymph nodes tend to demonstrate irregular cortical thickening with loss or replacement of the fatty hilum (
13) (
Fig. 2B).
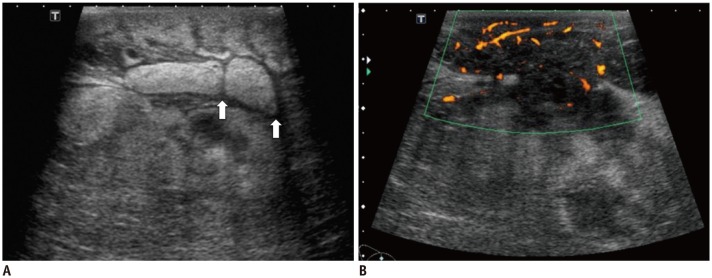
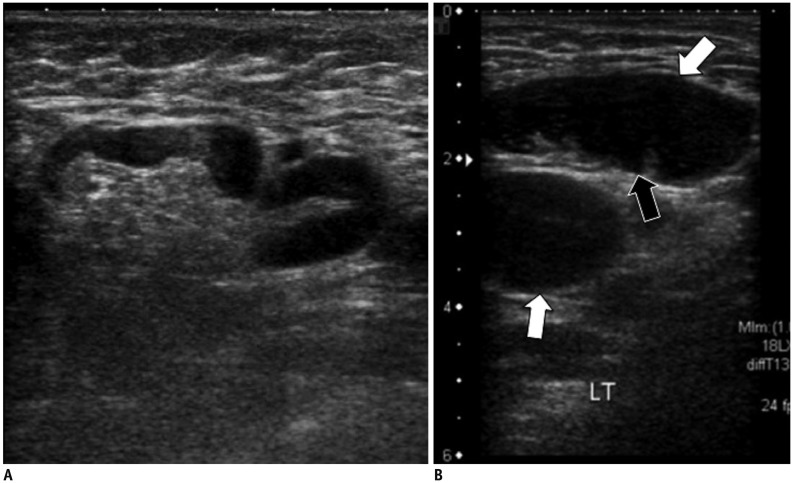 | Fig. 2
Reactive versus malignant lymphadenopathy.
A. Ultrasound of right axilla in 33-year-old female with large right breast abscess reveals enlarged lymph node with smooth thickening of cortex. Normal fatty hilum and reniform configuration is preserved. These are features of benign reactive lymph node. B. Ultrasound of right axilla in 52-year-old female, with painful right breast mass and palpable right axillary nodes. Lymph nodes reveal bulky cortex (white arrows) and loss of normal fatty hilum (black arrow), features that are more worrisome for malignant involvement. Ultrasound-guided biopsy of node was conducted and diagnosis of lymphoma was made.

|
Go to :

