Abstract
Objective
Knowing the origin of the inferior phrenic artery (IPA) is important prior to surgical interventions and interventional radiological procedures related to IPA. We aimed to identify variations in the origin of IPA and to investigate the relationship between the origin of IPA and celiac axis variations using computed tomography angiography (CTA).
Materials and Methods
The CTA images of 1000 patients (737 male and 263 female, the mean age 60, range 18–94 years) were reviewed in an analysis of IPA and celiac axis variations. The origin of IPA was divided into two groups, those originating as a common trunk and those originating independently without a truncus. The relationship between the origin of IPA and celiac axis variation was analyzed using Pearson's chi-square test.
Results
Both IPAs originated from a common trunk in 295 (29.5%) patients. From which the majority of the common trunk originated from the aorta. Contrastingly, the inferior phrenic arteries originated from different origins in 705 (70.5%) patients. The majority of the right inferior phrenic artery (RIPA) and the left inferior phrenic artery (LIPA) originated independently from the celiac axis. Variation in the celiac axis were detected in 110 (11%) patients. The origin of IPA was found to be significantly different in the presence of celiac axis variation.
Inferior phrenic arteries (IPA) are double arteries which give off small branches to the diaphragm, liver, adrenal glands, esophagus, stomach, inferior vena cava, and retroperitoneum. The right inferior phrenic artery 344(RIPA) and the left inferior phrenic artery (LIPA) generally originate from the aorta or celiac axis independently or as a common trunk (1). However, they may show variations in their origins.
Knowing the anatomy and variations of the IPA is important prior to surgical interventions and interventional radiological procedures related to IPA. The most commonly recognized clinical feature of the IPA is that it may provide a extrahepatic collateral arterial supply to hepatocellular carcinomas (HCC), especially those located in the peripheral segments of liver (1234). It is also necessary to be familiar with the anatomy of the IPA in surgical and traumatic vascular injuries, hemoptysis, especially due to pulmonary pathologies located in the lung base, and gastroesophageal hemorrhage from the gastroesophageal junction (15678910).
Although the origin of the IPA can be evaluated on a CT angiography (CTA), the movement artifacts and the calcified atherosclerotic plaques of aorta and celiac axis may sometimes preclude recognition of the exact origin (111). In such cases, knowing the frequency of IPA variations and their probable relation to the celiac axis variations help estimate the IPA origin for interventional procedures. In this study, we aimed to identify variations in the origin of IPA and to investigate the relation between IPA origin and celiac axis variations using CTA.
The Institutional Review Board approved this study and waived informed consent. Abdomen CTA images of 1190 patients, obtained between January 2010 and January 2014, were reviewed retrospectively in terms of their anatomy and variations of IPA and celiac axis orientation. Assessed CTA images included those from the following, mesenteric ischemia, peripheral arterial disease, donor patients for renal transplantation, renal artery stenosis and aortic aneurysms. Patients with known liver disease, HCC with prior transarterial chemoembolization (TACE), surgery or endovascular treatment of aorta were excluded from the study. CTA images in patients who had severe atherosclerosis or occlusion of the aorta and celiac axis, those who had occlusion of one of the IPAs, and those with movement artifacts preventing assessment of the IPA and celiac axis variations, were also excluded from the study. After exclusion, 1000 patients (737 male and 263 female; the mean age, 60 years; range, 18–94 years) were enrolled into the study (Fig. 1).
All CT examinations were performed by a 64-slice CT scanner (Aquilion 64; Toshiba Medical Systems, Tochigi, Japan). For venous access, an upper extremity vein (antecubital vein of the right arm) and a 20-gauge intravenous cannula was used. A total of 80–85 mL of contrast media with high iodine concentration (370–400 mg/mL) was injected with a flow rate of 4–5 mL/s, followed by a 40–60 mL saline chaser. The scanning parameters included 120 kV, 225 mA, a section thickness of 0.5 mm, and a reconstruction interval of 0.5 mm. The scan revolution time was 0.4 seconds. Data for CTA was obtained through utilisation of a caudocranial direction.
All multidetector CTA data was transferred from the archive to a workstation (Aquarius workstation; TeraRecon, San Mateo, CA, USA), via internal network connections, providing three-dimensional post-processing options, and multi-planar image reformatting and maximum intensity projections. All examinations were reviewed by two radiologists (a final-year radiology resident and a radiologist with 8 years of experience) independently with respect to the anatomy of the IPA and celiac axis. In cases of discrepancy, the CTA images were reviewed again to reach a consensus on all variations. The origin of the IPA was assessed and classified in order to describe the results of analyses.
