INTRODUCTION
A ruptured functional ovarian cyst is a frequent cause of acute pelvic pain in women of reproductive age. The disease course varies from no symptoms or signs to severe peritoneal irritations and even life-threatening shock (
1). Therefore, even though ovarian cyst rupture is a type of physiologic event and is self-limiting with conservative management, it occasionally requires surgical intervention when accompanied by hemodynamic instability, severe persistent pain, diagnostic uncertainty, or large amount of hemoperitoneum (
23). Although any functional ovarian cyst can present as a hemorrhage or rupture, the increased vascularity of the ovary in the luteal phase may increase the risk of rupture and bleeding of the corpus luteal cyst (
2). Although several previous studies have reported a rate of surgery for ruptured corpus luteal cysts with hemoperitoneum as high as 80% (
24), conservative management is usually performed with analgesia and close observation in actual clinical settings, which is supported by recent advances in imaging studies that allow an early and accurate diagnosis (
2356). Because surgery (ovarian cystectomy) is still an invasive procedure and postoperative scarring can be a cosmetic problem for patients, the appropriate identification of patients who need surgical treatment is important.
The evaluations of image findings of ruptured corpus luteal cysts using ultrasonography (
7) or computed tomography (CT) (
6) have been reported; however, the correlation between image findings with final clinical outcomes (surgery vs. conservative management) remains unclear. A recent retrospective study analyzed the risk factors for surgery to treat a corpus luteal cyst rupture among multiple clinical and CT findings; however, the diameter of the ovarian cyst and the depth of hemoperitoneum were the only CT findings analyzed (
5).
Therefore, the purpose of our study was to evaluate the pretreatment CT findings that are potential risk factors for surgical treatment for patients who are suffering from corpus luteal cyst rupture with hemoperitoneum.
Go to :

MATERIALS AND METHODS
This retrospective, single-institution study was approved by our Institutional Review Board and Ethics Committee. Informed consent was waived because of the retrospective nature of the study.
Study Population
For inclusion in the study, the patients were selected from the electronic medical record system of our hospital using the diagnosis-based searching engine in the system. From January 2009 to December 2014, a total of 284 patients who visited our emergency department and had a diagnosis that included ‘hemoperitoneum’ and/or ‘corpus luteal cyst’ were identified by the search engine.
One investigator reviewed the medical records of the initially selected patients and excluded the patients who were diagnosed with hemoperitoneum from causes other than corpus luteal cyst rupture (e.g., trauma, endometriosis or bleeding after ovum pick-up for in-vitro fertilization); an unruptured (incidentally found) corpus luteal cyst; or no CT scan, including 7 patients who underwent CT without a precontrast image and 2 patients whose CT images were lost due to a picture archiving and communication system (PACS) storage error. One patient, who had acute appendicitis and underwent removal of suspicious ruptured ovarian cyst during appendectomy, was also excluded because the decision for treatment strategy of the ruptured ovarian cyst was interrupted by the appendicitis, which required surgical treatment. Finally, 106 female patients who were diagnosed with a ruptured ovarian cyst with hemoperitoneum were included (mean age, 26.1 years; range, 17–44 years). The diagnosis of ruptured ovarian cyst with hemoperitoneum was based on clinical symptoms, physical examinations by the emergency physician and gynecologist, and image findings of ultrasound and CT. No patients in the final study population were on anticoagulation therapy or had a positive b-hCG test.
The researchers divided the study population into surgically treated and conservatively managed groups. Clinical parameters and imaging findings of the two groups were compared. In our institute, conservative management is the first choice of treatment for corpus luteal cyst rupture with hemoperitoneum, and the gynecologists determine whether surgical intervention is needed; usual indications of surgical treatment include unstable vital signs, significant hemoglobin decrease or hemoperitoneum increase, and severe or persistent abdominal pain despite the use of analgesics (
5).
CT Protocol
Of the 106 patients in the study, 96 underwent abdominal CT scans using a 16-detector CT scanner (LightSpeed Pro, GE Healthcare, Milwaukee, WI, USA). The CT protocol for acute abdomen in our institution consisted of standardized two-phase CT scans, including precontrast and portal venous phases.
