Abstract
Magnetic resonance imaging is the optimal modality for pelvic imaging. It is based on T2-weighted magnetic resonance (MR) sequences allowing uterine and vaginal cavity assessment as well as rectal evaluation. Anatomical depiction of these structures may benefit from distension, and conditions either developing inside the lumen of cavities or coming from the outside may then be better delineated and localized. The need for distension, either rectal or vaginal, and the way to conduct it are matters of debate, depending on indication for which the MR examination is being conducted. In this review, we discuss advantages and potential drawbacks of this technique, based on literature and our experience, in the evaluation of various gynecological and rectal diseases.
Magnetic resonance imaging (MRI) is widely recognized as the imaging modality of choice for the evaluation of the pelvis. Magnetic resonance (MR) examinations are based on T2-weighted MR imaging, allowing depiction of the uterus cavity, rectum lumen and vagina. The anatomy of these structures is best observed when the walls, that may spontaneously be collapsed, are distended. Distension of these cavities during pelvic MRI for evaluation of gynecologic or rectal diseases has been conducted with a variety of methods: vagina may be filled with ultrasound gel (12), saline solution (3), and rectum may be distended, among other materials, with air (“air balloon technique”) (4) or potato starch combined with gadolinium-based contrast media (567).
Among these different agents, ultrasound gel has the advantage to ensure stable distension of cavities and to provide high contrast with adjacent structures on T2-weighted images, thus facilitating, in some cases, diagnosis and evaluation of benign and malignant gynecologic or rectal conditions. The purpose of this review is to report and illustrate our experience in this field as well as to review literature findings in terms of use of vaginal and rectal opacification for various indications.
Pelvic MRI may be conducted either using 1.5T or 3T MR units. Although 3T MR imaging has inherent higher resolution, yields high contrast between tissue and fluid could thus provide more detailed depiction of rectal/vaginal walls, there has not been clear evidence in literature, to support superiority of 3T vs. 1.5T pelvic MR imaging in the field of rectal or gynecological disorders. The only study addressing an intra-patient comparison of 1.5T and 3T MRI performances for staging in patients with rectal cancer did not reveal improvement with 3T MRI. No rectal filling was conducted before imaging in that study (8). Another recent study comparing results of pelvic MRI conducted for rectal cancer in 50 patients imaged without and after rectal filling concluded that rectal distension improved visualization of tumors, even though studies were conducted on a 3T MR unit (9).
Three different types of distension may be conducted depending on studied pathology. Vaginal distension may be conducted alone in conditions such as cervix and endometrial carcinomas, developmental abnormalities and vaginal cysts, while vaginal and rectal filling may be undertaken in endometriosis or pelvic floor disorders such as cystocele, vaginal prolapse and rectocele. Last, rectal distension can be conducted alone to evaluate rectal cancer. When vaginal and/or rectal distension is scheduled, the patient should be familiarized with intention and course of the procedure. With adequate information provided to the patient before administration, tolerability is good with an acceptance rate ranging from 91.3% to 98.7% (101112). The approach to the patient preparation depends on the indication. Most gynecological pathologies do not require colonic preparation.
However, in case of endometriosis, most authors ask their patients to undergo bowel cleansing to maximize detection of a rectal implant (11131415) and fasting is recommended (1415), in studies using 1T and 1.5T scans. Many methods are being used throughout literature for bowel cleansing, mainly on 1.5T devices (13467810131415161718). They include administration of two doses of an oral laxative the day before the study (15), or of an oral mild laxative senna extract for 3 days (1617), or of a 120-mL single dose of ready-to-use enema kept by the patient for 15 minutes before bowel movement (18). In their recent guidelines, European Society of Urogenital Radiology (ESUR) recommend fasting prior to MRI (3–6 hours before MRI) and consider bowel preparation as “best practice” for detection of deep pelvic endometriosis (DPE) (19).