The relationship between variations of IPA origin and celiac axis were compared using Pearson's chi-square test. Classification was performed dependent on the cases in which celiac axis variation was present or absent, and statistical differences were evaluated between those groups in terms of IPA origin.
Inferior phrenic arteries were divided into two groups, those originating from a common trunk and those originating from different origins independently without a truncus.
Inferior phrenic arteries had a common trunk in their origin in 295 (29.5%) patients. The truncus originated from the aorta, celiac artery, renal artery and the left gastric artery, in descending order (Figs. 2, 3). The RIPA and the LIPA originated from different sources in 705 (70.5%) patients (Figs. 4, 5). IPA origin was consistently between the diaphragm and renal arteries in all patients. In patients with IPA originating from the aorta, the origin was the anterior, lateral or back of the aorta (Fig. 6). All IPA origins showed close proximity to celiac artery, renal arteries, and superior mesenteric artery. All IPAs originated from the celiac artery, renal arteries and the left gastric artery was determined to be located approximately 2 cm from the arteries. In patients with multiple renal arteries, IPA was detected to arise from the upper renal artery (Fig. 7).
The least frequently detected IPA variations were those with LIPA originating from the right renal artery, LIPA originating from the left hepatic artery, and RIPA originating from the common hepatic artery. Each variation was found only in one individual patient.
Celiac axis variations were organized according to a recent classification system (12). A total of 890 patients (89%) had classical anatomy and showed trifurcation in the celiac axis. Celiac axis variations were detected in 110 (11%) patients. Among patients with celiac axis variations, 54 (5.4%) had a hepato-splenic truncus, 28 (2.8%) had a gastro-splenic truncus, 3 (0.3%) had a hepato-splenic-mesenteric truncus, 1 (0.1%) had a hepatogastric truncus, 1 (0.1%) had a celiac-mesenteric truncus, 1 (0.1%) had no celiac truncus while other patients, 22 (2.2%), were placed in an unclassified group.
Tables 1 and 2 demonstrate the distribution of IPA origin in patients with and without celiac axis variation. The frequencies and percentages of IPA origin in patients with and without celiac axis variation are shown in Tables 3, 4, 5. In cases where IPA originated from a common trunk, RIPA and LIPA were found to be significantly different in patients with celiac axis variation (χ2p = 6.447, p = 0.039; χ2p = 6.451, p = 0.036; and χ2p = 81.035, p = 0.000, respectively) (Fig. 8).
We assessed variations of the IPA and celiac axis in 1000 patients using CTA and found that the majority of IPA originated from the aorta in patients with a common IPA trunk, while RIPA and LIPA originated the most from the celiac axis in patients without a common IPA truncus. There have been a number of descriptive CTA and cadaveric studies related to IPA variations published in literature (4511131415), however, the vast majority being carried out in patients with liver disease. This study is unique in its evaluation of the relationship between inferior phrenic artery origin and celiac axis variation. Furthermore, the number of patients evaluated exceeds those currently existing in literature.
It can be difficult to assess the overall arterial anatomy with digital subtraction angiography (DSA). Determining specific anatomy and variations found is more effective with the use of CTA. Furthermore, performing a CTA before interventional procedures eliminates the need for aortography (13). In addition, considering the selective embolization process during interventional procedures, a CTA is capable of saving significant time by allowing one to evaluate the full anatomy of the patient, including, vascular variations and parenchymal diseases prior to interventions (13).
Inferior phrenic arteries originate not only from the aorta and celiac axis but also, from many different arteries (17). Basile et al. (4) classified IPA variations in 13 different groups in their study using multidetector CT. Loukas et al. (7) evaluated the origins of RIPA and LIPA in 300 cadavers and classified them into five groups. Basile et al. (4) and Loukas et al. (7) found that the IPA originated the most from the celiac axis. Despite this, Basile et al. (4) neglects to mention IPA with a common trunk as its origin. Both of them enrolled patients with liver disease into their studies.
The reported frequencies of IPA variations were similar to our results in a similar study utilizing CTA (11). This is also the only previous study that described the IPA variations in 200 patients without liver disease using CTA. They reported on a RIPA that originated from the proper hepatic artery, in contrast to our study where the RIPA originated from the common hepatic artery. Additionally, its important to note our study group was larger and without the focus on liver disease, we have also discovered a LIPA originating from right renal artery that has not previously been described in prior studies.
