Abstract
Objective
To prospectively investigate the feasibility of using 2 small intravenous catheters for high-rate computed tomography (CT) contrast injection in patients lacking superficial veins capable of accommodating ≤ 20-gauge catheters.
Materials and Methods
Sixty-eight consecutive eligible adults referred for dynamic liver CT were enrolled; 58 had previously undergone liver CT, including 8 that experienced extravasation. Two 22- or 24-gauge catheters were placed in all patients after 2–5 venipunctures, and 2 mL/kg of contrast agent (370 mg I/mL) was split-administered through both catheters to achieve total flow rate of 4 mL/s. Patients' experience and examination success rate, defined as uneventful scans completed at 4 mL/s or at < 4 mL/s achieving standard image quality in all phases, were analyzed. Quantitative hepatic signal-to-noise and hepatic vascular contrast-to-noise ratios (CNRs) were compared with 30 control examinations scanned at 4 mL/s using an 18-gauge catheter.
Results
One case each of extravasation and severe injection pain caused the examination to be aborted. Success rate was 88.2% (60/68; 54 patients scanned at 4 mL/s, 6 at 3.5–3.9 mL/s). Fifty-five of 58 patients (94.8%) that had past CT regarded the venipuncture as more tolerable than (n = 36) or similar to (n = 19) past experiences; 45 of 58 patients (77.6%) found contrast injection less painful than (n = 35) or similar to (n = 10) past experiences. When compared with control examinations, signal-to-noise ratio was similar in all phases (p ≥ 0.502), but the hepatic arterial CNR in arterial phase was slightly inferior (p ≤ 0.047).
Computed tomography (CT) is a key element in modern medical diagnoses. Most current CT examinations require rapid intravenous injection of a large amount of contrast medium to obtain high-quality, contrast-enhanced images for accurate diagnosis (12). Rapid intravenous injection of contrast agents is particularly critical for examinations that include dynamic multiphase scanning, such as multiphasic liver or angiographic CT, reported to use injection rates ≥ 5 mL/s (345). To deliver CT contrast media at high injection rates, a large (18- or 20-gauge) intravenous catheter is needed (67). However, some patients needing CT examination lack superficial veins that can accommodate such large intravenous catheters because these veins were lost after prolonged treatment requiring multiple/repeated intravenous catheterizations (e.g., oncologic or chronic liver disease patients). Placing a large intravenous catheter in such patients is a substantial challenge even for experienced medical personnel and creates significant issues for the patient. Even if successfully placed, there is high risk of severe pain or venous rupture and contrast extravasation during injection as the fragile vein may not be able to withstand pressure and volume from the rapid contrast injection. Extravasation of intravenously administered iodinated contrast media into the surrounding subcutaneous tissue is a potentially serious complication that may lead to compartment syndrome, skin sloughing, and necrosis (8910).
Therefore, development of new alternative methods to safely achieve high-rate injection of CT contrast medium in patients lacking superficial veins that can accommodate a large intravenous catheter is of critical clinical significance. A previous study reported use of a specially designed fenestrated catheter with multiple side holes to decrease risk of contrast extravasation (3). However, this specialized catheter is not widely available and is expensive. We hypothesized that split-administration of the contrast medium through 2 small intravenous catheters placed at dual sites would be a simple and practical solution, provided total injection rate and volume match that of a large catheter. CT contrast injection through 2 intravenous catheters is not an arcane idea. For example, a 2-catheter approach has been used for pulmonary CT angiography in patients with Fontan physiology to account for their unique hemodynamic circulation (1112). However, it is a unique approach. To our knowledge, the use of a 2-catheter approach to mitigate complications in conducting CT on patients without superficial veins that can accommodate a large intravenous catheter has not been reported. Patient experience with dual venipuncture for non-invasive imaging has not been assessed. Therefore, the purpose of this prospective study was to investigate the feasibility of using 2 small intravenous catheters for patients requiring dynamic multiphase liver CT but lack superficial veins that can accommodate a large intravenous catheter.
The protocol of this prospective study was approved by the Institutional Review Board of Asan Medical Center. Informed consent was obtained from all study participants and was confirmed by the Institutional Review Board.