Infectious Mastitis
Acute Puerperal Mastitis
Mastitis that occurs during lactation is termed puerperal mastitis. This is the most common form of mastitis and usually occurs from infection with Staphylococcus aureus or Streptococcus bacteria. This may lead to reduced milk production and is a common reason for mothers to stop breast feeding (
6). Infection often arises from disruption to the skin surface of the nipple areolar complex and milk stasis is a risk factor for infection (
7). Most patients will respond to antibiotic treatment, but a small percentage may develop abscess collections, that may complicate treatment and require further drainage. Ultrasound is useful for detecting these collections (
Fig. 1B). Although rare, one should always keep in mind the possibility of cancer in puerperal mastitis that does not respond to antibiotic therapy, in which case histological sampling should be conducted (
138).
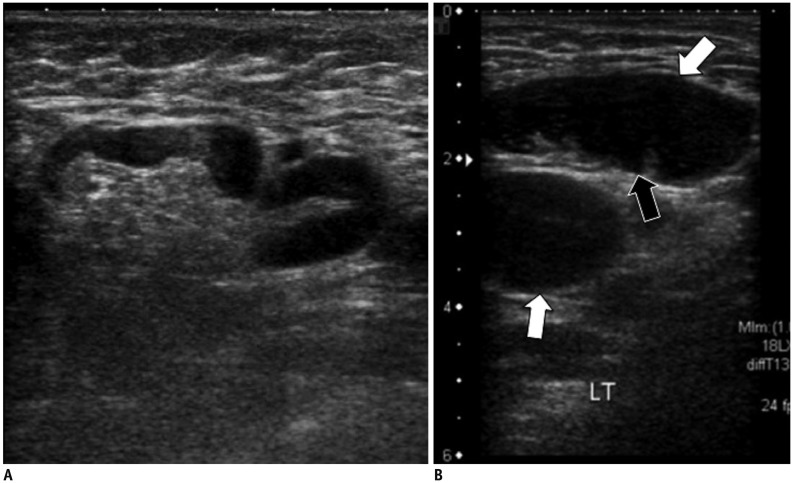
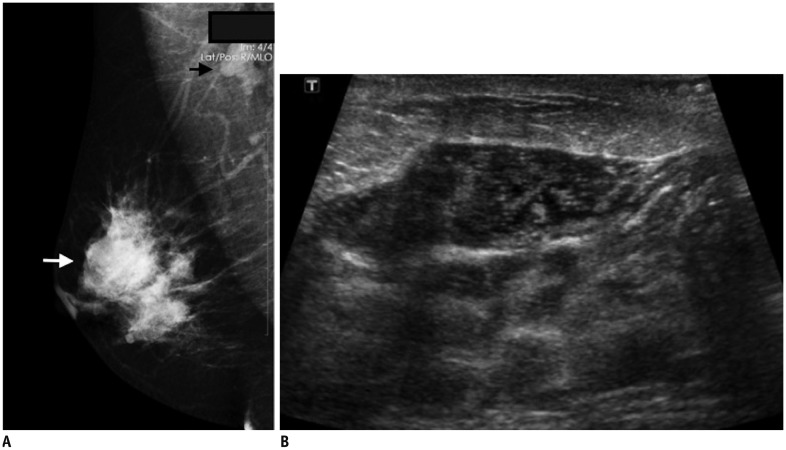
Infected Galactocele
Galactoceles are the most common lesions in lactating women. Milk is retained and stagnant when breast-feeding is stopped, causing ductal dilatation and development of cysts or galactoceles. Infection is a relative common complication of galactoceles (
8). Galactoceles will appear similar to abscesses but follow a ductal distribution (
3). Diagnosis is made based on an appropriate clinical picture (i.e., history of recent lactation) and aspiration of mixed milky and purulent material from the cyst (
8) (
Fig. 3).
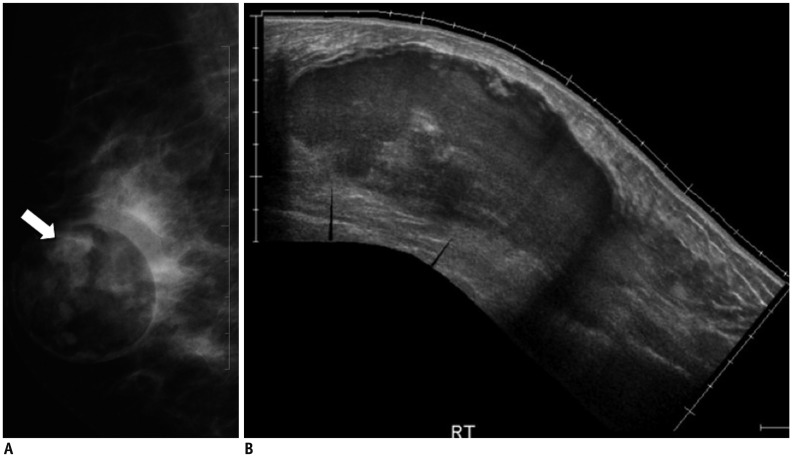 | Fig. 3
Infected galactocele in 32-year-old lactating female presenting with right breast swelling and pain.
A. Mammogram of right breast in mediolateral oblique projection shows well-defined predominantly lucent mass with some opaque material within (white arrow). This appearance is in keeping with presence of both lucent fat and dense proteinaceous content (milk and inflammatory cells). B. Ultrasound demonstrates large collection in right breast with heterogeneous cystic-solid content. This lesion was aspirated which yielded milk content and inflammatory cells. No malignant cell was observed. Subsequent follow-up ultrasound examinations reveal gradual resolution of this lesion.