After precontrast images were obtained from the diaphragmatic dome to the symphysis pubis, low-osmolar nonionic iodine contrast media (iohexol, Omnihexol 350, Korea United Pharm Inc., Seoul, Korea) was intravenously administered in a volume of 2 mL/kg using a power injector (Optivantage DH, Mallinckrodt Imaging Solutions, Hazelwood, MO, USA) at a rate of 3 mL/s. The scanning delay for the portal venous phase was 90 seconds after initiation of the contrast material injection. The scan range of the portal venous phase was the same as the precontrast scan.
The detailed parameters were as follows: detector configuration, 16 × 1.25 mm; tube voltage, 120 kVp; noise index, 12.35 with automatic exposure control (smart mA, GE Healthcare, Milwaukee, WI, USA); gantry rotation period, 0.6 second; pitch factor, 1.375; table speed, 27.5 mm per rotation; reconstructed section width, 3.75 mm; and reconstructed section interval, 3.75 mm.
Ten patients visited our emergency department via another hospital; and had undergone CT elsewhere. We included those cases if the CT met the following criteria: taken using multidetector CT; including at a minimum precontrast, and the portal venous phase covering the liver dome to symphysis pubis; and saved as a DICOM file for PACS. All 10 cases met the aforementioned criteria and were included in our study.
Image Analysis
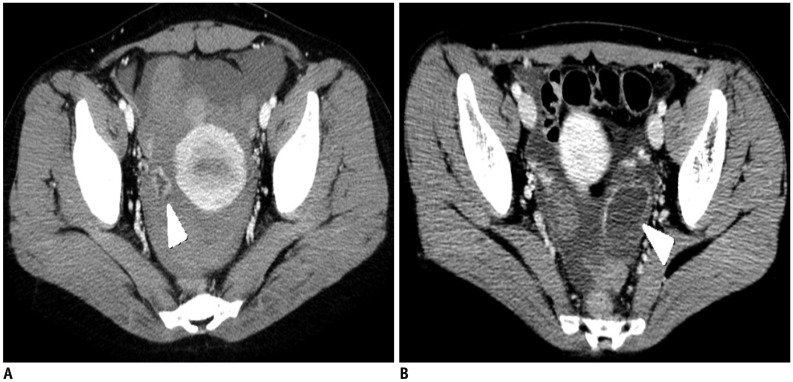
CT images were reviewed and evaluated in consensus by two genitourinary radiologists (with 2 years of experience and with 12 years of experience in genitourinary radiology) using PACS software (Maroview 5.4, Infinitt, Seoul, Korea). The CT findings for analysis were as follows: cyst size, cyst shape (shrunken vs. maintained) (
Fig. 1), sentinel clot sign, ring of fire sign, depth of the hemoperitoneum, active bleeding in the portal phase, attenuation of the hemoperitoneum on the precontrast scan, attenuation of the hemoperitoneum on the portal phase scan, and attenuation difference of the hemoperitoneum between the precontrast and portal phase scans. The size of the cyst was measured along its major axis. The positive sentinel clot sign was determined as focal high-density clotted blood around the ovarian cyst on the precontrast CT scan (
Fig. 2) (
8). The ring of fire sign, which originated from the color Doppler ultrasonographic finding of a corpus luteal cyst as an increased cyst wall flow, was determined as a more prominent enhancement of the possibly involved cyst wall, with visual comparison of the myometrium as an internal reference (
Fig. 3) (
9). The depth of the hemoperitoneum was measured at the deepest pocket in the pelvic cavity on an axial scan. A single investigator measured the attenuation of hemoperitoneum by placing a round region of interest in the center of high-attenuated pelvic fluid on the precontrast image, taking care not to locate the cursor on the beam-hardening artifact. Hemoperitoneum was determined as > 30 Hounsfield unit. Active bleeding in the portal venous phase (AB_PVP) was determined as the presence of visualized contrast media extravasation on the CT scan (
Fig. 4).