To reduce bowel peristalsis and avoid gastrointestinal tract artifacts, an antispasmodic agent is generally administered (1011131820), intravenously or intramuscularly, in absence of contraindication. Specifically, ESUR's guidelines recommend use of anti-peristaltic agent in the evaluation of DPE (19).
As far as endometriosis is concerned, the vagina and the rectum may be filled immediately before examination, with the patient in left lateral decubitus position inside the MR scanner. Most centers use ultrasound gel, either sterile (101121) or not sterile (161718), as gel is a widely available contrast agent, low-cost, easy to use and administer, and convenient for vaginal and rectal distension. As it is viscous, it allows good expansion of hollow organs and doesn't leak during the procedure. The amount of gel used to fill the vagina and the rectum is a matter of debate. Usually, using 1.5T units, 50 mL (141516171821) to 100 mL (10) can be used to fill the vagina. Rectum should be filled with approximately 100–150 mL of sonographic gel (1114161718).
Regarding dynamic pelvic study, ESUR and European Society of Gastrointestinal and Abdominal Radiology (ESGAR)'s recommendations suggest that the rectum should be filled with a large amount of gel (180–200 mL) to improve capacity to defecate (22). In literature, the amount varies between 100–300 mL (12623242526). Investigators either use standardized amount of gel or administer gel until the patient expresses an urge to relieve the bowel (16). A recent study has revealed that decreasing rectal gel volume from 180–120 mL did not compromise defecation performance (24). Although no consensus could be obtained among experts from the ESGAR and the ESUR (22), a rectal cleansing enema prior to examination is beneficial. When vaginal opacification is conducted, quantity introduced is generally between 20 mL and 50 mL, in studies conducted on 1.5T units (122232627).
As far as rectal cancer evaluation is conducted, when used, the amount of ultrasound gel should not exceed 60 mL to avoid potential compression of the mesorectum (28). In our experience, 50 mL and 250 mL of non-sterile ultrasound gel are used to fill the vagina and the rectum, respectively, for evaluation of DPE and dynamic pelvic studies. For evaluation of cervix or endometrial carcinomas, developmental anomalies and vaginal cysts, we conduct a vaginal opacification with 50 mL of ultrasound gel. For rectal cancer evaluation, we gently fill the rectum with 60–80 mL of ultrasound gel, but do not consider it mandatory. Last, patients do not fast prior to our pelvic MRI studies, nor undergo colonic preparation nor receive antispasmolytic agents.
Endometriosis is abnormal presence of endometrial tissue outside the uterus. DPE is histologically defined as an endometriotic lesion penetrating into the retroperitoneal space or into the wall of the pelvic organs to a depth of at least five millimeters (11).
Endometriosis lesions are most commonly seen in ovaries and the pelvic peritoneum, followed in order of decreasing frequency by deep lesions of the pelvic subperitoneal space, the intestinal tract, and urinary system. Endometriotic lesions mainly appear as well-defined nodules or wall thickening of low signal intensity on T2-weighted MR images corresponding to abundant fibrous tissue observed in these lesions at histologic examination.
Posterior deeply infiltrating endometriosis may involve anatomic structures that border the pouch of Douglas, i.e., posterior border of the cervix and isthmus of the uterus, uterosacral ligaments (USL), vaginal wall, and anterior wall of the rectum or rectosigmoid junction. Knowledge of precise distribution of the endometriosis is crucial, as it may be beneficial in determining surgical options and minimizing complications. It is widely recognized that MRI is the best imaging modality for detection and pre-surgical mapping of deep implants of endometriosis. However, MRI may be limited for identification of USL, particularly in patients with retroflexed uterus and when pelvic anatomy is distorted by nodules or infiltrating masses of deep endometriosis. Involvement of the vagina is seen in approximately 15% of cases and the rectovaginal septum (RVS) may sometimes be difficult to assess, particularly if the fornices or/and vaginal wall are collapsed.