In January–October 2016, 68 consecutive patients (30 men and 38 women; mean age ± standard deviation [SD], 65.1 ± 9.1 years) that fulfilled the following criteria were enrolled in this study: 1) referred for contrast-enhanced dynamic liver CT (mostly for surveillance, suspicion, or posttreatment follow-up for hepatic malignancy); 2) adults (≥ 20 years old); 3) no superficial arm veins to accommodate 18- or 20-gauge intravenous catheters as assessed by highly experienced nurses (> 5 years of experience in catheter placement for contrast-enhanced CT and an approximate daily case volume of 50 patients); 4) no history or current signs of central venous occlusion in both upper extremities; and 5) out-patients without hemodynamic instability. Sample size estimation is explained further in the statistical analysis section. Fifty-eight of the 68 patients (27 men and 31 women; mean age ± SD, 65.3 ± 9.3 years) underwent dynamic liver CT 1–13 months prior (median, 3 months; interquartile range, 4 months), and 37 experienced difficulties during the previous CT, such as difficult intravenous catheter placement requiring multiple needle punctures (n = 26), contrast extravasation (n = 8), and severe pain during contrast injection (n = 3). We additionally recruited 30 consecutive control patients that had superficial arm veins capable of accommodating an 18-gauge intravenous catheter and met other eligibility criteria. Characteristics of both patient groups are summarized in Table 1. The 68 patients in the 2-catheter group revealed greater mean age and had significantly more women than the 30 control patients. Otherwise, the 2 groups were not significantly different.
Highly experienced nurses conducted placement of the 2 intravenous catheters (Fig. 1) for all 68 patients using either 22- or 24-gauge catheters (BD Angiocath Plus; Becton-Dickinson and Company, Franklin Lakes, NJ, USA). Both catheters were placed in all 68 patients after 2–5 venipuncture attempts (median, 2 times); 2 22-gauge catheters were placed in 53 patients, 1 22- and 1 24-guage catheter were placed in 12 patients, and 2 24-guage catheters were placed in 3 patients. Catheters were placed bilaterally in the upper extremities in 60 patients and unilaterally in 8 (left side only, 5 patients; right side only, 3 patients). Unilateral placement was necessary in cases wherein there were no superficial veins present to accommodate even small catheters in one arm. Overall, 127 catheters were placed in the wrist or hand and 9 were placed in the forearm. In the control group, an 18-gauge catheter (BD Angiocath Plus; Becton-Dickinson and Company) was placed in the forearm of all patients.
Iopamidol (370 mgI/mL, Pamiray 370; Dongkook Pharmaceutical, Seoul, Korea) was administered intravenously (2 mL/kg; maximum, 150 mL) using an automatic double-head power injector (OptiVantage DH; Covidien, Mansfield, MA, USA). Nurses that conducted the venipuncture empirically determined maximum tolerable injection rate for each catheter according to resistance/pressure perceived during a test hand injection of a small amount of saline (approximately 2–3 mL) through each catheter. Then, desired total injection rate of 4 mL/s was split between the 2 catheters accordingly (Fig. 2). In 12 patients, total rate had to be lowered to 3.5–3.9 mL/s because of the fragility and small size of the veins. Split ratio between the 2 catheters for the 68 patients was 1:1 to 1:2.5. In control patients, 2 mL/kg (maximum, 150 mL) iopamidol was administered at a rate of 4 mL/s through an 18-gauge catheter. Intracatheter pressure during contrast injection was continuously monitored, and peak pressure was recorded. In patients with 2 intravenous catheters, only the catheter with higher pressure at any time was recorded due to technical configuration of the pressure monitoring system. Incidences of extravasation or severe pain in injection sites that required cessation of contrast injection were noted.
CT scans were conducted using a 128-detector row scanner (SOMATOM Definition AS+; Siemens, Erlangen, Germany). Arterial (using bolus triggering with a 25-second delay after attenuation of the aorta at the thoracolumbar junction had reached 100 Hounsefield unit [HU]), portal (30 seconds after completion of the arterial phase), and delayed (95 seconds after finishing the portal phase) contrast-enhanced images through the liver were obtained using 64 × 0.6-mm beam collimation, beam pitch of 1, 0.5-second gantry rotation time, field of view to fit, 120 kVp, automated tube current modulation with 200-mA quality reference, and 5-mm slice thickness and increment.
An experienced clinical research coordinator that did not participate in other study procedures assessed each patient's experience using a set of uniform questionnaires. Immediately after placement of the 2 intravenous catheters, but before contrast injection, the 58 patients that previously underwent liver CT were asked if they perceived the current catheter placement to be more, the same, or less tolerable compared with their previous experience. After CT examination, they were asked if the contrast injection was less, the same, or more painful at either of the 2 venipuncture sites compared with their previous experience. All 68 patients were asked about their willingness to use the small 2-catheter approach for a later CT examination using a 10-point Likert scale (0 = definite unwillingness; 5 = indeterminate; 10 = definite willingness).
CT images from the 2-catheter and the control groups were randomly mixed, and their visual quality was independently evaluated by 3 readers. Readers were board-certified gastrointestinal radiologists with 2 years of non-trainee experience with liver CT (approximately 300 cases/month) and were completely blinded to the group assignment, as well as other parts of the study design to avoid bias. Readers conducted qualitative visual assessment using a 4-point system (grade 4 = better than standard liver CT quality; grade 3 = same as usual quality; grade 2 = worse than usual quality but diagnostically acceptable; and grade 1 = worse than usual quality and diagnostically unacceptable) separately for each scan phase.