|
Non-Puerperal Subareolar Mastitis
Non-puerperal subareolar mastitis and breast abscess, also known as Zuska's disease is an uncommon and recurring disease strongly linked to cigarette smoking (
29) (
Fig. 4). It frequently affects middle-age females in their 40s but may affect a wide range of ages (mid-teens-80s) and may even be observed in males (
2) (
Fig. 5). This is caused by squamous metaplasia and proliferation of the epithelium in the lactiferious ducts, causing obstruction and secretory stasis leading to abscess formation. They present as recurring abscesses, often with fistulous tracks extending to the skin near the periareolar region (
1210). Initial infections are usually caused by Staphylococcus bacteria. Subsequent recurring episodes of infection may be caused by mixed flora of bacteria, including anaerobes, and can be more complicated to treat with higher rates of recurrence. Radiological features of subareolar mastitis and inflammatory breast carcinoma may be similar (
2). If clinically suspected, biopsy should be conducted to exclude presence of malignancy.
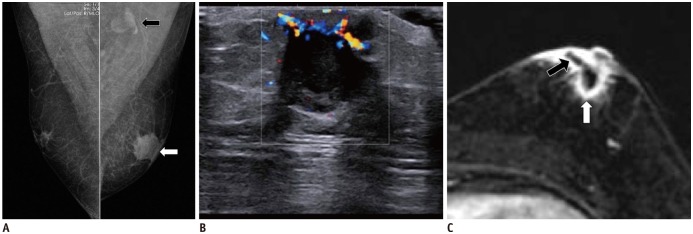
 | Fig. 4
Non-pueperal subareolar abscess in 49-year-old female with history of smoking.
This patient presented with palpable retroareolar lump in right breast.
A. Mammogram of right breast in mediolateral oblique projections reveals retro-areolar opacity (black arrow). B. Ultrasound reveals retro-areolar collection with increased peripheral vascularity in right breast. C. T2 weighted and post-contrast T1-weighted MR imaging shows cystic lesion in subareolar region of right breast on T2-weighted image (white arrow). This also demonstrates rim enhancement on post-contrast T1-weighted image (black arrow). Repeat ultrasound study conducted three months later reveals slightly smaller but persistent subareolar collection. This lesion was biopsied and inflammatory cells were seen. No malignant cells were obtained.

|
 | Fig. 5
Subaerolar abscess in 49-year-old male, presenting with left breast pain and swelling.
A. Mammogram of both breasts in mediolateral oblique projections demonstrates left breast retro-areolar opacity (white arrow). Prominent left axillary node is also seen (black arrow). B. Ultrasound of left breast with color Doppler reveals hypoechoic collection in left subareolar region with echogenic internal debris and increased peripheral vascularity. Ultrasound guided tru-cut biopsy of this lesion was conducted which yielded inflammatory cells. No malignant cells were observed. C. Post contrast T1 weighted fat saturated MR imaging of both breasts in axial plane reveals subareolar rim-enhancing collection in left breast (white arrow). Fistulous tract extending to skin surface was also noted (black arrow).

|
Peripheral Non-Puerperal Breast Abscesses
Peripheral breast abscesses usually occur in older women. In some cases, it may occur in patients with pre-existing conditions such as diabetes and rheumatoid arthritis. Staphylococcus aureus is the most common pathogen. These abscesses typically respond well to antibiotic treatment and drainage, and they tend not to recur (
10).
Peripheral breast abscesses may also occur in patients with pre-existing cystic breast conditions, with superimposed infection of breast cyst (
1). Patients may present with a painful palpable lump in the breast. Typical features of a infected breast cysts include thickening of the cyst wall, increased peripheral vascularity and presence of echogenic debris within the cyst (
13) (
Fig. 6).
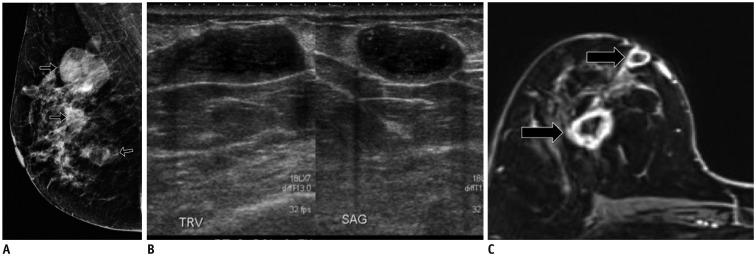
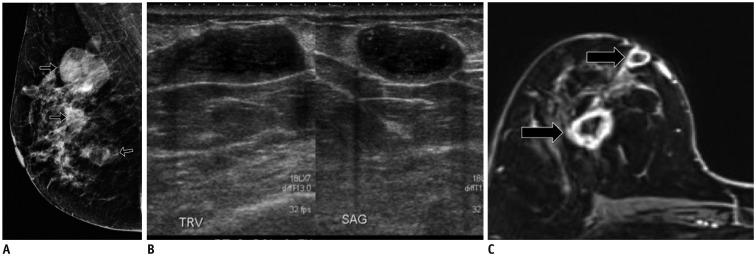 | Fig. 6
Peripheral breast abscesses from infected cysts in 38-year-old non-lactating female, presenting with painful lumps in right breast.
A. Mammogram of right breast reveals several partial circumscribed masses (black arrows), predominantly in upper half of right breast. B. Ultrasound of right breast reveals cysts with thickened walls and internal echogenic material. C. T1-weighted post contrast fat saturated MR imaging of breasts reveal presence of several cysts in upper half of right breast with thickened enhancing walls (black arrows). SAG = sagittal, TRV = transverse