Knowing IPA origin is important in a number of clinical situations. TACE is treatment of choice in the unresectable HCC (16). Besides ensuring improvement in the prognosis of patients with HCC, it also provides benefits in tumor control (316). Prior to TACE procedure, identification of the tumor arterial supply using CTA is extremely important for both successful treatment with complete embolization of the blood supply and preventing complications due to embolization of the nontargeted branches (13). Hepatic neoplasms commonly derive their arterial supply from the hepatic arteries, but, extrahepatic collateral vessels can also supply the entire or at least part of the hepatic neoplasm. IPA are among the most important collateral supplies of HCCs, especially those located in the peripheral segments and bare areas of the liver (117). The enlargement of the RIPA, especially those exceeding 2.5 mm, have been considered a sign of collateral supply of the tumor by IPA on CTA (14).
Inferior phrenic arteries also prevent development of ischemia or necrosis in vital organs in case of arterial stenosis or occlusion. The LIPA can result in anastomosis with transdiaphragmatic collaterals and left anterior descending coronary artery, which may play an important role in atherosclerotic ischemic heart diseases (18). Occurance of anastomosis resulted between the medial branch of LIPA and pericardiophrenic, musculophrenic arteries. Furthermore, a post-traumatic pericardial tamponade developed secondary to these anastomosis and was subsequently treated with LIPA embolization where reported have been reported (18).
The LIPA provides blood supply to the gastroesophageal junction and thus should be considered in the event of upper gastrointestinal bleeding, if the origin of the bleeding source is not demonstrated at routine selective catheterization (119). Intra-abdominal bleeding may be induced by LIPA after a gastrectomy and the LIPA originated from the left gastric artery may be injured or ligated during the surgical process of both gastrectomy and repair of hiatal hernia (1520). Pseudoaneurysms originating from the LIPA may cause upper gastrointestinal system bleeding or post-traumatic intra-abdominal massive hemorrhaging (9). The collaterals from the LIPA may supply tumoral lesions developed around the region of the esophagogastric junction (19).
Diseases associated with fibrosis and decreased pulmonary blood flow, such as bronchiectasis, cystic fibrosis, tuberculosis, sarcoidosis, chronic pneumonia, congenital pulmonary artery stenosis may cause the development of transpleural systemic-pulmonary artery anastomosis. If one of the aforementioned lung abnormalities is located at the base of the lung, IPA should also be considered as a potential cause of massive hemoptysis (1). Massive hemoptysis due to IPA may also be encountered in patients with chronic pancreatitis (8).
The celiac axis is the first branch of the abdominal aorta and classically has trifurcation, this includes the common hepatic artery, left gastric artery, and splenic artery. Apart from classical trifurcation, it may show variations (122122). The largest study group in relevant literature looked at celiac axis variations in 5002 patients using CTA and DSA (12). In our study group, celiac axis variations were detected in 10% of patients and the hepatosplenic truncus was the most common variation, as described previously by Song et al. (12).
The relationship between IPA origin and celiac axis variations could be explained by embryologic development of the celiac axis. The primitive aorta possesses ventral, lateral and posterior segments. The ventral segments, that later become the celiac axis, have longitudinal anastomosis between each other. Regression of the ventral segmental roots, or non-regression and continuous growth of the longitudinal anastomosis results in anatomical variations of the celiac axis (122223). The celiac axis variations may cause variations in origin of IPAs as a result of the IPA being developed mostly from the ventral segments of the primitive aorta, most probably from similar levels.
There were several limitations with our study. First, the IPAs are small vessels and sometimes result in differences in interpretation of IPA origin. We attempted to overcome this problem by review of all images independently by two radiologists. However, we did not evaluate the intraobserver and interobserver agreement and the study was conducted on the basis of consensus opinion. Secondly, we were unable to obtain digital subtraction angiography images of the patients and relied on the evaluation of all variations from CTA images. Despite this, recent advances in CTA allow for better visualization of small vessels and have replaced digital subtraction angiography in many clinical algorithms of the abdominal vasculature (424).