According to the ESUR, vaginal and rectal opacification are “optional” in diagnosis of DPE (19). Results of studies addressing this issue of added value of vaginal opacification, using 1T or 1.5T units, are discrepant (10111317). Two studies report no significant added value for expert readers in terms of improved sensitivity with the adjunct of post contrast MRI (1113), whereas results of two other studies (1017) report better evaluation of DPE. It is noteworthy that evaluation in terms of improvement of Douglas pouch obliteration was controversial in one study (10).
No consensus exists in literature on the value of rectal opacification in diagnosis of DPE. Some authors claim that rectal opacification provides better evaluation of pouch of Douglas and of rectosigmoid colon involvement (16171829), while several other studies argue that this technique is useless in evaluation of posterior DPE locations (131530), all studies except one (30) conducted on a 1.5T unit. Drawbacks of systematic rectal opacification include that rectal opacification is time-consuming, may result in patient discomfort, and may cause increased bowel peristalsis and subsequent blurring of bowel segments (1530). Some authors, working at 3T, suggest that endorectal gel should be administered only in presence of symptoms that may be related to rectal involvement, such as constipation, hematochezia, or painful defecation (20).
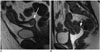
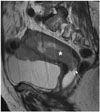
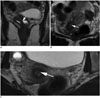
According to our experience, use of vaginal opacification unfolds vaginal walls, thus increasing detection of small lesions, with better accuracy regarding intra- or extra-vaginal location of a lesion and assessing extension of endometriosis to the cervix (Fig. 1) and to vaginal fornices (Figs. 2, 3). Rectal opacification improves distension of the rectosigmoid colon allowing clear delineation of bowel lumen and the wall and, therefore, accurate assessment of anatomic distribution of endometriotic lesions (Fig. 4).
In conclusion, the question of usefulness of using vaginal and rectal opacification in endometriosis is unclear. We believe from our experience that it has the undisputed advantage of providing interesting information particularly for small vaginal lesions, posterior vaginal fornix and anterior rectal wall, and that it enables less experimented radiologists to better interpret deep endometriosis as suggested in the study by Chassang et al. (11).
Recent recommendations from the Urogenital Society of Radiology state that vaginal/rectal opacification is “optional” for staging of uterine cervical cancer, as it is used by few expert centers (31). According to these guidelines, vaginal opacification is useful in case vaginal extension of the tumor is suspected. It facilitates differentiating tumors International Federation of Gynecology and Obstetrics (FIGO) IIA from FIGO IB, particularly regarding extension to the posterior vaginal fornix (3132) (Figs. 5, 6). Akata et al. (32) studied the MRI tumoral staging obtained in 50 patients diagnosed with cervical carcinoma that prospectively underwent pelvic MRI before and after vaginal opacification, with correlation to pathological results. The authors revealed that opacification correctly lowered staging in 7 patients, compared to pre-opacification MRI and that it accurately increased it in 3, changing treatment planning in 14% of cases, with appropriate treatment chosen in 90% of cases versus 79% without use of vaginal opacification (32). Finally, vaginal opacification allows better evaluation of tumoral size, particularly in case of vaginal involvement and facilitates detecting signs of local recurrence, particularly after trachelectomy and conization (3).
The use of gel-based vaginal distension may be beneficial in case of endometrial cancer in to accurately assess vaginal extension (Fig. 7). We share the same experience with Young et al. (33), that revealed in a study dealing with 9 patients with cervical, vaginal and endometrial cancers that underwent 1.5T pelvic MRI before and after gel opacification that use of vaginal distension improves staging.
There is a general agreement that evaluation of the pelvic floor should be conducted using rectal opacification (22). The rectum must be distended to delineate the anorectal junction, rectocele and intussusceptions, and to study active defecation. It is critical that the patient evacuate the total amount of gel to analyze defecation (Fig. 8).