|
Post-Procedural Infections
Infections following invasive procedures such as breast surgery or biopsy are a relatively common cause of breast infection. Diagnosis is usually straightforward with the appropriate clinical history (
1) (
Fig. 7).
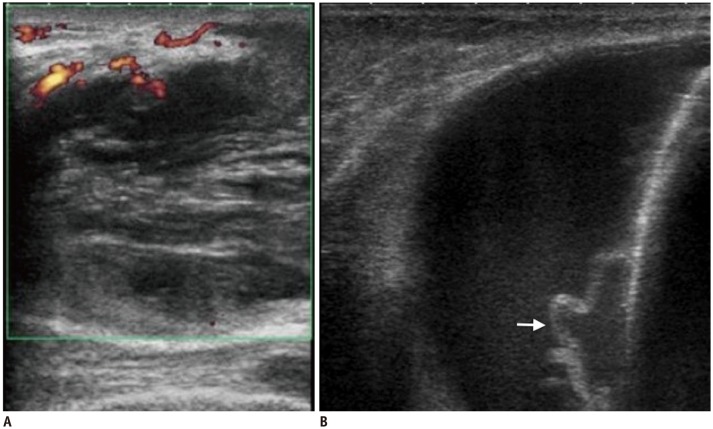
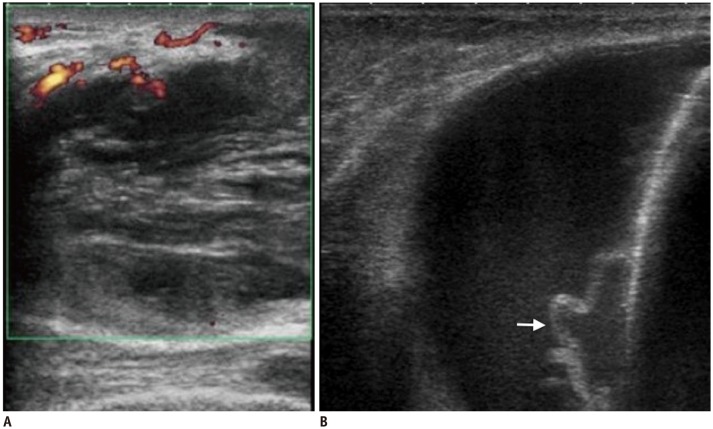 | Fig. 7
Post-procedural breast infections.
A. Post nipple-piercing breast abscess. This is immunocompromised 20-year-old female who presented with left breast swelling and pain post nipple piercing. Ultrasound image of left breast with color Doppler shows hypoechoic collection with heterogeneous content and increased peripheral vascularity. B. Abscess post mastectomy with insertion of tissue expander. This 62-year-old female experienced pain, redness and swelling after mastectomy with insertion of tissue expander. Ultrasound image of affected right breast reveals thick walled, lobulated collection situated posterior to tissue expander (white arrow). Aspiration of this lesion yielded inflammatory cells. No sign of malignant cells was observed.

|
Rare Forms of Infectious Mastitis
Uncommon microorganisms such as mycobacterium tuberculosis, salmonella and fungi may also infect the breast. Tuberculosis of the breast is a rare extra-pulmonary manifestation of tuberculosis infection. It most commonly presents as a unilateral solitary hard breast lump, that may turn into an abscess, form fistulas or ulcerate into the skin. Less commonly, tuberculosis of the breast can present as a multifocal disseminated disease with multiple communicating abscesses and discharging sinuses (
Fig. 8). A rare sclerosing type, of which excessive fibrosis is a dominant feature, has also been described, in which the whole breast is hard with nipple retraction. Diagnosis is usually conformed on tissue sampling and detection of acid-fast bacilli on Ziehl-Neelsen stain or by culture (
91112).
 | Fig. 8
Tuberculosis mastitis in 33-year-old female with chronic discharging sinuses in left breast.
A. Mammogram of left breast demonstrates partially circumscribed masses in left breast (white arrows). B. Ultrasound of left breast reveals collections (black arrow) with fistulous tracts to skin surface (white arrow). C. T1-weighted fat saturated MR imaging of left breast in sagittal plane shows rim-enhancing collections (black arrow) with fistulous tracts to skin surface (white arrow). US-guided biopsy of these lesions revealed presence of acid-fast bacilli, in keeping with diagnosis of tuberculous mastitis. Chest radiograph was also conducted for this patient. However it did not reveal any sign of infection.