In conclusion, anatomy and variations of the IPA are clinically important and can be evaluated using CTA before surgical or interventional treatments. The IPA originated for the most part from the aorta in patients with a common IPA trunk, and the RIPA and the LIPA originated the most from the celiac axis in patients without a common IPA trunk. Origin of the IPA may diversify in the presence of celiac axis variation.
Figures and Tables
 | Fig. 1Flowchart shows study population and patient selection process.CTA = computed tomography angiography, HCC = hepatocellular carcinoma, IPA = inferior phrenic artery
|
 | Fig. 2Schematic representation of origin of inferior phrenic arteries with common trunk.A = aorta, CA = celiac axis, LGA = left gastric artery, LIPA = left inferior phrenic artery, LRA = left renal artery, RIPA = right inferior phrenic artery, RRA = right renal artery
|
 | Fig. 3CT angiography MIP images show inferior phrenic artery (IPA) originating aorta (A), celiac axis (B), and right renal artery (C) as common trunk (arrowheads).White arrows: right IPA, black arrows: left IPA. MIP = maximum intensity projections
|
 | Fig. 4Schematic representation of origin of inferior phrenic arteries without common trunk.A = aorta, CA = celiac artery, CHA = common hepatic artery, LGA = left gastric artery, LIPA = left inferior phrenic artery, LRA = left renal artery, RIPA = right inferior phrenic artery, RRA = right renal artery, SA = splenic artery
|
 | Fig. 5CT angiography MIP images show right inferior phrenic artery (RIPA, white arrow) and left inferior phrenic artery (LIPA, black arrow) originating separately without truncus.
A. Both RIPA and LIPA originate from celiac axis (black arrowhead). B. RIPA originates from right renal artery and LIPA from aorta. C. RIPA originates from left gastric artery (white arrowhead) and LIPA from celiac axis (not shown). MIP = maximum intensity projections
|
 | Fig. 6CT angiography MIP image shows left inferior phrenic artery (black arrow) arising from back of aorta.MIP = maximum intensity projections
|
 | Fig. 7CT angiography MIP image demonstrates right inferior phrenic artery (white arrow) originates from right superior polar renal artery.MIP = maximum intensity projections
|
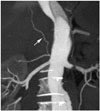
 | Fig. 8CT angiography images of patient with celiac axis variation.
A. CT angiography MIP image demonstrates no celiac truncus and common hepatic artery (black arrowhead), splenic artery (white arrowhead) and left gastric artery originate from aorta rather than celiac trifurcation. B. CT angiography 3D volume-rendered image shows that right inferior phrenic artery (white arrows) arising from common hepatic artery (black arrowhead). White arrowhead indicates splenic artery and black arrow shows left inferior phrenic artery, arising from aorta. MIP = maximum intensity projections
|
Table 1
Origin of Inferior Phrenic Artery in Patients without Celiac Axis Variation

Table 2
Origin of Inferior Phrenic Artery in Patients with Celiac Axis Variation

Table 3
Relationship between Origin of Inferior Phrenic Artery Truncus and Celiac Axis Variation*

Table 4
Relationship between Origin of RIPA and Celiac Axis Variation*

Table 5
Relationship between Origin of LIPA and Celiac Axis Variation*

References
1. Gwon DI, Ko GY, Yoon HK, Sung KB, Lee JM, Ryu SJ, et al. Inferior phrenic artery: anatomy, variations, pathologic conditions, and interventional management. Radiographics. 2007; 27:687–705.
2. Liu PS, Platt JF. CT angiography in the abdomen: a pictorial review and update. Abdom Imaging. 2014; 39:196–214.
3. Lee AJ, Gomes AS, Liu DM, Kee ST, Loh CT, McWilliams JP. The road less traveled: importance of the lesser branches of the celiac axis in liver embolotherapy. Radiographics. 2012; 32:1121–1132.
4. Basile A, Tsetis D, Montineri A, Puleo S, Massa Saluzzo C, Runza G, et al. MDCT anatomic assessment of right inferior phrenic artery origin related to potential supply to hepatocellular carcinoma and its embolization. Cardiovasc Intervent Radiol. 2008; 31:349–358.
5. Gürses İA, Gayretli Ö, Kale A, Öztürk A, Usta A, Şahinoğlu K. Inferior phrenic arteries and their branches, their anatomy and possible clinical importance: an experimental cadaver study. Balkan Med J. 2015; 32:189–195.