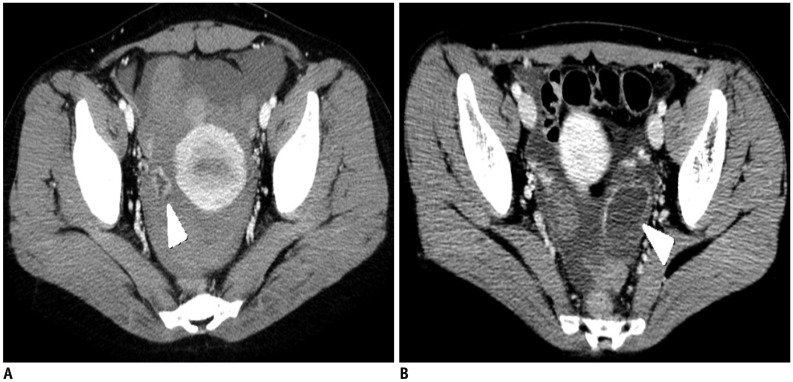 | Fig. 1Sample image of shrunken (A) and tensile (B) shape cysts (arrowheads).
|
 | Fig. 2Sample image of sentinel clot, which was determined as focal high-density clotted blood around ovarian cyst on precontrast CT (arrowhead).
|
 | Fig. 3
Sample image of ring of fire sign (arrowhead).
Involved cyst also showed tensile contour.

|
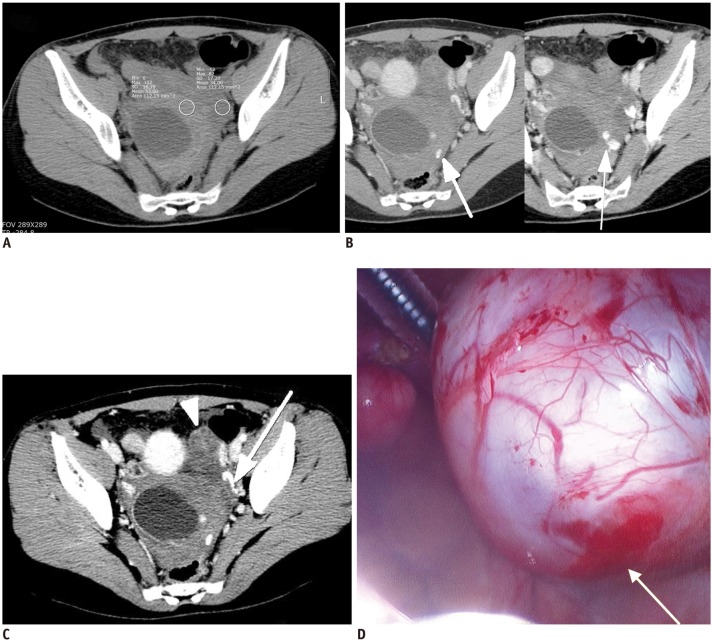
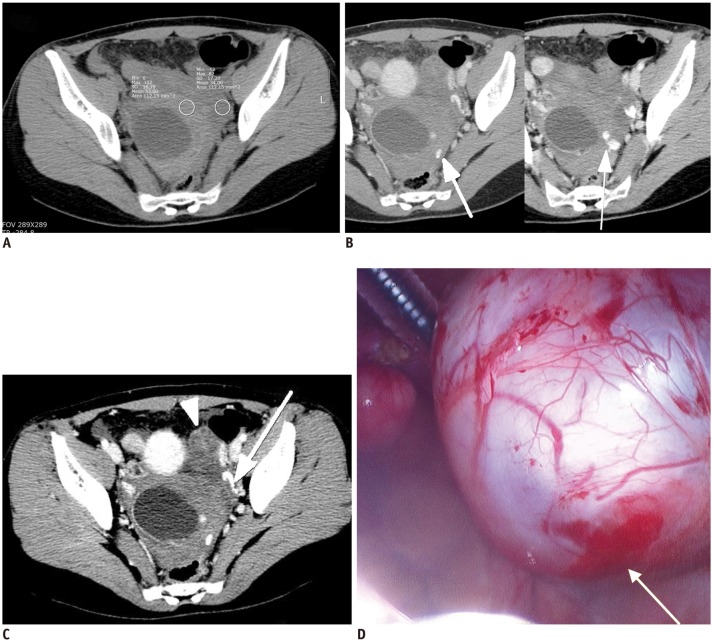 | Fig. 4
26-year-old female patient visited emergency room with acute lower abdominal pain.
