Abstract
Objective
To determine the effect of reduced abdominal compression in prone position on ascending colonic movement during supine-to-prone positional change during CT colonography (CTC).
Materials and Methods
Eighteen consecutive patients who had undergone prone CTC scanning with cushion blocks placed under the chest and hip/thigh to reduce abdominal compression and had confirmed sessile polyps ≥ 6 mm in the well-distended, straight, mid-ascending colon, were included. Radial location along the ascending colonic luminal circumference (°) was measured for 24 polyps and 54 colonic teniae on supine and prone CTC images. The supine-to-prone change ranging between -180° and +180° (- and + for internal and external colonic rotations, respectively), was determined. In addition, possible causes of any ascending colonic rotations were explored.
Results
Abdominal compression during prone CTC scanning completely disappeared with the use of cushion blocks in 17 of 18 patients. However, some degrees of ascending colonic rotation were still observed, with the radial location changes of -22° to 61° (median, 13.9°) for the polyps and similar degrees for teniae. Fifty-four percent and 56% of polyps and teniae, respectively, showed changes > 10°. The radial location change of the polyps was significantly associated with the degree of anterior shift of the small bowel and mesentery (r = 0.722, p < 0.001) and the degree of posterior displacement of the ascending colon (r = 0.566, p = 0.004) during supine-to-prone positional change.
Dual-position image acquisition, including supine and prone scans, is generally considered a standard procedure for computed tomography colonography (CTC) (123). CT scanning in the 2 consecutive, opposed positions helps to achieve complete mucosal evaluation by redistributing luminal fluid, stool, and gas (4567). The lesional location during the positional change can be determined as immobile, suggestive of a true lesion and mobile, suggestive of a false lesion that is a mobile stool piece, which is crucial to achieve a competent interpretation of CTC (7). An accurate confirmation of the mobility or lack of mobility of a suspected lesion requires a precise registration of supine and prone CTC images, which is sometimes quite challenging (8) as colonic segments often lack specific topographic landmarks; in addition, untagged sticky stool pieces occasionally move only mildly instead of full gravitational movement towards the opposite side of the colonic wall, and the colon may undergo considerable movement or deformation during the positional change (9101112), thus mimicking lesion mobility. Mobility of the colon during the positional change of CTC typically occurs in the sigmoid colon, the transverse colon, and the cecum (1011); however, a recent study (12) indicated that it can also be seen in the ascending colon (and presumably similarly in the descending colon that is in the mirror-image location). Colonic mobility occurs in unexpected locations, such as the ascending colon; hence, it could be deceptive and pose an even greater interpretive challenge to readers who customarily assume it to be immobile and fixed to the retroperitoneum. Ascending colonic mobility during the supine-to-prone positional change of CTC is due to abdominal compression in the prone position, which causes the ascending colon to rotate externally, particularly when the ascending colon has an anatomically variant, long mesocolon (121314). Abdominal compression leads to suboptimal distention or collapse of some colonic segments in the prone position and therefore, measures to decrease pressure on the abdomen in the prone position, such as placement of a pillow under the chest and thigh are currently recommended (1). The ascending colonic mobility during the positional change of CTC is correlated with abdominal compression in the prone position (12); hence, we hypothesize that reducing abdominal compression in the prone position may also decrease the ascending colonic rotation during supine-prone positional change of CTC and, therefore, help to prevent interpretive errors. Therefore, the purpose of this study was to determine the effect of reduced abdominal compression in the prone-position on the movement of the ascending colon during the supine-to-prone positional change of CTC.
This retrospective study was approved by the Institutional Review Board of Asan Medical Center. The requirement for patient informed consent was waived.