|
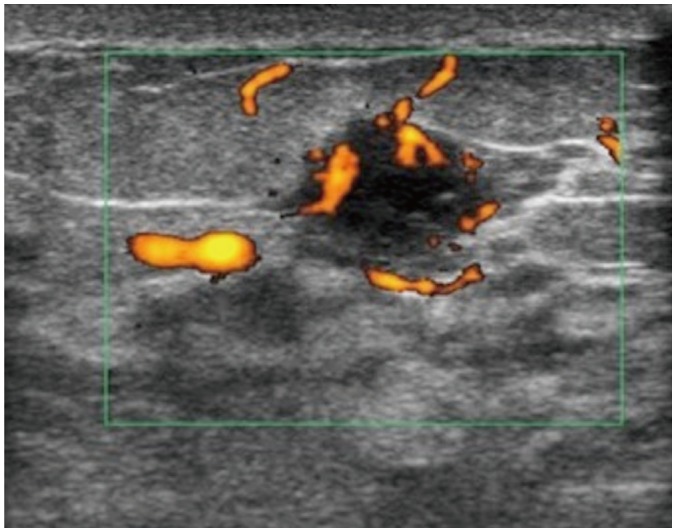
Infected Skin Lesions
Skin lesions such as epidermal inclusion cysts or sebaceous cysts can be infected. Radiological investigations reveal dermal lesion, often well circumscribed with mixed echogenicity, reflecting varying internal contents (
Fig. 9). There may be presence of a tract extending to the skin surface (
13). Inflammatory changes may extend into the surrounding subcutaneous tissue or even into the breast parenchyma (
1).
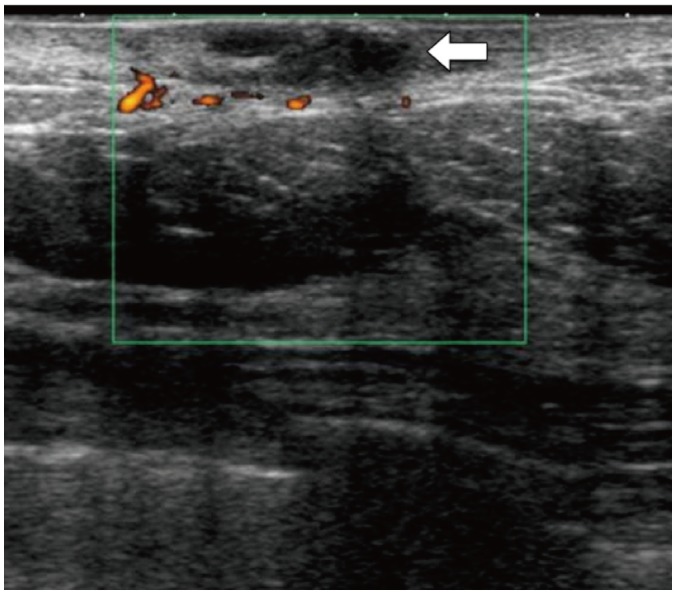 | Fig. 9
Infected sebaceous cyst in 59-year-old female with painful left breast lump.
Ultrasound of left breast with color Doppler reveals hypoechoic lesion within dermis with surrounding increased vascularity (white arrow). No deep extension of this lesion is observed. Surrounding skin is thickened.

|
Go to :

Non-Infectious Mastitis
Idiopathic Granulomatous Mastitis
This is a rare form of mastitis that usually occurs in young women within a few years following childbirth (
13). Its clinical and radiological presentation mimics breast malignancy (
7). It may present with a palpable lump, or a more diffuse involvement of the breast (
Fig. 10). This is usually accompanied with lymphadenopathy. In some cases, aseptic abscesses can develop, that may form sinus tracts with the overlying skin. Diagnosis is usually confirmed on histology, which demonstrates well-formed non-caseating granulomata with epithelioid macrophages and Langhans-type multinucleated giant cells (
139).
 | Fig. 10
Chronic granulomatous mastitis in 40-year-old female with long standing right breast pain and swelling.
A. Mammogram of breasts in mediolateral oblique projection shows ill-defined mass in upper half of right breast (white arrow). There is also enlarged right axillary node (black arrow). B. Ultrasound examination reveals lobulated heterogeneously hypoechoic lesion in upper half of right breast. This lesion has imaging features that are suspicious for malignancy and ultrasound guided biopsy was conducted. Histological diagnosis of chronic granulomatous mastitis was made.