Müllerian duct anomalies (MDA) are rare conditions, estimated to be approximately 5.5% in the population. They may somehow be encountered by the radiologist as MDA's prevalence has been estimated at 8.0% in infertile women, 13.3% in those with a history of miscarriage, and 24.5% in those with miscarriage and infertility (35). Surgery can be beneficial in several cases, and MRI is useful to select patients that can benefit from surgical treatment. Although several authors do not use vaginal opacification in case of evaluation of Müllerian duct anomalies (3637), it may allow optimal depiction of vaginal abnormalities such as septations or duplications (38) that may be easily overlooked in absence of adequate vaginal distention. It may facilitate in differentiating presence of double cervices versus one cervix.
As far as longitudinal vaginal septum is concerned, it may go undiagnosed if cavities are not obstructed. The septum, that can be either perforate (incomplete) or imperforate (complete), is best demonstrated on T2-weighted MR images, when intracavitary gel is used thanks to contrast between low-signal-intensity septum and high signal intensity gel (Figs. 9, 10). Use of vaginal opacification may be of some help for the surgeon before reconstruction, to optimally assess vaginal agenesis or segmental vaginal atresia (Fig. 11).
Magnetic resonance imaging best characterizes anatomic location of vaginal cysts, allowing the radiologist to differentiate these from other regional formations such as urethral diverticula, cervical cysts or Skene glands. Vaginal cysts are mainly diagnosed based on location. Vaginal opacification may be useful, if a cyst is too large to assess its precise localization or if the connection with the vaginal wall is difficult to depict (Fig. 12).
As far as anorectal diseases are concerned, rectal cancer is the only condition for which use of rectal filling may be of interest. However, it is not part of recommendations issued by a panel of experts from the European Society of Gastrointestinal and Abdominal Radiology (39) because the primary goal of rectal tumor staging is not to assess the endoluminal part of the rectal tumor but rather the extent of the tumor growth through the bowel wall. It has been reported that distension of the rectum may compress the mesorectal fat thus leading to overestimation of fascial involvement, although this notion has not been further validated (40). Rectal filling may be beneficial for unexperienced readers, for easier delineation of the inferior tumor pole and subsequent measurement to the anal margin or assessment to the relationships with anal sphincters. It may reduce susceptibility artefacts on diffusion-weighted MR images, needed in case of reevaluation of rectal tumor after neoadjuvant chemoradiotherapy.
Vaginal and rectal opacification with ultrasound gel before MR imaging is an inexpensive, well tolerated procedure. While use of rectal opacification is widely recognized as necessary in evaluation of dynamic pelvic floor disease, use of rectal and/or vaginal opacification is a matter of debate. We believe from our experience that, as far as endometriosis is concerned, opacification may be beneficial particularly for small vaginal lesions, lesions infiltrating posterior vaginal fornix and anterior rectal wall, and that it enables less-experienced radiologists to better interpret deep endometriosis. Regarding cervical and endometrial cancer, endovaginal filling is useful when vaginal extension of the tumor is suspected. Development anomalies, such as vaginal septum, vaginal agenesis, as well as vaginal cysts are often better characterized and localized, when vaginal opacification is conducted. Finally, in the case of rectal tumor, we presume that rectal opacification may enable radiologists to measure distance from inferior pole of the tumor to the anal margin and to assess relationship of the tumor with the sphincter.
Figures and Tables
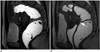 | Fig. 130-year-old woman with clinical suspicion of endometriosis (dysmenorrhea).T2-weighted MR sequences in sagittal plane with rectal opacification only (A), and after rectal and vaginal opacification (B). Endometriotic nodule revealing low signal intensity is more conspicuous after vaginal distension (arrow) (B) than before use of opacification. Vaginal lesions are ruled out. MR = magnetic resonance
|