We designed this study to assess ascending colonic rotation/mobility during the positional change of CTC by assessing the position of proven, immobile, ascending colonic polyps (see the section on CTC image analysis), according to the method established in a published study (12). Eligible patients who fulfilled all of the following criteria were identified from our clinical CTC registry: 1) prone CTC scan performed with placement of cushion blocks under the chest and hip/thigh in order to decrease abdominal compression (Fig. 1); 2) the presence of sessile polyps ≥ 6 mm in maximum diameter in the straight mid-portion of the ascending colon confirmed by colonoscopy performed within 6 months of the CTC; 3) optimally distended ascending colon and clear visualization of the mid-ascending colonic polyps on both supine and prone CTC images; 4) absence of any conditions that might affect ascending colonic rotation/mobility, such as advanced cancer or inflammation with pericolic extension; and 5) lack of notable deformities of the spine such as scoliosis or kyphosis so that the analytic method of this study could be correctly applied (see the section on CTC image analysis). Pedunculated or flat lesions were excluded as the former are inherently mobile and the latter may have low conspicuity on CTC images. Of the 1218 clinical CTC examinations performed at Asan Medical Center, a tertiary referral center, between January 2013 and July 2014, 18 eligible patients were identified (16 men and 2 women; mean age ± standard deviation [SD], 65.1 ± 12 years). These 18 patients had a total of 24 sessile polyps in the mid-ascending colon, including 12 patients each with a single eligible polyp and 6 patients each with 2 eligible polyps. The mid-ascending colonic polyps were 6 to 16 mm in maximum diameter and consisted of 15 tubular adenomas, 3 cancerous polyps, and 6 hyperplastic polyps. The same location of the colonic polyps in the colon on the supine and prone CTC images, was accurately confirmed by continuously tracing 3 colonic teniae and haustral folds from the ileocecal area to the lesions using a 3-dimensional panoramic endoluminal display technique (15) on a commercial CTC system (Xelis Colon; Infinitt Healthcare, Seoul, Korea).
CTC was performed after cathartic purgation and fecal/fluid tagging with oral administration of 50 mL of 350 mgI/mL iohexol (Omnipaque 350; GE Healthcare, Little Chalfont, United Kingdom). Colonic distention with carbon dioxide was achieved using an automated insufflator (PROTOCO2L colon insufflator; Bracco, Milan, Italy). Both prone and supine scans were obtained using a 16-detector row CT scanner (Somatom Sensation 16; Siemens Medical Solutions, Erlangen, Germany). As the patients were symptomatic, both unenhanced and contrast-enhanced scans were performed. Scan parameters for the unenhanced scan were as follows: beam collimation, 16 × 0.75 mm; reconstructed section thickness, 1 mm; reconstruction interval, 0.7 mm; beam pitch, 1; gantry rotation time, 0.5 second; field of view, to fit; 120 kVp; and 50 mAs. The subsequent contrast-enhanced scan was obtained after positional change during the portal phase (72-second delay) after administering 2 mL/kg-body weight iopromide (Ultravist 300; Bayer Healthcare, Berlin, Germany) or iohexol at a rate of 2.5-3.0 mL/sec. Scan parameters were the same as those for the unenhanced scan except for the use of an automated dose-reduction system (CARE Dose 4D; Siemens Medical Solutions) with the maximum allowable tube current set at 200 mAs. We placed 1 rectangular-shaped cushion block under the lower chest and 1 under the hip/thigh with the patient in the prone position so as to decrease abdominal compression against the table (Fig. 1). The height of the cushion blocks was approximately 7-8 cm when compressed by body weight.
A commercial image processing workstation system (Lucion; Infinitt Healthcare, Seoul, Korea) was used for the analysis.