Another radiologist blinded to the group assignment and study design quantitatively measured signal-to-noise ratio (SNR) of the liver separately for each scan phase according to a method described elsewhere (13) and measured contrast-to-noise ratio (CNR) of the hepatic artery and the portal vein in arterial and the portal phases, respectively. To measure the hepatic signal, 3 circular regions of interest (diameter, 1–1.5 cm each) were carefully placed in separate, relatively homogeneous areas in the right hepatic lobe, approximately half way from the hilum and hepatic surface, away from discernible vessels or focal changes in attenuation, and the average of the 3 mean HU values was used as the hepatic signal. Image noise was measured in the same manner by averaging 3 region-of-interest measurements of SD values in the homogenous subcutaneous fat of the anterior abdominal wall at the midabdomen level. Regarding vascular measurements, as the hepatic artery and intrahepatic portal veins are too small for accurate HU measurements, we instead used the average of 3 measurements on 3 consecutive images of the aorta at the level of the celiac axis and of the main portal vein, respectively, according to a published method (14). Hepatic SNR was then calculated by dividing the hepatic signal with the image noise, and hepatic vessel-to-liver CNR was calculated by dividing the vessel-to-liver difference with the image noise.
Examination success rate, defined as completion of scanning without extravasation or cessation at a total injection rate of 4 mL/s or at lower rates with an image quality grade ≥ 3 in all phases (as judged by all 3 independent readers), was the primary endpoint. We intended to estimate the primary endpoint within ± 10% (i.e., 2-sided 95% confidence interval with a 10% width on each side). We predicted an 80–90% examination success rate, that required 43–68 patients. Patient experience results in the 2-catheter groups were summarized using proportions for categorical items and using median and interquartile range for the 10-point Likert scale scores. In the 58 patients that had previously undergone liver CT, results were compared between those that had experienced and those that had not experienced problems regarding intravenous catheter placement or contrast injection during the previous CT examination using the Fisher exact or Wilcoxon's rank sum tests wherein appropriate. Peak intracatheter pressure during contrast injection, image quality grades, hepatic HU, hepatic SNR, and hepatic vessel-to-liver CNR between the 2-catheter group and the control group were compared using independent sample t test or the Wilcoxon rank sum test, appropriately. Sample size was estimated using PASS 12 (NCSS, Kaysville, UT, USA), and other analyses were conducted using SPSS for Windows version 21.0 (IBM Corp., Armonk, NY, USA). A p < 0.05 was statistical significance.
Examination success rate was 88.2% (60/68; 95% confidence interval, 78.2–94.2); successful completion of the scan at a total injection rate of 4 mL/s in 54 patients and at 3.5–3.9 mL/s with an image quality grade ≥ 3 in all phases as judged by all 3 independent readers in 6 patients.
Of the 58 patients that previously underwent liver CT in the 2-catheter group, 62.1% (36/58) regarded placement of the 2 small intravenous catheters as more tolerable than their previous experience despite the 2–5 venipunctures (median, 2 times) required. The rate was slightly higher among those that had previously experienced venipuncture/contrast injection-related difficulties (67.6%; 25/37) than those that had not (52.4%; 11/21), although not significantly (p = 0.275) (Table 2).
Of the 56 patients in the 2-catheter group that sustained total injection rate of 4 mL/s, 54 were scanned without adverse events, whereas the remaining 2 experienced contrast extravasations (1 case; after injecting 34 mL) and severe pain at the venipuncture site (1 case; after injecting 29 mL) and had to abort the examination (Fig. 3). The other 12 patients in the 2-catheter group achieved total injection rate of 3.5–3.9 mL/s and completed scanning without problems. All 8 patients (out of 58) that had experienced contrast extravasation during a previous CT scan were examined uneventfully with a total injection rate of 4 mL/s (n = 6), 3.8 mL/s (n = 1), or 3.6 mL/s (n = 1). Peak intracatheter pressure during contrast injection was significantly smaller in the 68 2-catheter group patients than in the control patients (mean pressure ± SD, 96.5 ± 27.2 vs. 117.7 ± 21.9 psi; p < 0.001). Of patients that previously underwent liver CT in the 2-catheter group, 60.4% (35/58) regarded the current contrast injection as less painful at both venipuncture sites than their previous experience. The rate was slightly higher among those that had previously experienced venipuncture/contrast injection-related difficulties (67.6%; 25/37) than those that had not (47.6%; 10/21), although not significantly (p = 0.168) (Table 2).
Median overall experience score for the 2-catheter method was 8 or 9 according to patient grouping, and almost all patients were inclined to use the 2-catheter method in the future (Table 2).
CT examinations of 66 patients in the 2-catheter group excluding the 2 patients whose examinations were aborted (Fig. 3), were compared with the 30 control patients. Image qualities were not significantly different between the 2 groups regarding visual quality as well as quantitative measurements in the portal and delayed scan phases (Tables 3, 4). However, visual quality in the arterial phase as assessed by 1 reviewer (Reader 2) and hepatic artery-to-liver CNR in the arterial phase were significantly lower in the 2-catheter group patients than in the control patients although differences were small (Tables 3, 4).