 | Fig. 2Pelvic MRI study in 27-year-old female with endometriosis that presents dyspareunia.T2-weighted MR images with rectal and vaginal opacification in sagittal (A), coronal (B), and axial (C) planes. Thanks to vaginal distension, thin fibrous lesion in posterior vaginal fornix displaying low signal intensity on T2-weighted images (arrows) (A-C) and hemorrhagic microcyst displaying high signal intensity focus on fat-suppressed T1-weighted MR image (arrow) (D) are depicted. MRI = magnetic resonance imaging
|
 | Fig. 3Pre-operative MR images in 37-year-old patient with known endometriosis and suffering from recurrent dyschesia.Sagittal T2-weighted MR view with rectal opacification (A) revealing endometriotic nodule of anterior wall of rectum (*), surgically removed. MRI conducted after surgery using T2-weighted MR images after vaginal and rectal opacification in sagittal (B), axial (C), and coronal (D) planes demonstrates endometriotic nodule in lateral right vaginal fornix (arrows) (B-D). This lesion had not been detected on pre-operative MR imaging, probably because of absence of initial vaginal distension.
|
 | Fig. 4Pre-operative pelvic MR study in 28-year-old female with endometriosis presenting pain radiating to back.Sagittal T2-weighted MR image using vaginal and rectal opacification reveals thick lesion in posterior vaginal fornix and posterior cervix (arrow) (B). There is large nodular lesion infiltrating anterior rectal wall on axial T2-weighted MR image (arrow) (C), associated with Douglas cul-de-sac obliteration. Vaginal and rectal opacification clearly improve detection of these lesions compared to what was observed on MR image MRI study conducted without opacification (A).
|
 | Fig. 5Sagittal T2-weighted MR images without and after vaginal opacification in two women (respectively 41-year-old and 47-year-old) with cervical carcinoma.Relatively high signal-intensity tumor is observed in posterior cervix (arrow). Vaginal fornices appear to be invaded by mass in absence of vaginal distension (A). After vaginal opacification, borders of tumor are better observed, and no vaginal extension is depicted in second case (arrow) (B). Tumor′s boundaries are less conspicuous without opacification.
|
 | Fig. 645-year-old female with cervical tumor undergoing pretherapeutic MRI.Sagittal T2-weighted MR image reveals large cervical tumor (*). Vaginal opacification nicely delineates wellpreserved posterior vaginal wall (arrow).
|
 | Fig. 767-year-old female with endometrial carcinoma (*).Sagittal T2-weighted MR image reveals that vaginal opacification facilitates identification of absence of vaginal involvement (arrow) from mass related to endometrial carcinoma (*).
|
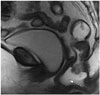 | Fig. 8Midsagittal T2-weighted MR image in 62-year-old patient with dyssynergic defecation.Distension of rectum simulates rectocele as rectal gel has not been completely evacuated during maximal straining (arrow).
|
 | Fig. 927-year-old woman suffering from infertility.
A. Coronal T2-weighted MR image with ultrasound gel vaginal opacification reveals septate vagina (arrow), outlined by high T2 signal intensity from ultrasound endovaginal gel. B, C. Axial T2-weighted MR images in same patient at different levels reveal complete septate uterus with septum displaying homogenous low signal T2 signal and extending from fundus to cervix (arrows).
|
 | Fig. 1025-year-old patient with story of recurrent spontaneous miscarriages.
A. Coronal T2-weighted MR image without opacification image reveals bicornuate uterus with significant fundal cleft (*). B. Coronal T2-weighted MR images obtained with endovaginal gel reveal incomplete vaginal septation (arrow), easily overlooked without opacification.
|
 | Fig. 1118-year-old female with Mayer-Rokitansky-Küster-Hauser syndrome.Sagittal T2-weighted MR image reveals absence of uterus. Vagina is not observed (arrow) (A). After opacification, on sagittal (B) and coronal (C) T2-weighted MR image, gel is not observed inside vagina (hypoplasic vagina), but underlines labiae (arrows). Ovaries are normal.
|
 | Fig. 1249-year-old woman complaining of mass in lower part of vagina.
A. Vaginal abnormalities are observed in sagittal T2-weighted MR images without vaginal opacification, but are difficult to analyze (arrow). B. After vaginal opacification was conducted subsequently, three cysts of anterior vaginal wall became much more conspicuous (arrows).
|
Table 1
Summarizing MRI Sequences and Use of Endovaginal/Rectal Filling for Each Disease, Both in Literature and in Our Experience (including Advantages)