6. Lee JW, Kim S, Kim CW, Kim KH, Jeon TY. Massive hemoperitoneum due to ruptured inferior phrenic artery pseudoaneurysm after blunt trauma. Emerg Radiol. 2006; 13:147–149.
7. Loukas M, Hullett J, Wagner T. Clinical anatomy of the inferior phrenic artery. Clin Anat. 2005; 18:357–365.
8. Takanami I. Massive haemoptysis due to chronic pancreatitis: control with inferior phrenic artery embolization. Eur J Cardiothorac Surg. 2000; 18:120–122.
9. Arora A, Tyagi P, Gupta A, Arora V, Sharma P, Kumar M, et al. Pseudoaneurysm of the inferior phrenic artery presenting as an upper gastrointestinal bleed by directly rupturing into the stomach in a patient with chronic pancreatitis. Ann Vasc Surg. 2012; 26:860.e9–860.e11.
10. Hong SS, Kim AY. Early postoperative bleeding after living donor liver transplantation. Abdom Imaging. 2009; 34:365–370.
11. Ozbulbul NI, Yurdakul M, Tola M, Akdogan G, Olcer T. Can multidetector row CT visualize the right and left inferior phrenic artery in a population without disease of the liver? Surg Radiol Anat. 2009; 31:681–685.
12. Song SY, Chung JW, Yin YH, Jae HJ, Kim HC, Jeon UB, et al. Celiac axis and common hepatic artery variations in 5002 patients: systematic analysis with spiral CT and DSA. Radiology. 2010; 255:278–288.
13. Hieda M, Toyota N, Kakizawa H, Ishikawa M, Horiguchi J, Ito K. The anterior branch of the left inferior phrenic artery arising from the right inferior phrenic artery: an angiographic and CT study. Cardiovasc Intervent Radiol. 2009; 32:250–254.
14. Miclaus GD, Matusz P, Loukas M, Ples H. Rare case of the trunk of the inferior phrenic arteries originating from a common stem with a superior additional left renal artery from the abdominal aorta. Clin Anat. 2012; 25:979–982.
15. Tanaka R, Ibukuro K, Akita K. The left inferior phrenic artery arising from left hepatic artery or left gastric artery: radiological and anatomical correlation in clinical cases and cadaver dissection. Abdom Imaging. 2008; 33:328–333.
16. Gonsalves CF, Brown DB. Chemoembolization of hepatic malignancy. Abdom Imaging. 2009; 34:557–565.
17. Kim HC, Chung JW, An S, Seong NJ, Jae HJ, Cho BH, et al. Left inferior phrenic artery feeding hepatocellular carcinoma: angiographic anatomy using C-arm CT. AJR Am J Roentgenol. 2009; 193:W288–W294.
18. Jones BV, Vu D. Diagnosis of posttraumatic pericardial tamponade by plain film and computed tomography and control of bleeding by embolotherapy of the left inferior phrenic artery. Cardiovasc Intervent Radiol. 1993; 16:183–185.
19. Zeng R, Yao Z, Chen Y, Xu Z, Chen Y, Liu J. Variant arterial supply to the lesser curvature of the stomach and duodenum from double inferior phrenic arteries. Surg Radiol Anat. 2015; 37:867–869.
20. Mu GC, Huang Y, Liu ZM, Lin JL, Zhang LL, Zeng YJ. Clinical research in individual information of celiac artery CT imaging and gastric cancer surgery. Clin Transl Oncol. 2013; 15:774–779.
21. Ozbülbül NI. CT angiography of the celiac trunk: anatomy, variants and pathologic findings. Diagn Interv Radiol. 2011; 17:150–157.
22. Iezzi R, Cotroneo AR, Giancristofaro D, Santoro M, Storto ML. Multidetector-row CT angiographic imaging of the celiac trunk: anatomy and normal variants. Surg Radiol Anat. 2008; 30:303–310.
23. Winston CB, Lee NA, Jarnagin WR, Teitcher J, DeMatteo RP, Fong Y, et al. CT angiography for delineation of celiac and superior mesenteric artery variants in patients undergoing hepatobiliary and pancreatic surgery. AJR Am J Roentgenol. 2007; 189:W13–W19.
24. So YH, Chung JW, Yin Y, Jae HJ, Jeon UB, Cho BH, et al. The right inferior phrenic artery: origin and proximal anatomy on digital subtraction angiography and thin-section helical computed tomography. J Vasc Interv Radiol. 2009; 20:1164–1171.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download