The radial location of colonic polyps and teniae in degrees (0° to 360°) along the ascending colonic circumference, as seen on transverse 2-dimensional CTC images with respect to fixed anatomical landmarks of the torso, was measured according to a previously reported coordinate system that is unaffected by rotation or tilting of the torso (12). The observer variability of this measurement method is already reportedly within ± 10° (12), hence, we did not assess observer variability in this study. Instead, we performed the measurement in consensus between 2 radiologists (each with clinical experience reviewing approximately 200 or 3000 CTC cases) in order to minimize any subjectivity in determining the radial polyp location. In brief, the coordinate system uses several reference lines. A straight horizontal line was drawn to connect the lateral tips of the transverse processes of the lumbar vertebra that was closest to the polyp of interest in order to remove any influence of rotation/tilting of the torso with respect to the CT table. A line parallel to the previous line was then drawn to pass through the center of the distended ascending colonic lumen. The 2 points where this line met with the colon wall were given the circumferential coordinates of 90° (medial wall) and 270° (lateral wall). Subsequently, a vertical line that was perpendicular to the horizontal line and passed through the center of the ascending colonic lumen was drawn. The 2 points where this line crossed the colon wall were designated as 0° (anterior wall) and 180° (posterior wall). The radial location of a polyp was then obtained by measuring the angle between the vertical line of 0° and the line that connected the center of the lumen and the center of the polyp in degrees with clockwise increments. The measurement was performed for the supine image set and the prone image set in 2, separate sessions 2 months apart in order to avoid recall bias. The difference between the supine and prone measurements was then recorded between -180° and +180°, where - and + represented internal and external rotation, respectively, of the ascending colon with the patient in the prone position (Fig. 2B), as compared with the supine position (Fig. 2A). Since the cross-sectional appearance of the ascending colon is not completely circular and the radial location change between supine and prone images can also be created by colonic deformation rather than by rotation during positional change, we also measured the radial location change of 3 colonic teniae, i.e., the libera, mesocolica, and omentalis, at the level of the mid-ascending colon in order to confirm whether the degrees of radial location change were coherent among the 3 colonic teniae and the colonic polyp as coherent changes among them would clearly indicate a colonic rotation.
In order to explore plausible causes of ascending colonic movement during supine-to-prone positional change, if any movement occurred, another radiologist who did not participate in the radial location measurement and was blinded to the radial location results, performed the measurement of several quantitative abdominal indices as explained below and also visually assessed the positions of intra-abdominal structures. An anthropometric index, Abdcomp, to demonstrate the degree of abdominal compression in the prone position, as compared with the supine position was obtained: (abdominal thicknesssupine - abdominal thicknessprone) / abdominal thicknesssupine × 100%, where the abdominal thickness was the distance from the anterior abdominal wall to the anterior margin of the lumbar spine at the level of the umbilicus, as seen on transverse CTC images (Fig. 3). Therefore, a greater value indicated a greater degree of abdominal compression in the prone position. An index to represent the degree of anterior shift of the small bowel and mesentery during supine-to-prone positional change, SMAshift, was measured by the difference in aorto-mesenteric angle, i.e., angle between the abdominal aorta and the straight main trunk of the superior mesenteric artery, between prone and supine positions (prone angle - supine angle) (Fig. 4A). A greater SMAshift value indicated a greater anterior shift of the small bowel and mesentery in the prone position. Any apparent visual movement or reposition of the small bowel and mesentery was also noted. Another index, Ascdisp, defined as the distance of ascending colonic movement in the anteroposterior direction that is vertical to the aforementioned reference horizontal line during the supine-to-prone positional change, was determined using the lumbar spine as the reference structure and by measuring the vertical anteroposterior distances between the horizontal line going through the center of the distended mid-ascending colon and a parallel horizontal line that is tangent to the anterior margin of the lumbar spine in the supine and prone positions (Fig. 3). Positive values indicated posterior displacement of the ascending colon in the prone position, as compared with the supine position.
Statistical distributions of the data were confirmed and descriptive statistics were appropriately obtained. Correlations between the radial location change of the colonic polyps and teniae and the 3 abdominal indices including Abdcomp, SMAshift, and Ascdisp were analyzed using the Spearman correlation analysis. IBM SPSS Statistics for Windows (version 21.0; IBM Corp., Armonk, NY, USA) was used for statistical analyses. Two-sided p values < 0.05 were considered statistically significant.