Patient had coitus 3 hours before symptom development.
A. Precontrast CT scan showed cystic mass and hemoperitoneum (34–53 HU) in pelvic cavity. B, C. Contrast media extravasation suggestive of active bleeding (arrows) adjacent to cystic mass was detected on portal venous phase axial scans. Two consecutive images confirmed curvilinear lesion as contrast media extravasation, and not dilated paraovarian vein in (B). Left ovary was well-demarcated and intact without active bleeding (arrowhead). D. Patient was surgically treated with right ovarian cystectomy and hematoma evacuation, and active bleeding focus was observed at right ovary (arrow), based on operation record. HU = Hounsfield unit

|
Statistical Analysis
Each CT finding was compared between the surgically treated and conservatively managed groups using the Mann-Whitney U-Test for continuous numeric data or chi-square test for binary categorical data. Multivariable stepwise logistic regression analysis with backward elimination was then performed to evaluate the adjusted odds ratio (ORs) for the CT findings, which was confirmed as statistically significant on previously performed univariable analyses. Variables with a
p value < 0.05 based on the Mann-Whitney U-Test or chi-square test were used as input variables for the multivariable stepwise logistic regression analysis, and the removal of variables was based on likelihood ratio statistics with a probability of 0.10. Receiver-operating characteristic (ROC) curve analysis for consecutive variables, which were determined as statistically significant findings on the multivariable logistic regression, was performed to evaluate the diagnostic performance and cut-off value. The depth of hemoperitoneum showed statistical significance in the comparative study and univariable logistic regression analysis, ROC curve was obtained for hemoperitoneum depth using surgery as the endpoint. Finally, based on the result of the ROC analysis, the OR of cases with both a hemoperitoneum depth > 5.8 cm and a positive AB_PVP was calculated. All data analyses, except the ROC analysis, were performed using commercial statistics software (SPSS ver. 20.0, SPSS Inc., Chicago, IL, USA). The ROC analysis with curve fitting was performed with the JROCFIT and JLAPROC4 web-based calculators (John Eng, Johns Hopkins University;