References
2. Bitti GT, Argiolas GM, Ballicu N, Caddeo E, Cecconi M, Demurtas G, et al. Pelvic floor failure: MR imaging evaluation of anatomic and functional abnormalities. Radiographics. 2014; 34:429–448.

3. Marchiolè P, Cittadini G, Sala P, Moioli M, Mathevet P, Capaccio E, et al. Pre- and post-operative work-up in patients affected by early cervical cancer and eligible for fertilitysparing treatment: role of MRI with saline hydrocolpos. Abdom Imaging. 2010; 35:271–279.

4. Maccioni F. Functional disorders of the ano-rectal compartment of the pelvic floor: clinical and diagnostic value of dynamic MRI. Abdom Imaging. 2013; 38:930–951.

5. Hetzer FH, Andreisek G, Tsagari C, Sahrbacher U, Weishaupt D. MR defecography in patients with fecal incontinence: imaging findings and their effect on surgical management. Radiology. 2006; 240:449–457.

6. Reiner CS, Weishaupt D. Dynamic pelvic floor imaging: MRI techniques and imaging parameters. Abdom Imaging. 2013; 38:903–911.

7. Reiner CS, Tutuian R, Solopova AE, Pohl D, Marincek B, Weishaupt D. MR defecography in patients with dyssynergic defecation: spectrum of imaging findings and diagnostic value. Br J Radiol. 2011; 84:136–144.

8. Maas M, Lambregts DM, Lahaye MJ, Beets GL, Backes W, Vliegen RF, et al. T-staging of rectal cancer: accuracy of 3.0 Tesla MRI compared with 1.5 Tesla. Abdom Imaging. 2012; 37:475–481.
9. Ye F, Zhang H, Liang X, Ouyang H, Zhao X, Zhou C. Journal club: preoperative MRI evaluation of primary rectal cancer: intrasubject comparison with and without rectal distention. AJR Am J Roentgenol. 2016; 207:32–39.

10. Fiaschetti V, Crusco S, Meschini A, Cama V, Di Vito L, Marziali M, et al. Deeply infiltrating endometriosis: evaluation of retro-cervical space on MRI after vaginal opacification. Eur J Radiol. 2012; 81:3638–3645.

11. Chassang M, Novellas S, Bloch-Marcotte C, Delotte J, Toullalan O, Bongain A, et al. Utility of vaginal and rectal contrast medium in MRI for the detection of deep pelvic endometriosis. Eur Radiol. 2010; 20:1003–1010.

12. Novellas S, Marcotte Bloch C, Berthier F, Fournol M, Delotte J, Bongain A, et al. [Anatomy of the female pelvis on MRI: value of intravaginal contrast]. J Radiol. 2009; 90(7-8 Pt 1):819–824.
13. Bazot M, Gasner A, Lafont C, Ballester M, Dara E. Deep pelvic endometriosis: limited additional diagnostic value of postcontrast in comparison with conventional MR images. Eur J Radiol. 2011; 80:331–339.

14. Macario S, Chassang M, Novellas S, Baudin G, Delotte J, Toullalan O, et al. The value of pelvic MRI in the diagnosis of posterior cul-de-sac obliteration in cases of deep pelvic endometriosis. AJR Am J Roentgenol. 2012; 199:1410–1415.

15. Chami LP, Blasbalg R, Pereira RM, Warmbrand G, Serafini PC. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics. 2011; 31:77–100.

16. Takeuchi H, Kuwatsuru R, Kitade M, Sakurai A, Kikuchi I, Shimanuki H, et al. A novel technique using magnetic resonance imaging jelly for evaluation of rectovaginal endometriosis. Fertil Steril. 2005; 83:442–447.

17. Kikuchi I, Kuwatsuru R, Yamazaki K, Kumakiri J, Aoki Y, Takeda S. Evaluation of the usefulness of the MRI jelly method for diagnosing complete cul-de-sac obliteration. Biomed Res Int. 2014; 2014:437962.

18. Loubeyre P, Copercini M, Frossard JL, Wenger JM, Petignat P. Pictorial review: rectosigmoid endometriosis on MRI with gel opacification after rectosigmoid colon cleansing. Clin Imaging. 2012; 36:295–300.

19. Bazot M, Bharwani N, Huchon C, Kinkel K, Cunha TM, Guerra A, et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur Radiol. 2017; 27:2765–2775.

20. Coutinho A Jr, Bittencourt LK, Pires CE, Junqueira F, Lima CM, Coutinho E, et al. MR imaging in deep pelvic endometriosis: a pictorial essay. Radiographics. 2011; 31:549–567.

