INTRODUCTION
MATERIALS AND METHODS
Study Population
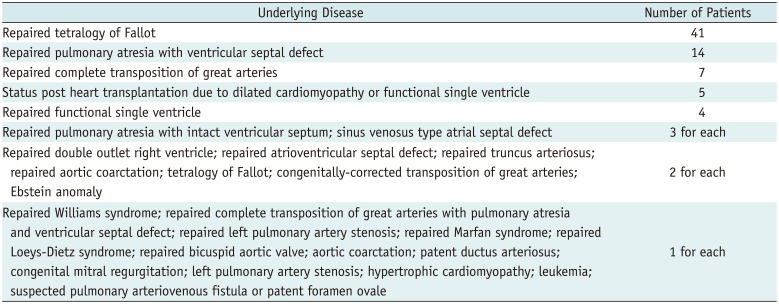
Table 1
Underlying Diseases of Study Population (n = 104)
Cardiothoracic CT Imaging
Tube Current Saturation
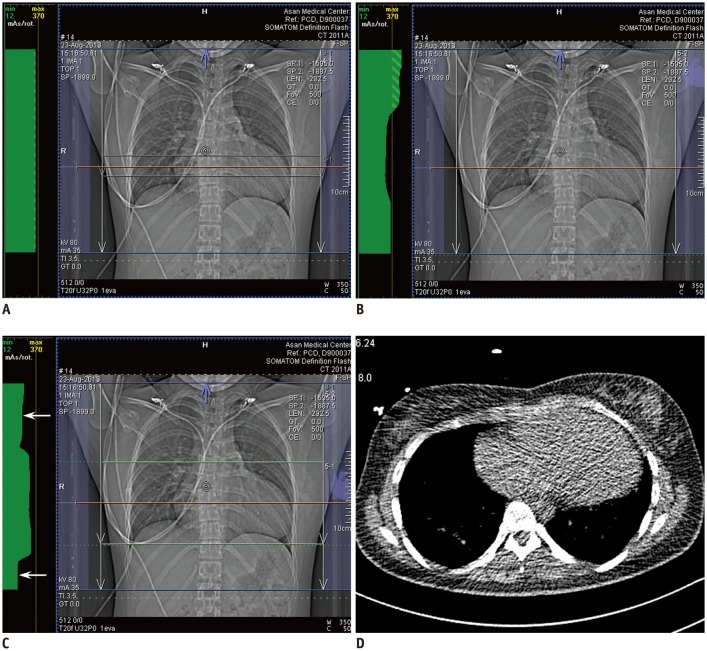 | Fig. 1Retrospectively ECG-gated spiral cardiothoracic CT using dual-source technique in 23-year-old woman with repaired tetralogy of Fallot.
A. Anteroposterior scout image of conventional CT protocol shows tube current modulation curve in green throughout whole longitudinal scan range indicating no tube current saturation. In other words, tube current time product per rotation remains below maximum value of 370 over entire scanning range. Of note, tube current modulation curve is flat on top indicating no change in tube current time product per rotation over whole scan range in this protocol. B. Anteroposterior scout image of uniphasic chest pain CT protocol demonstrates tube current modulation curve in green over whole longitudinal scan range. In contrast to conventional CT protocol (A), tube current time product per rotation is modulated in this protocol according to patient-specific attenuation information acquired from scout image. C. Anteroposterior scout image of biphasic chest pain CT protocol also displays tube current modulation curve in green over whole longitudinal scan range. In this protocol, cardiac region is defined by user as green dotted lines and radiation dose is subsequently reduced to half (arrows) in upper and lower parts of scan range outside cardiac region because one of two X-ray tubes in dual-source CT system is switched off in these regions. D. From axial CT image acquired at slice position (orange line in A–C) approximately 2.5 cm above liver dome for bolus tracking, cross sectional area and mean body density was measured as 597 mm2 and −147 Hounsfield unit, respectively, and optimal volume CT dose index for non-ECG-synchronized cardiothoracic CT was calculated as 3.8 mGy (for one slice) that was increased to 4.8 mGy (for whole scan range) after application of automatic tube current modulation. Axial CT image looks noisy because low radiation dose setting (80 kVp and 25 mA) was used to minimize patient radiation exposure. CT = computed tomography, ECG = electrocardiography
|
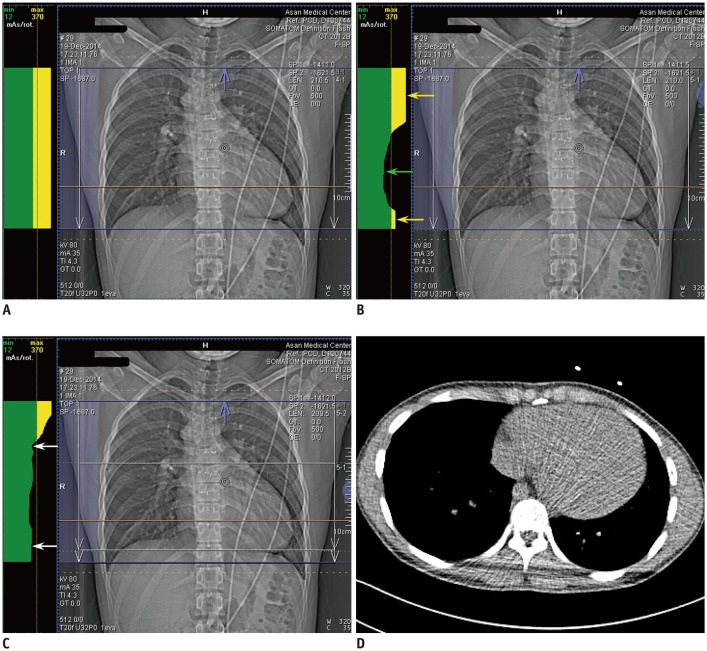 | Fig. 2Retrospectively ECG-gated spiral cardiothoracic CT using dual-source technique in 19-year-old man with repaired double-outlet right ventricle and subaortic ventricular septal defect.