This study reveals that using 2 small intravenous catheters is an effective and well-received solution for achieving high-rate contrast injection for liver CT in patients lacking superficial veins capable of accommodating a large intravenous catheter. Examination success rate using the 2-catheter method was 88.2%. It is particularly noteworthy that all 8 patients that experienced contrast extravasation during previous CT were examined uneventfully in this study using the small 2-catheter approach (total injection rate = 4 mL/s in 6 of 8 patients). Considering slightly inferior image quality in the arterial phase, one should not entirely equate the 2-catheter method with the usual CT contrast injection using a large intravenous catheter. However, the 2-catheter approach could be a simple, practical solution to obtain high-quality CT examinations in patients lacking large superficial veins.
CT contrast injection through 2 small intravenous catheters instead of a large one is an unconventional approach. It is remarkable that median overall experience score was 8 or 9 (out of 10), with most patients with previous CT experience considering catheter placement (62.1%) and contrast injection (60.4%) as better than their previous experience. It is possible that because most of the patients had experienced prior difficulties with intravenous catheter placement or contrast injection, patient satisfaction could have been inflated to some degree. However, because responses from patients without such experience were similarly favorable, this suggests the 2-catheter approach was well-accepted. Objective data from pressure monitoring were consistent with subjective patient-reported results as peak pressure during contrast injection was significantly lower in the 2-catheter group than in the control group. Because we could only measure higher pressure between the 2 catheters instead of separately measuring the pressure of each, peak pressures recorded in the 2-catheter group were likely slightly overestimated. Lower injection pressure would explain why there were fewer reports of injection-related pain in the 2-catheter group and reduces risk of venous rupture and contrast extravasation, which is a significant advantage.
Efforts to decrease CT contrast volume and, thereby, the injection rate have been made in other ways, as well. For example, the current state-of-the-art CT scanners provide multi-kVe spectral imaging capability or enable low kVp imaging without increasing image noise using iterative reconstruction. These scanners allow for augmented contrast enhancement relative to conventional CT for a given amount of contrast medium (15161718192021222324). As these scanners decrease the amount of contrast agent needed, injection flow rate and need for large intravenous catheters can be reduced. Combining the 2-intravenous catheter approach with the latest CT technology may resolve most cases of difficulty or inability to perform contrast-enhanced CT due to the lack of superficial veins capable of accommodating a large intravenous catheter.
One technical disadvantage of the 2-catheter approach is that it is only possible with at least dual-head injectors and that it precludes use of saline flushing because both cylinders of a dual-head injector system must be used to inject contrast material. Therefore, unless injectors with more than 2 cylinders are available, this technique would be unsuitable for CT examinations for which saline flushing is crucial.
This study had limitations. First, patients included in this study were undergoing liver CT, and results may differ by patient groups because those with other diseases may have different subjective perceptions towards intravenous catheterization and CT contrast injection. We chose this group of patients because liver CT requires high-rate contrast injection, and image quality is sensitive to the injection process (12). Second, some patients, albeit a small number, could not recall their experience during their previous CT examination; these patients were recorded as “uncertain” to avoid inaccuracy in results. Finally, the 2-catheter group had higher mean age and a greater proportion of women than the control group. However, these intergroup differences are natural because superficial veins in upper extremities are generally thinner and more fragile in older patients and women.
In conclusion, using 2 small intravenous catheters is an effective and well-received solution for patients requiring high-rate contrast injection for liver CT but lacking superficial veins capable of accommodating a large intravenous catheter. This method enables quality liver CT examination and obviates the need for costly or specialized catheters.
Figures and Tables
 | Fig. 1Placement of 2 small intravenous catheters and dynamic liver CT obtained using them in 61-year-old female.
A. Two intravenous catheters (24- and 22-gauge) placed in left thumb and lateral side of right hand (arrows), respectively. B. Arterial- (left), portal- (middle), and delayed- (right) phase contrast-enhanced CT images obtained with 4 mL/s total injection rate. CT = computed tomography
|
 | Fig. 2Simultaneous contrast injection through 2 intravenous catheters.Two coiled intravenous tubing (arrows) are observed, one each connecting one cylinder of dual-head injector to one intravenous catheter (this exemplary patient is not from study cohort).
|
Table 1
Baseline Patient Characteristics
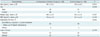
Table 2
Experience of Patients Who Underwent CT Using 2 Small Intravenous Catheters