http://www.jrocfit.org), which are direct JAVA translations of the ROCFIT and LABROC4 programs developed by the late Charles Metz and colleagues at the University of Chicago.
Go to :

RESULTS
The rate of surgical treatment was 17.9% (n = 19) and that of conservative management was 82.1% (n = 87).
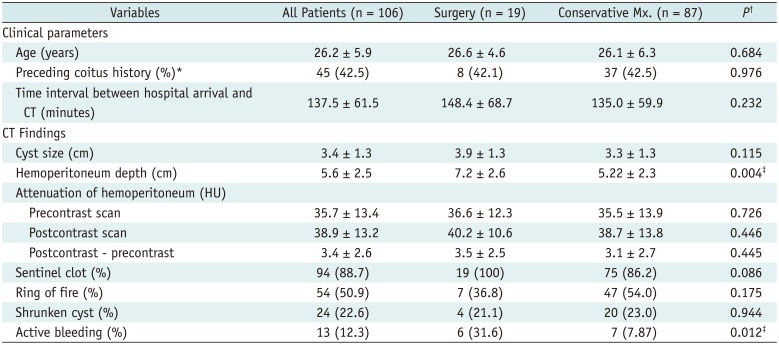
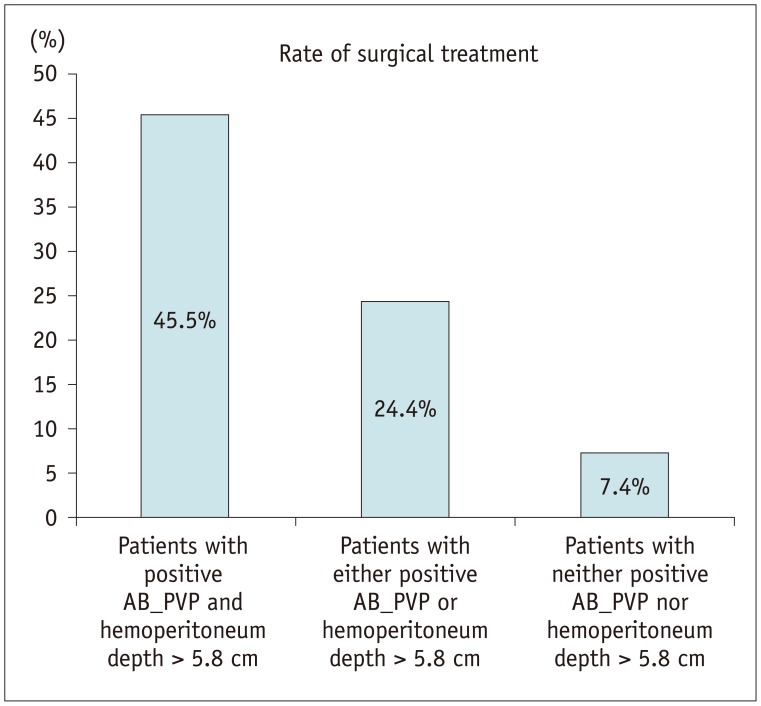
Table 1 summarizes the comparative result of the CT findings between the surgery and conservative management groups. The mean age, preceeding coitus history, and the time interval between hospital arrival and CT study showed no significant differences between the surgery and conservative management groups.
Table 1
Comparative Results of Clinical Parameters and CT Findings between Surgical Treatment Group and Conservative Management Group
|
Variables |
All Patients (n = 106) |
Surgery (n = 19) |
Conservative Mx. (n = 87) |
P†
|
|
Clinical parameters |
|
|
|
|
|
Age (years) |
26.2 ± 5.9 |
26.6 ± 4.6 |
26.1 ± 6.3 |
0.684 |
|
Preceding coitus history (%)*
|
45 (42.5) |
8 (42.1) |
37 (42.5) |
0.976 |
|
Time interval between hospital arrival and CT (minutes) |
137.5 ± 61.5 |
148.4 ± 68.7 |
135.0 ± 59.9 |
0.232 |
|
CT Findings |
|
|
|
|
|
Cyst size (cm) |
3.4 ± 1.3 |
3.9 ± 1.3 |
3.3 ± 1.3 |
0.115 |
|
Hemoperitoneum depth (cm) |
5.6 ± 2.5 |
7.2 ± 2.6 |
5.22 ± 2.3 |
0.004‡
|
|
Attenuation of hemoperitoneum (HU) |
|
|
|
|
|
Precontrast scan |
35.7 ± 13.4 |
36.6 ± 12.3 |
35.5 ± 13.9 |
0.726 |
|
Postcontrast scan |
38.9 ± 13.2 |
40.2 ± 10.6 |
38.7 ± 13.8 |
0.446 |
|
Postcontrast - precontrast |
3.4 ± 2.6 |
3.5 ± 2.5 |
3.1 ± 2.7 |
0.445 |
|
Sentinel clot (%) |
94 (88.7) |
19 (100) |
75 (86.2) |
0.086 |
|
Ring of fire (%) |
54 (50.9) |
7 (36.8) |
47 (54.0) |
0.175 |
|
Shrunken cyst (%) |
24 (22.6) |
4 (21.1) |
20 (23.0) |
0.944 |
|
Active bleeding (%) |
13 (12.3) |
6 (31.6) |
7 (7.87) |
0.012‡
|

The depth of hemoperitoneum on the axial scan and positive AB_PVP showed statistical significance (< 0.05) between the surgery and conservative management groups in the comparative study. There were no significant differences in age, coitus history within 24 hours, cyst size, cyst shape (shrunken vs. maintained), presence of sentinel clot sign, presence of ring of fire sign, and attenuation/attenuation difference of the hemoperitoneum between the two treatment groups.