A. Anteroposterior scout image of conventional CT protocol shows upper part of tube current modulation curve in yellow throughout whole longitudinal scan range indicating tube current saturation. It means that tube current time product per rotation exceeds maximum value of 370 over entire scanning range. Of note, tube current modulation curve is flat on top indicating no change in tube current time product per rotation over whole scan range in this protocol. B. Anteroposterior scout image of uniphasic chest pain CT protocol demonstrates upper part of tube current modulation curve in yellow in upper thorax (yellow arrow) and lower thorax (yellow arrow) exceeding maximum tube current time product per rotation of 370. In contrast, tube current time product per rotation is modulated below maximum value of 370 in cardiac region (green arrow). C. Anteroposterior scout image of biphasic chest pain CT protocol shows that tube current time product per rotation is reduced (arrows) in upper and lower parts of scan range outside cardiac region defined by user as green dotted lines. Nonetheless, yellow tube current saturation is still shown in upper thorax. D. From axial CT image acquired at slice position (orange line in A–C) approximately 2.0 cm above liver dome for bolus tracking, cross sectional area and mean body density was measured as 522 mm2 and −240 Hounsfield unit, respectively, and optimal volume CT dose index for non-ECG-synchronized cardiothoracic CT was calculated as 2.8 mGy (for one slice) that was increased to 5.1 mGy (for whole scan range) after application of automatic tube current modulation. Axial CT image looks noisy because low radiation dose setting (80 kVp and 25 mA) was used to minimize patient radiation exposure.
|
Statistical Analysis
RESULTS
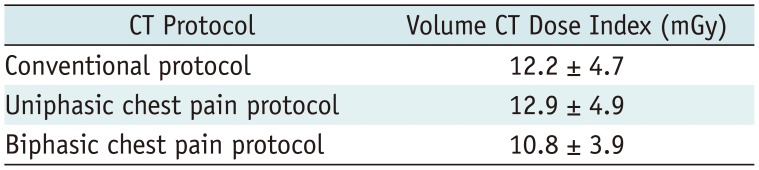
Table 3
Differences in Volume CT Dose Index Values between Biphasic Chest Pain and Other CT Protocols in Groups with and without Tube Current Saturation
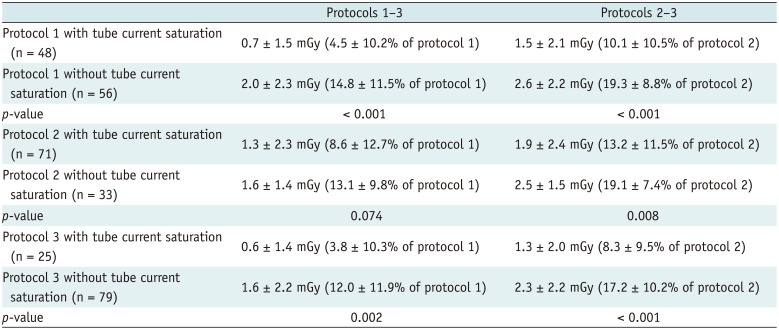
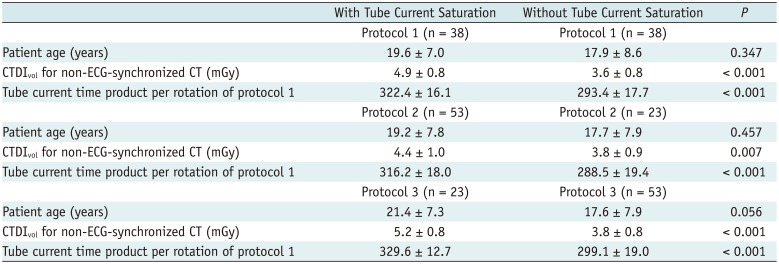
Table 4
Comparisons of Patient Age, Volume CT Dose Index Value based on Cross Sectional Area and Mean Body Density, Tube Current Time Product per Rotation of Conventional Protocol between Groups with and without Tube Current Saturation in 76 Patients Using 100 kVp




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download