The difference in the radial location between the supine and prone positions ranged from -22° to 61° for the 24 polyps (median, 13.9°; interquartile range, 0.9° to 24.6°) (Fig. 5). Eighty-eight percent (21 of 24 in 16 patients) of the polyps showed positive values of the radial location change, thus indicating external rotation of the ascending colon in the prone position, as compared with the supine position. Fifty-four percent (13 of 24 in 12 patients) of the polyps showed a radial location change greater than 10° and 13% (3 of 24 in 3 patients) showed a change greater than 30° (41°, 42°, and 61°). The results for the 3 colonic teniae were similar (Table 1), thus indicating that the radial location changes were caused by universal rotation of the ascending colon.
Abdcomp ranged from -36.1 to 21.8% (mean ± SD, -12.8 ± 12.1%) and it had a negative value in 17 of the 18 patients, i.e., complete absence of abdominal compression and further anterior protrusion of the abdomen in the prone position, as compared with the supine position. Abdcomp was not significantly correlated with the radial location change of the colonic polyps or of any of the colonic teniae (Table 2). SMAshift ranged from -12.9° to 38° (mean ± SD, 16.1 ± 12.9°) and was positive in 17 of the 18 patients, i.e. anterior shift of the small bowel and mesentery in the prone position. Consistent with these numerical values, an apparent lump of the small bowel and mesentery was displaced anteriorly in the prone position and occupied the intra-abdominal space anteromedial to the mid-ascending colon (Fig. 4) in most patients at visual evaluation. SMAshift showed a significant correlation with the radial location change of the colonic polyps (r = 0.722, p < 0.001) and statistical trends of correlation with 3 colonic teniae (r = 0.399 to 0.462, p = 0.054 to 0.101) (Table 2). Ascdisp ranged from -6.1 to 26.6 mm (mean ± SD, 9.5 ± 8.7 mm) and had a positive value in 15 of the 18 patients, i.e., posterior displacement of the ascending colon in the prone position, as compared with the supine position. Ascdisp showed a significant correlation with the radial location change of colonic polyps (r = 0.566, p = 0.004) and colonic teniae (r = 0.562 to 0.702, p < 0.015) (Table 2).
The results of the study indicated that the ascending colonic rotation that occurs during the supine-to-prone positional change during CTC was only slightly decreased by removing the abdominal compression in the prone position, demonstrating -22° to 61° (median, 13.9°) radial location changes for the ascending colonic polyps, as compared with -23° to 79° (median, 21°) reported in a previous study (12). The ascending colon externally rotated in approximately half of the patients beyond the reported range of observer variability, i.e., > 10° (12). These degrees of rotation were smaller than the maximum gravitational shift of 180° during the supine-to-prone positional change that can be seen with a freely mobile intraluminal object. However, considering that untagged sticky stool pieces may occasionally move only mildly, particularly when reduced preparation is used, the relatively small degrees of ascending colonic rotation may still represent a notable interpretive pitfall as previously reported (12). We anticipate a similar pitfall associated with colonic rotation also in the descending colon, given its mirror-image anatomical location, as compared with the ascending colon. We did not directly investigate the descending colon in this study, since the absence versus presence of mobility in the descending colon by continuous tracing of colonic teniae and folds from the cecum was impossible to confirm.