Table 3
Comparison of Visual Image Quality between 2-Catheter and Control Groups

Table 4
Comparison of Quantitative Hepatic Attenuation, SNR, and CNR between 2-Catheter and Control Groups

References
1. Fishman EK. CTisus: everything you need to know about computed tomography (CT) & CT scanning. August 30, 2017. Web site. http://www.ctisus.com.
2. Springer Healthcare. MDCT.net. August 30, 2017Springer Healthcare. Web site. https://mdct.net.
3. Johnson PT, Christensen GM, Fishman EK. I.v. contrast administration with dual source 128-MDCT: a randomized controlled study comparing 18-gauge nonfenestrated and 20-gauge fenestrated catheters for catheter placement success, infusion rate, image quality, and complications. AJR Am J Roentgenol. 2014; 202:1166–1170.

4. Schima W, Hammerstingl R, Catalano C, Marti-Bonmati L, Rummeny EJ, Montero FT, et al. Quadruple-phase MDCT of the liver in patients with suspected hepatocellular carcinoma: effect of contrast material flow rate. AJR Am J Roentgenol. 2006; 186:1571–1579.

5. Cho JS, Kwag JG, Oh YR, Han SD, Song CJ. Detection and characterization of hepatocellular carcinoma: value of dynamic CT during the arterial dominant phase with uniphasic contrast medium injection. J Comput Assist Tomogr. 1996; 20:128–134.

6. Behrendt FF, Bruners P, Keil S, Plumhans C, Mahnken AH, Stanzel S, et al. Impact of different vein catheter sizes for mechanical power injection in CT: in vitro evaluation with use of a circulation phantom. Cardiovasc Intervent Radiol. 2009; 32:25–31.

7. Wienbeck S, Fischbach R, Kloska SP, Seidensticker P, Osada N, Heindel W, et al. Prospective study of access site complications of automated contrast injection with peripheral venous access in MDCT. AJR Am J Roentgenol. 2010; 195:825–829.

8. Nicola R, Shaqdan KW, Aran S, Prabhakar AM, Singh AK, Abujudeh HH. Contrast media extravasation of computed tomography and magnetic resonance imaging: management guidelines for the radiologist. Curr Probl Diagn Radiol. 2016; 45:161–164.