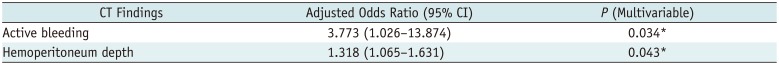
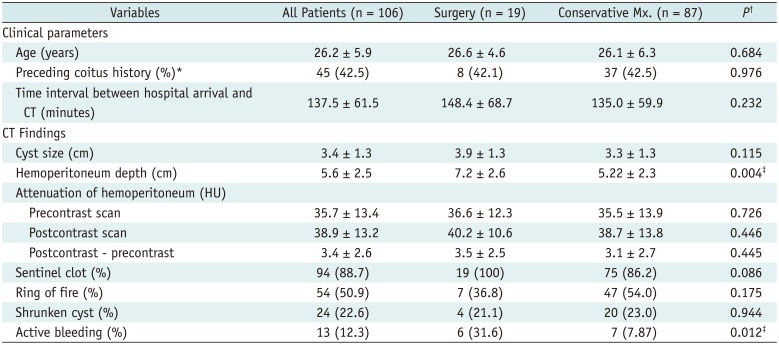
Multivariable logistic regression analysis revealed that both the presence of AB_PVP and hemoperitoneum depth were significant predictors of surgical intervention for ruptured ovarian cyst patients, with adjusted ORs of 3.773 and 1.318, respectively (
Table 2).
Table 2
Logistic Regression Results for Predicting Necessity of Surgical Treatment for Patients with Ruptured Ovarian Cyst with Hemoperitoneum by Each Pretreatment CT Finding
|
CT Findings |
Adjusted Odds Ratio (95% CI) |
P (Multivariable) |
|
Active bleeding |
3.773 (1.026–13.874) |
0.034*
|
|
Hemoperitoneum depth |
1.318 (1.065–1.631) |
0.043*
|

The Az value of 0.711 for hemoperitoneum depth using surgery as the endpoint indicated fair diagnostic performance. The optimal cut-off value of the hemoperitoneum depth was 5.8 cm with 75.0% sensitivity and 58.6% specificity (
Fig. 5).
 | Fig. 5
ROC analysis for hemoperitoneum depth.
Area under curve value was 0.711 (p = 0.004). Optimal cut-off value was 5.8 cm with 75.0% sensitivity and 58.6% specificity. Cut-off value for 95% specificity was 8.75 cm. ROC = receiver-operating characteristic

|
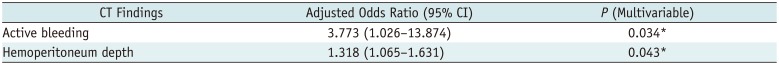
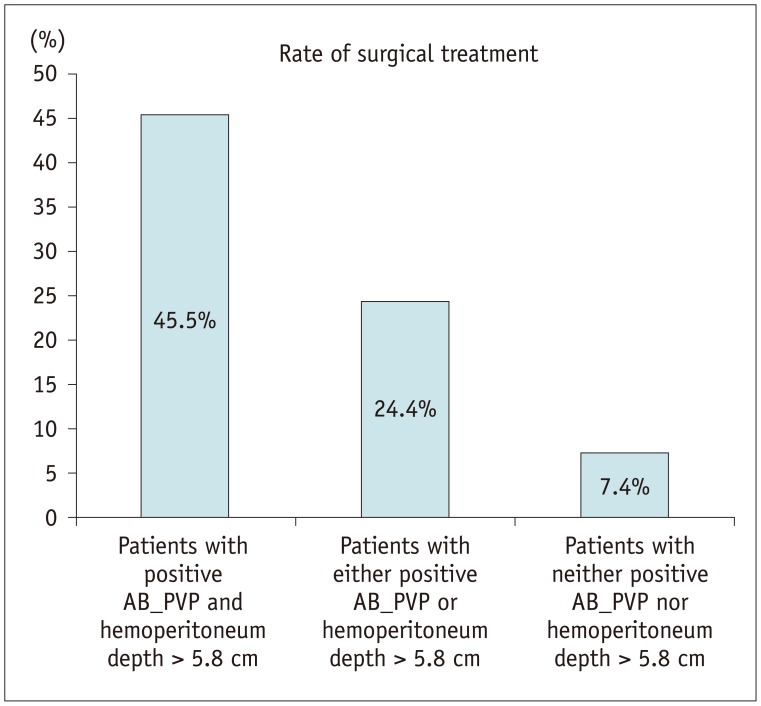
The patients who had both a hemoperitoneum depth > 5.8 cm and a positive AB_PVP had a 5.8 times higher rate of surgical intervention in the logistic regression analysis (
p = 0.019). The rate of surgical treatment was 45.5% in patients having both a positive AB_PVP and a hemoperitoneum depth > 5.8 cm (5/11 patients), 24.4% in those having either a positive AB_PVP or a hemoperitoneum depth > 5.8 cm (10/41 patients), and only 7.4% in those with neither a positive AB_PVP nor a hemoperitoneum depth > 5.8 cm (4/54 patients) (
p = 0.001, chi-square for trend) (
Fig. 6).