In this study, the external abdominal compression in the prone position completely disappeared with the placement of the cushion blocks; hence, the ascending colonic rotation could not be explained by abdominal compression as indicated by lack of correlation between Abdcomp and the radial location change of the ascending colonic polyps or teniae. The correlation occurs only when abdominal compression is present. Consequently, our results suggested an intra-abdominal mechanism in the prone position on release of abdominal compression that exerts forces to the ascending colon in a manner similar to external abdominal compression. While the exact intra-abdominal mechanism remains unclear, some of the study findings could provide possible explanations. In the prone position, the small bowel and mesentery was shifted anteriorly, as expected, by gravitational repositioning; whereas, despite the lack of abdominal compression in the prone position, the ascending colon was displaced posteriorly in most patients. Both SMAshift and Ascdisp were significantly correlated with ascending colonic rotation although the correlation with SMAshift was not statistically significant when assessed with 3 colonic teniae, probably due to the smaller subject number. Posterior displacement of the ascending colon on supine-to-prone position change during CTC is known (9); however, it occurs as a consequence of anterior abdominal compression when lying prone, which displaces the intra-abdominal contents posteriorly. Therefore, in this study, with the release of abdominal compression in the prone position using the cushion blocks, we expected the opposite due to the effects of gravity. The collective results of the displacements of the small bowel and mesentery and the ascending colon, as well as their correlations with the ascending colonic rotation, the unexpected movement of the ascending colon in the prone position with no external abdominal compression could be explained as follows. The highly mobile small bowel and the mesentery would readily move anteriorly due to gravity when changing from the supine to the prone position, particularly in the absence of abdominal compression in the prone position, and would preoccupy the intra-abdominal space anteromedial to the mid-ascending colon. As the abdominal cavity is not a freely expandable space, the repositioned small bowel and mesentery would push adjacent structures away to a certain extent and the ascending colon would be pushed posteriorly as well as laterally given its spatial relationship with the small bowel and consequently result in an external rotation of the ascending colon.
This study indicates the importance of awareness of the ascending colonic rotation during supine-to-prone positional change during CTC to avoid misinterpretation of CTC findings, since it is not easily prevented by any particular patient positioning or scanning methods. Furthermore, our study underscores the general importance of confirming the mobility or lack of mobility of a suspected lesion on CTC by careful topographic comparisons with other available fixed structures, such as colonic folds, teniae or diverticula, using both, 3-dimensional and 2-dimensional views rather than a simple comparison of apparent lesion locations on 2-dimensional images. This careful interpretive approach is particularly important, since CTC can be obtained not only in the standard supine-prone positions but also in alternative positions, including lateral decubitus positions (16171819). The degree and pattern of colonic movement caused by lateral decubitus positions of patients would likely differ from standard supine-to-prone change; hence, comparing lesion locations between different sets of CTC images is even more difficult.
The degree of ascending colonic rotation was not large in the majority of our patients, whereas quite substantial degrees of colonic rotation were observed in a small number of patients. These occasional large degrees of colonic rotation are most likely related to an unusual anatomical variation of incomplete (or a lack of) fusion between the embryonic ascending mesocolon and the posterior parietal peritoneum, which leaves the ascending colon connected to the posterior abdominal wall via a long mesocolon rather than tightly anchored completely embedded in the retroperitoneum (131420). According to a prospective study on patients undergoing laparotomy, an ascending mesocolon of ≥ 10 cm in length is present in approximately 10% (11 of 115) of patients from western countries, with some difference among ethnic groups (14).
There are limitations to our study. First, our study did not directly investigate the clinical implication of this potential pitfall. The phenomenon of ascending colonic rotation may pose a greater interpretive challenge to those who primarily use 2-dimensional interpretation. Generally, it is relatively easier with 3-dimensional review to confirm the same vs. different locations of a colonic structure between different sets of CTC images and 3-dimensional review is dominantly used in current daily practice. Furthermore, we did not directly evaluate the ultimate effect of this pitfall on diagnostic accuracy of CTC. Secondly, as the ascending colon is not a completely circular tube and the measurement technique used in this study relied on radiologists' visual interpretation for determining the various reference points, small measurement errors would be unavoidable. The measurement method was established and approved in a previously published study; however, some degree of observer variability (approximately ± 10° in terms of the radial location) is known to exist (12). We accordingly attempted to minimize the error and subjectivity by performing the measurements in consensus. Thirdly, there was a small possibility that the degree of colonic rotation was slightly underestimated. True colonic lesions misinterpreted as false lesions in our practice due to large degrees of ascending colonic rotation were not likely to have follow-up colonoscopy and, therefore, were possibly missed in the study case search.
In conclusion, ascending colonic rotation that occurs with supine-to-prone positional change during CTC was not eliminated by removing abdominal compression in prone position. The majority of patients still showed an external rotation of the ascending colon during the positional change even without abdominal compression. Awareness of the ascending colonic rotation is important to prevent interpretive pitfalls.