|
Xanthogranulomatous Mastitis
Xanthogranulomas are usually well-circumscribed cutaneous nodules or indurated plaques that occur elsewhere in the body, with predilection for the periorbital area. Extra-cutaneous involvement is rare; involvement of the breast is even more uncommon. Imaging findings in the breast are variable (
Fig. 11). These lesions are characterized on histology by the presence of multi-nucleated giant cells, lipid-laden macrophages (also called xanthoma cells or foamy histiocytes) and cholesterol crystals (
1214).
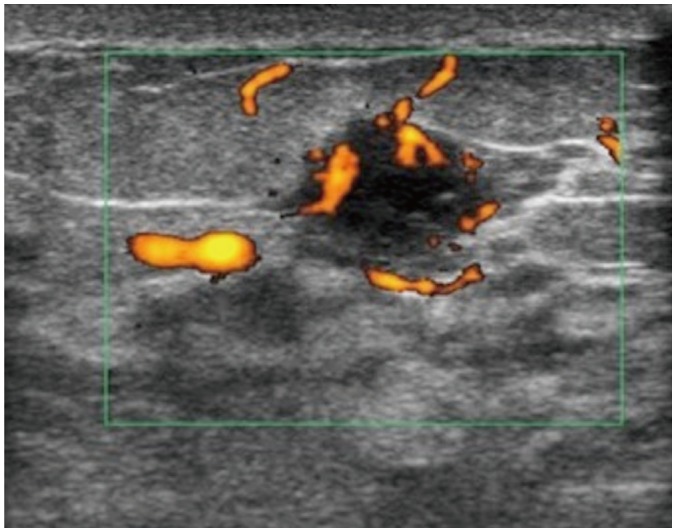 | Fig. 11
Xanthogranulomatous mastitis in 41-year old female 34 weeks pregnant with pain in upper inner quadrant of left breast.
Hypoechoic well-circumscribed lesion was seen in 2:00 position of left breast with surrounding and internal increased vascularity. This was thought to be likely related to lactational changes. However, due to presence of increased vascularity, this lesion was biopsied and histology revealed xanthogranulomatous mastitis.

|
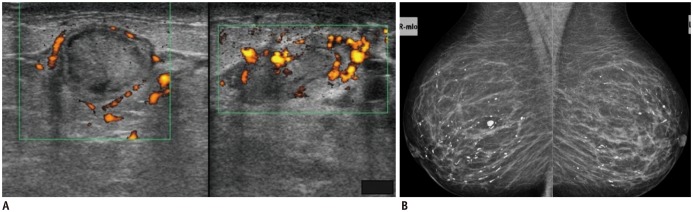
Plasma Cell Mastitis
Plasma cell mastitis, also known as duct ectasia or periductal mastitis, is a benign inflammatory disease of the breast that may present with nipple discharge and nipple retraction, which mimics malignancy. On ultrasound, dilated ducts are noted with echogenic material within (debris) and surrounding increased vascularity (
Fig. 12A). On mammography, inspissated calcified intra-ductal content will show up as large rod-like branching calcifications radiating from the nipple (
39) (
Fig. 12B).
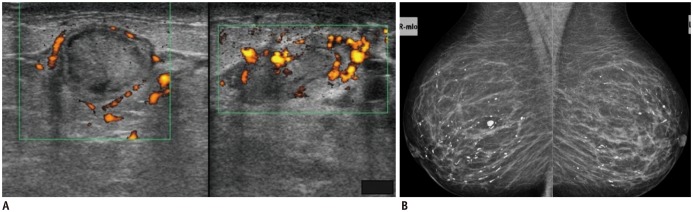 | Fig. 12
Plasma cell mastitis.
A. Plasma cell mastitis in non-lactating 34-year-old female with pain and swelling in lower half of left breast and nipple discharge. Ultrasound images of left breast in transverse (image on left) and longitudinal views (image on right) reveal markedly dilated intramammary duct in retroareolar region with echogenic content and surrounding increased vascularity. Ultrasound-guided biopsy of this duct was conducted to rule out malignancy, which only yielded inflammatory cells. B. Plasma cell mastitis in asymptomatic 71-year-old female at screening mammogram. Mammogram of both breasts in mediolateral oblique view shows characteristic large rod-like branching calcifications in both breasts.