 | Fig. 6
Rate of surgical treatment based on coexistent CT predictors.
AB_PVP = active bleeding in the portal venous phase.

|
Go to :

DISCUSSION
In this study, we described the CT findings of corpus luteal cyst ruptures and determined pretreatment CT findings that are potential risk factors for surgical treatment of a ruptured corpus luteal cyst with hemoperitoneum. Positive AB_PVP and hemoperitoneum depth were determined as significant CT findings of risk factors for surgical treatment.
First, we delineated the CT findings of ruptured corpus luteal cysts from our results. The average cyst size was 3.4 cm. Twenty-four cases of ruptured corpus luteal cysts showed a shrunken shape (22.6%), which was unlike the findings of a previous study (
9) that described crenulation of the cyst wall in all investigated corpus luteal cysts.
In our study, 54 cases showed a ring of fire sign on the CT scan (50.9%). As mentioned previously, we used the term “ring of fire sign” when the cyst wall showed strong enhancement on the CT, similar to the original ring of fire sign on Doppler sonography. A previous study on the features of a ruptured corpus luteal cyst (
6) determined that all 6 cases of ruptured corpus luteal cysts showed strong wall enhancement and hemoperitoneum. Another study on the CT findings of uncomplicated corpus luteal cysts (
9), found that 6 of 10 cases (60%) showed a ring of fire sign on a CT scan. Collectively, these studies may indicate that the ring of fire sign on a CT scan would be observed in approximately half of all cases with corpus luteal cyst rupture.
A sentinel clot sign, which correlates with the high attenuated cyst content described in the previous study (
6), was found in 88.7% (94 of 106) of our cases and in 83% (5 of 6) of cases in the previous study (
6). As the sentinel clot sign is well known as a useful CT sign for evaluating probable anatomic sites of hemorrhage (
10), it could be regarded as one of the CT findings for a ruptured corpus luteal cyst.
In our study, 13 cases of AB_PVP were identified (12.3%). Several studies have reported active bleeding, which appears as contrast media extravasation on CT in corpus luteal cyst ruptures (
1011); however, to our best knowledge, we are the first to report the percentage of patients with active bleeding shown on CT from a ruptured corpus luteum.
Operative findings of ruptured corpus luteal cysts often reveal that the rupture involved the arteriole of the ovary, which produces active bleeding with resultant hemoperitoneum (
112). Therefore, active bleeding detected on a CT scan is suggestive of ruptured corpus luteal cyst. However, the positive active bleeding of a corpus luteal cyst rupture on CT and its relationship with surgical treatment have not been described previously. In our study, a positive AB_PVP on CT was the most significant risk factor for surgical treatment, with an adjusted OR of 3.773. We evaluated the presence of active bleeding in the portal phase, although active bleeding is reported to be most clearly observed in the arterial phase. However, a study for optimizing the CT protocol for blunt splenic injury revealed that a portal phase scan can visualize active bleeding more sensitively and accurately than an arterial phase scan; and pseudoaneurysm has higher sensitivity of detection in the arterial phase (
13). Active bleeding may appear on portal venous phase images after a negative arterial phase scan because of intermittent hemorrhage, a venous source of bleeding, or as a reflection of decreased perfusion related to cardiovascular insufficiency, vasospasm, or hypotension; in addition, the decreasing gantry rotation time of current multidetector CTs may affect the negative arterial phase scan for active bleeding by reducing effective sampling time and outrunning contrast media circulation time (
13). The amount of bleeding from a corpus luteal cyst rupture could be less than splenic bleeding, and the contrast media arrival time to cyst arteriole could be longer than the splenic artery; therefore, it is reasonable to evaluate active bleeding with a portal phase scan.