21. Brown MA, Mattrey RF, Stamato S, Sirlin CB. MRI of the female pelvis using vaginal gel. AJR Am J Roentgenol. 2005; 185:1221–1227.

22. El Sayed RF, Alt CD, Maccioni F, Meissnitzer M, Masselli G, Manganaro L, et al. Magnetic resonance imaging of pelvic floor dysfunction - joint recommendations of the ESUR and ESGAR pelvic floor working group. Eur Radiol. 2017; 27:2067–2085.

23. Colaiacomo MC, Masselli G, Polettini E, Lanciotti S, Casciani E, Bertini L, et al. Dynamic MR imaging of the pelvic floor: a pictorial review. Radiographics. 2009; 29:e35.

24. Khatri G, Bailey AA, Bacsu C, Christie AL, Kumar N, Pedrosa I, et al. Influence of rectal gel volume on defecation during dynamic pelvic floor magnetic resonance imaging. Clin Imaging. 2015; 39:1027–1031.

25. Francesca M, Najwa AA, Valeria B, Fabrizio M, Marileda I, Massimo M, et al. Prospective comparison between two different magnetic resonance defecography techniques for evaluating pelvic floor disorders: air-balloon versus gel for rectal filling. Eur Radiol. 2016; 26:1783–1791.

26. García del Salto L, de Miguel Criado J, Aguilera del Hoyo LF, Gutiérrez Velasco L, Fraga Rivas P, Manzano Paradela M, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014; 34:1417–1439.

27. Lienemann A, Anthuber C, Baron A, Kohz P, Reiser M. Dynamic MR colpocystorectography assessing pelvic-floor descent. Eur Radiol. 1997; 7:1309–1317.

28. Hoeffel C, Mulé S, Laurent V, Bouché O, Volet J, Soyer P. Primary rectal cancer local staging. Diagn Interv Imaging. 2014; 95:485–494.

29. Loubeyre P, Petignat P, Jacob S, Egger JF, Dubuisson JB, Wenger JM. Anatomic distribution of posterior deeply infiltrating endometriosis on MRI after vaginal and rectal gel opacification. AJR Am J Roentgenol. 2009; 192:1625–1631.

30. Hottat N, Larrousse C, Anaf V, Noël J-C, Matos C, Absil J, et al. Endometriosis: contribution of 3.0-T pelvic MR imaging in preoperative assessment--initial results. Radiology. 2009; 253:126–134.

31. Balleyguier C, Sala E, Da Cunha T, Bergman A, Brkljacic B, Danza F, et al. Staging of uterine cervical cancer with MRI: guidelines of the European Society of Urogenital Radiology. Eur Radiol. 2011; 21:1102–1110.

32. Akata D, Kerimoglu U, Hazirolan T, Karcaaltincaba M, Köse F, Ozmen MN, et al. Efficacy of transvaginal contrast-enhanced MRI in the early staging of cervical carcinoma. Eur Radiol. 2005; 15:1727–1733.

33. Young P, Daniel B, Sommer G, Kim B, Herfkens R. Intravaginal gel for staging of female pelvic cancers--preliminary report of safety, distention, and gel-mucosal contrast during magnetic resonance examination. J Comput Assist Tomogr. 2012; 36:253–256.

34. Mondot L, Novellas S, Senni M, Piche T, Dausse F, Caramella T, et al. Pelvic prolapse: static and dynamic MRI. Abdom Imaging. 2007; 32:775–783.

35. Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011; 17:761–771.

36. Troiano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology. 2004; 233:19–34.
37. Griffin N, Grant LA, Sala E. Magnetic resonance imaging of vaginal and vulval pathology. Eur Radiol. 2008; 18:1269–1280.

38. Yoo RE, Cho JY, Kim SY, Kim SH. A systematic approach to the magnetic resonance imaging-based differential diagnosis of congenital Müllerian duct anomalies and their mimics. Abdom Imaging. 2015; 40:192–206.

39. Beets-Tan RG, Lambregts DM, Maas M, Bipat S, Barbaro B, Caseiro-Alves F, et al. Magnetic resonance imaging for the clinical management of rectal cancer patients: recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2013; 23:2522–2531.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download