9. Pacheco Compaña FJ, Gago Vidal B, Méndez Díaz C. [Extravasation of contrast media at the puncture site: strategies for managment]. Radiologia. 2014; 56:295–302.
10. Sbitany H, Koltz PF, Mays C, Girotto JA, Langstein HN. CT contrast extravasation in the upper extremity: strategies for management. Int J Surg. 2010; 8:384–386.

11. Sandler KL, Markham LW, Mah ML, Byrum EP, Williams JR. Optimizing CT angiography in patients with Fontan physiology: single-center experience of dual-site power injection. Clin Radiol. 2014; 69:e562–e567.

12. Prabhu SP, Mahmood S, Sena L, Lee EY. MDCT evaluation of pulmonary embolism in children and young adults following a lateral tunnel Fontan procedure: optimizing contrastenhancement techniques. Pediatr Radiol. 2009; 39:938–944.

13. Shuman WP, Chan KT, Busey JM, Mitsumori LM, Choi E, Koprowicz KM, et al. Standard and reduced radiation dose liver CT images: adaptive statistical iterative reconstruction versus model-based iterative reconstruction-comparison of findings and image quality. Radiology. 2014; 273:793–800.

14. Park SH, Kim PN, Kim KW, Lee SW, Yoon SE, Park SW, et al. Macrovesicular hepatic steatosis in living liver donors: use of CT for quantitative and qualitative assessment. Radiology. 2006; 239:105–112.

15. Shuman WP, O'Malley RB, Busey JM, Ramos MM, Koprowicz KM. Prospective comparison of dual-energy CT aortography using 70% reduced iodine dose versus single-energy CT aortography using standard iodine dose in the same patient. Abdom Radiol. 2017; 42:759–765.

16. Lv P, Liu J, Chai Y, Yan X, Gao J, Dong J. Automatic spectral imaging protocol selection and iterative reconstruction in abdominal CT with reduced contrast agent dose: initial experience. Eur Radiol. 2017; 27:374–383.

17. Ma CL, Chen XX, Lei YX, Zhang XR, Jia YJ, Tian X, et al. Clinical value of dual-energy spectral imaging with adaptive statistical iterative reconstruction for reducing contrast medium dose in CT portal venography: in comparison with standard 120-kVp imaging protocol. Br J Radiol. 2016; 89:20151022.

18. Lee JW, Lee G, Lee NK, Moon JI, Ju YH, Suh YJ, et al. Effectiveness of adaptive statistical iterative reconstruction for 64-slice dual-energy computed tomography pulmonary angiography in patients with a reduced iodine load: comparison with standard computed tomography pulmonary angiography. J Comput Assist Tomogr. 2016; 40:777–783.
19. Iyama Y, Nakaura T, Yokoyama K, Kidoh M, Harada K, Tokuyasu S, et al. Impact of knowledge-based iterative model reconstruction in abdominal dynamic CT with low tube voltage and low contrast dose. AJR Am J Roentgenol. 2016; 206:687–693.

20. Chung YE, You JS, Lee HJ, Lim JS, Lee HS, Baek SE, et al. Possible contrast media reduction with low keV monoenergetic images in the detection of focal liver lesions: a dual-energy CT animal study. PLoS One. 2015; 10:e0133170.

21. Noda Y, Kanematsu M, Goshima S, Kondo H, Watanabe H, Kawada H, et al. Reduction of iodine load in CT imaging of pancreas acquired with low tube voltage and an adaptive statistical iterative reconstruction technique. J Comput Assist Tomogr. 2014; 38:714–720.

22. Chen CM, Chu SY, Hsu MY, Liao YL, Tsai HY. Low-tube-voltage(80 kVp) CT aortography using 320-row volume CT with adaptive iterative reconstruction: lower contrast medium and radiation dose. Eur Radiol. 2014; 24:460–468.
23. Nakaura T, Nakamura S, Maruyama N, Funama Y, Awai K, Harada K, et al. Low contrast agent and radiation dose protocol for hepatic dynamic CT of thin adults at 256-detector row CT: effect of low tube voltage and hybrid iterative reconstruction algorithm on image quality. Radiology. 2012; 264:445–454.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download