|
Diabetic Mastopathy
Diabetic mastopathy is another condition that is frequently mistaken for carcinoma due to its often indistinguishable radiological presentation (
39). It usually occurs in patients with longstanding insulin dependent diabetes. Patients usually present with large, painless, hard breast masses. Multifocal or bilateral breast involvement is not uncommon (
7). On mammogram, ill-defined masses or asymmetrical densities can be seen. On ultrasound, diabetic mastopathy often manifest as ill-defined hypoechoic lesions with significant posterior acoustic shadowing (
12) (
Fig. 13). Diagnosis is usually confirmed on histology (
3).
 | Fig. 13
Diabetic mastopathy in 29-year-old female with Type I diabetes, presenting with palpable lumps in upper outer quadrants of both breasts.
Ultrasound of upper half of left breast reveals ill-defined heterogeneously hypoechoic area, with posterior acoustic shadowing. Similar findings were also observed over right breast.

|
Go to :

Malignant Mastitis
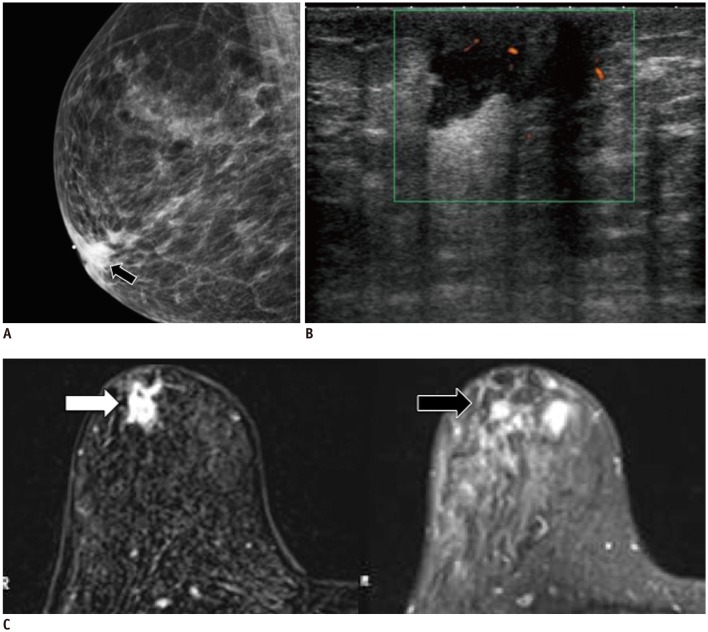
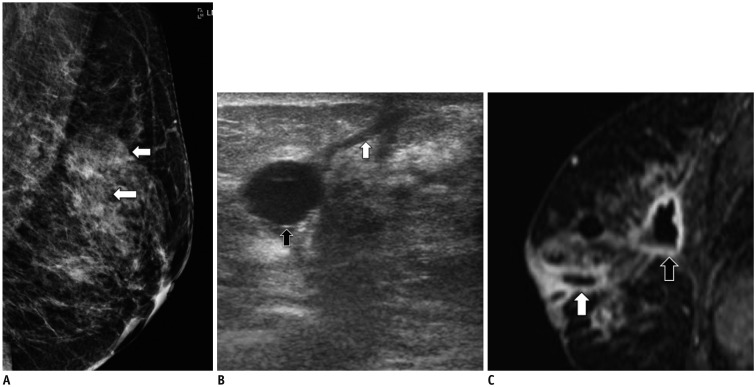
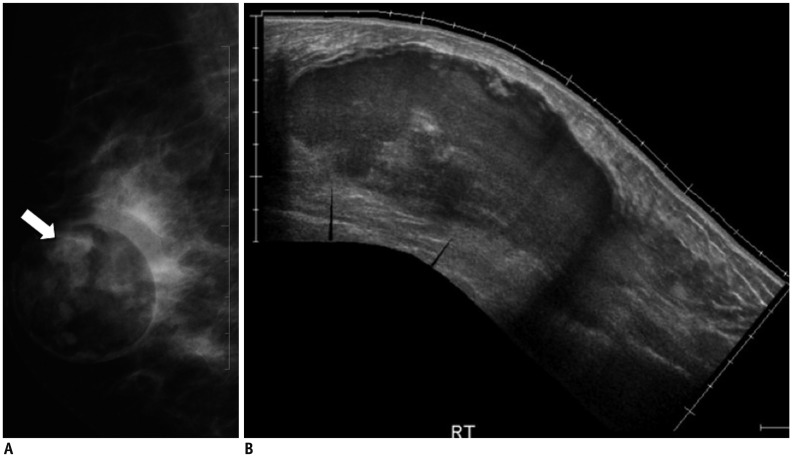
Inflammatory Breast Cancer
Inflammatory breast cancer is an invasive aggressive disease with high rate of metastasis at diagnosis (
1). Clinical symptoms include palpable tumor, skin erythema, edema and warmth, breast enlargement and nipple retraction. Some patients may present with breast pain. Mammographic findings include skin thickening, increased breast density and trabeculation (
15). On ultrasound, subareolar mastitis tends to show mixed solid-cystic lesions or collections. However, inflammatory breast cancers are more likely to show solid mass lesions. On MR imaging, both inflammatory breast cancers and benign mastitis may exhibit similar morphological features such as skin thickening, edema and presence of mass lesions or non-mass like enhancement. Their differences, however, lie in their enhancement characteristics. Masses in inflammatory breast cancer tend to display greater initial enhancement and more frequent subsequent washout. Lesions in benign mastitis tend to show a more persistent or plateaued enhancement pattern. Lesions in benign mastitis also tend to occur in a subareolar location, whereas malignant lesions tend to occur either centrally or dorsally within the breast tissue (