Figures and Tables
Fig. 1
Placement of 2 cushion blocks (double arrows) under lower chest and hip/thigh in prone position demonstrated in sagittal (upper) and transverse (lower) images.

Fig. 2
Coordinate system to determine radial location of polyp or tenia along circumference of mid-ascending colon in supine (A) and prone (B) positions.
Horizontal, white line (labeled as A) is drawn to connect lateral tips of transverse processes of lumbar vertebra that are closest to polyp of interest (which is projected onto present image at exact level where polyp is shown) and is used as reference horizontal line. Blue line (labeled as B) parallel to line A is drawn to pass through center of distended, mid-ascending colonic lumen. 2 points where line B meets with colon wall are given circumferential coordinates of 90° and 270°. Another green line (labeled as C) that is perpendicular to line B and passes through center of ascending colonic lumen is drawn. 2 points where this line crosses colon wall are designated as 0° and 180°. Radial location of polyp (arrows) is then obtained by measuring angle between vertical line of 0° and line that connects center of lumen and center of polyp in degrees with clockwise increments. Polyp radial location in this example is 243° and 226° in supine and prone positions, respectively, indicating external rotation of ascending colon by 17° during supine-to-prone position change.

Fig. 3
Measurement of anthropometric indices.
Abdcomp is defined as (abdominal thicknesssupine - abdominal thicknessprone) / abdominal thicknesssupine x 100%, where abdominal thickness was distance from anterior abdominal wall to anterior margin of lumbar spine at level of umbilicus. Ascdisp, distance of ascending colonic movement in anteroposterior direction vertical to aforementioned reference horizontal line, is calculated by comparing distance labeled as d, vertical anteroposterior distance between horizontal line that passes through center of distended mid-ascending colon, and parallel horizontal line that is tangent to anterior margin of lumbar spine, between supine and prone positions.
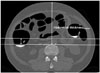
Fig. 4
Anterior displacement of mesentery and small bowel, which pushes ascending colon posterolaterally in 59-year-old man.
A. SMAshift measured by difference in aorto-mesenteric angle, which is angle between abdominal aorta (Aorta; red line) and straight main trunk of superior mesenteric artery (SMA; yellow line), between prone and supine positions is 38° in this example, i.e., prone angle of 18° - supine angle of -20°. B. External rotation of ascending colon by 61° (219° - 158°) during supine-to-prone positional change in absence of abdominal compression is demonstrated by radial locations of 6-mm, sessile, tubular adenoma. Prone CT colonography image shows large lump consisting of mesentery and small bowel, which is displaced anteriorly due to gravity and occupying large space in anteromedial side of abdomen (arrows). TM, TL, and TO represent tenia mesocolica, tenia libera, and tenia omentalis. C. Endoscopic image shows sessile polyp (arrow) in mid-ascending colon.

Fig. 5
Histogram showing distribution of polyp radial location difference during supine-to-prone positional change.
Each bar represents number of polyps for each 10° range, e.g., 7 polyps in 0° to < 10° range. Negative and positive values (°) represent internal and external rotation, respectively, of ascending colon in prone position, as compared with supine position.

Table 1
Radial Location Change of Polyps and Teniae of Mid-Ascending Colon
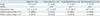
Table 2
Correlation between Radial Location Change and Anthropometric Indices

References
1. Dachman AH. Scheduling, performing and reporting CT colonography. In : Dachman AH, Laghi A, editors. Atlas of virtual colonoscopy. 2nd ed. New York, NY: Springer-Verlag, Inc.;2011. p. 87–109.
2. Kim DH, Pickhardt PJ. MDCT protocol for CT colonography. In : Pickhardt PJ, Kim DH, editors. CT colonography: principles and practice of virtual colonoscopy. 1st ed. Philadelphia, PA: Saunders Elsevier;2010. p. 148–156.