In the current study, the depth of hemoperitoneum was a significant CT risk factor, with an adjusted OR of 1.318. In a recent study (
5) that determined the risk factors for surgical treatment for ovarian cyst rupture, the total pelvic fluid collection depth on a CT scan (TFCD_CT) showed a significant difference between the surgery and conservative management groups and was confirmed as a significant risk factor for surgery, with an OR of 1.59. The ORs in the aforementioned study and our study were similar, and the optimal cut-off values from the ROC analysis for surgical treatment were almost the same (5.6 cm in the previous study and 5.8 cm in our study). In addition, the previous study (
5) defined TFCD_CT as the sum of the depths in the anterior and posterior cul-de-sac; whereas, we defined the depth of hemoperitoneum as the deepest pocket in the pelvic cavity on an axial scan. We evaluated hemoperitoneum depth by a one-step measurement method, which is more convenient than summing the depths of the anterior and posterior cul-de-sac. This method could be beneficial to clinicians who interpret the CT images of patients with corpus luteal cyst rupture.
In our study, the patients who had both a positive AB_PVP and a hemoperitoneum > 5.8 cm showed a surgery rate of 45.5%, and the rate decreased in patients who had only one or none of these risk factors. This result is similar to the result of a previous study (
5), which used TFCD_CT and diastolic blood pressure (dBP) as the two major risk factors. These similar trends of rate indicate that AB_PVP might represent dBP and concurrent significant bleeding, which is supported by our result of a high OR (5.786) for surgical treatment in patients with a hemoperitoneum depth > 5.8 cm as well as a positive AB_PVP.
Regarding the sentinel clot sign, it is likely that sentinel clots decelerate active bleeding by sealing cyst wall defects and, consequently, lower the risk of surgical intervention. The CT ring of fire sign was expected to have an association with bleeding when rupture occurs. However, these two parameters did not show significant differences between the surgically treated and conservatively managed groups, and they also failed to reveal statistical significance as risk factors for surgical treatment.
Our study has several limitations. First, the diagnosis of ruptured corpus luteal cyst in the conservative management group was based on medical imaging and clinical presentation and was therefore, not confirmative. Moreover, currently, there is no gold standard for surgical treatment of a ruptured corpus luteal cyst. In our center, we consider hemodynamic status, diagnostic uncertainty, persistent pain, and increasing hemoperitoneum as indications of surgery, as previously suggested (
3); however, the lack of a widely accepted official gold standard could be a major limitation. Moreover, the time interval between patient's onset of symptoms and CT study could not be evaluated, due to lack of complete description in the medical record. As a result, the patients who did not show active bleeding on CT simply presented themselves later in the disease course (i.e., after the bleeding had stopped or tamponade). The time interval between hospital arrival and CT study was used as a substitute, based on the expectation that the patients visited the emergency department as soon as possible after symptom onset. This could reflect the time delay in clinical process, which can also affect the CT visualization of bleeding and the amount of hemoperitoneum. Finally, this study was a single-institute retrospective study, and a prospective multicenter study with a larger population is required to validate our results.
In conclusion, the pretreatment CT scan for ruptured corpus luteal cysts can suggest the necessity of surgical treatment based on image findings. The presence of AB_PVP and the greatest depth of hemoperitoneum on the axial plane are potential risk factors for surgery in patients with a ruptured corpus luteal cyst with hemoperitoneum.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download