2). Any non-lactating patient with mastitis that does not respond to antibiotic therapy should undergo biopsy to exclude presence of malignancy (
315) (
Fig. 14).
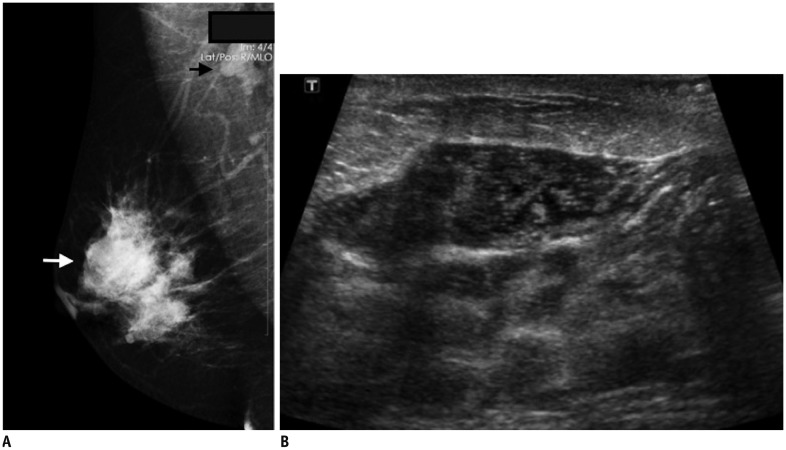
 | Fig. 14
Inflammatory breast carcinoma in 43-year-old, presenting with right breast lump, pain and erythema with yellow nipple discharge and palpable right axillary lymph nodes.
A. Mammogram of both breasts in mediolateral oblique view demonstrates ill-defined opacity on lower half of right breast (black arrows) with overlying skin thickening (white arrows). B. Ultrasound of right breast reveals heterogeneously hypoechoic, solid-cystic mass with increased peripheral vascularity. C. Enlarged right axillary node is observed with loss of normal fatty hilum and thickened cortex. US-guided biopsy was conducted on right breast mass and axillary node. Histology confirms presence of invasive carcinoma with ductal features.

|
Go to :

CONCLUSION
Inflammatory breast diseases consist of a wide array of conditions ranging from the benign simple infective mastitis to breast malignancy. Imaging features of benign and malignant inflammatory conditions often overlap which may cause diagnostic confusion and possibly delay proper treatment. In some cases, correlation with clinical history and risk factors may be useful. For example, in a case of a lactating female, with signs of inflammation, benign mastitis is the most probable diagnosis and treatment can be initiated with follow-up imaging to look for resolution. Complications of breast infection, such as abscess formation or fistulas should also be sought after. The radiologist should be familiar with the range of common inflammatory breast conditions and should also be aware of specific disease patterns such as Zuska's disease and diabetic mastopathy. Mastitis that does not resolve or respond to antibiotic therapy should always be further evaluated with biopsy to rule out presence of malignancy.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download