3. Neri E, Halligan S, Hellström M, Lefere P, Mang T, Regge D, et al. The second ESGAR consensus statement on CT colonography. Eur Radiol. 2013; 23:720–729.
4. Chen SC, Lu DS, Hecht JR, Kadell BM. CT colonography: value of scanning in both the supine and prone positions. AJR Am J Roentgenol. 1999; 172:595–599.
5. Fletcher JG, Johnson CD, Welch TJ, MacCarty RL, Ahlquist DA, Reed JE, et al. Optimization of CT colonography technique: prospective trial in 180 patients. Radiology. 2000; 216:704–711.
6. Morrin MM, Farrell RJ, Keogan MT, Kruskal JB, Yam CS, Raptopoulos V. CT colonography: colonic distention improved by dual positioning but not intravenous glucagon. Eur Radiol. 2002; 12:525–530.
7. Yee J, Kumar NN, Hung RK, Akerkar GA, Kumar PR, Wall SD. Comparison of supine and prone scanning separately and in combination at CT colonography. Radiology. 2003; 226:653–661.
8. Boone DJ, Halligan S, Roth HR, Hampshire TE, Helbren E, Slabaugh GG, et al. CT colonography: external clinical validation of an algorithm for computer-assisted prone and supine registration. Radiology. 2013; 268:752–760.
9. Punwani S, Halligan S, Tolan D, Taylor SA, Hawkes D. Quantitative assessment of colonic movement between prone and supine patient positions during CT colonography. Br J Radiol. 2009; 82:475–481.
10. Chen JC, Dachman AH. Cecal mobility: a potential pitfall of CT colonography. AJR Am J Roentgenol. 2006; 186:1086–1089.
11. Mang T, Maier A, Plank C, Mueller-Mang C, Herold C, Schima W. Pitfalls in multi-detector row CT colonography: a systematic approach. Radiographics. 2007; 27:431–454.
12. Kim JY, Park SH, Lee SS, Kim AY, Ha HK. Ascending colon rotation following patient positional change during CT colonography: a potential pitfall in interpretation. Eur Radiol. 2011; 21:353–359.
13. Saunders BP, Phillips RK, Williams CB. Intraoperative measurement of colonic anatomy and attachments with relevance to colonoscopy. Br J Surg. 1995; 82:1491–1493.
14. Saunders BP, Masaki T, Sawada T, Halligan S, Phillips RK, Muto T, et al. A peroperative comparison of Western and Oriental colonic anatomy and mesenteric attachments. Int J Colorectal Dis. 1995; 10:216–221.
15. Lee SS, Park SH, Kim JK, Kim N, Lee J, Park BJ, et al. Panoramic endoluminal display with minimal image distortion using circumferential radial ray-casting for primary three-dimensional interpretation of CT colonography. Eur Radiol. 2009; 19:1951–1959.
16. Buchach CM, Kim DH, Pickhardt PJ. Performing an additional decubitus series at CT colonography. Abdom Imaging. 2011; 36:538–544.
17. Gryspeerdt SS, Herman MJ, Baekelandt MA, van Holsbeeck BG, Lefere PA. Supine/left decubitus scanning: a valuable alternative to supine/prone scanning in CT colonography. Eur Radiol. 2004; 14:768–777.
18. Pickhardt PJ, Bakke J, Kuo J, Robbins JB, Lubner MG, del Rio AM, et al. Volumetric analysis of colonic distention according to patient position at CT colonography: diagnostic value of the right lateral decubitus series. AJR Am J Roentgenol. 2014; 203:W623–W628.
19. Lee JH, Park SH, Lee SS, Kim AY, Kim JC, Yu CS, et al. CT colonography in patients who have undergone sigmoid colostomy: a feasibility study. AJR Am J Roentgenol. 2011; 197:W653–W657.
20. Culligan K, Coffey JC, Kiran RP, Kalady M, Lavery IC, Remzi FH. The mesocolon: a prospective observational study. Colorectal Dis. 2012; 14:421–428. discussion 428-430




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download