Abstract
Objective
The maximum standardized uptake value (SUVmax) of pulmonary mucoepidermoid carcinoma (PMEC) in fluorine-18fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) was evaluated as a preoperative predictor of pathologic grade and survival rate.
Materials and Methods
Twenty-three patients who underwent preoperative PET/CT and complete resection for PMEC were enrolled. The optimal cut-off SUVmax for tumor grade was calculated as 6.5 by receiver operating characteristic curve. The patients were divided into a high SUV group (n = 7) and a low SUV group (n = 16). Clinicopathologic features were compared between the groups by χ2 test and overall survival was determined by Kaplan-Meier analysis.
Results
The mean SUVmax was 15.4 ± 11.5 in the high SUV group and 3.9 ± 1.3 in the low SUV group. All patients except one from the low SUV group had low grade tumors and all had no nodal metastasis. The sensitivity and specificity of SUVmax from PET/CT for predicting tumor grade was 85.7% and 93.8%, respectively. During the follow-up period (mean, 48.6 ± 38.7 months), four patients from the high SUV group experienced cancer recurrence, and one died of cancer. In contrast, none of the low SUV group had recurrence or mortality. Five-year overall survival rate was significantly higher in the low SUV group (100% vs. 71.4%, p = 0.031).
Conclusion
Pulmonary mucoepidermoid carcinoma patients with high SUVmax in PET/CT had higher tumor grade, more frequent lymph node metastasis and worse long-term outcome. Therefore, PMEC patients with high uptake on PET/CT imaging might require aggressive mediastinal lymph node dissection and adjuvant therapies.
Pulmonary mucoepidermoid carcinoma (PMEC) is a rare cancer that comprises only 0.1 to 0.2% of all primary lung malignancies (1,2,3,4). PMEC is classified as a salivary gland type lung carcinoma, which originates from the submucosal glands of the trachea and bronchus (5,6). Histologic grade, cancer stage and lymph node metastasis are reported independent factors for long-term prognosis in patients with PMEC (5). These prognostic factors, especially tumor grade, have been verified (3,7,8,9,10,11,12,13,14). It is now generally accepted that low-grade PMEC behaves like a benign or low-grade malignant tumor, while high-grade PMEC shows virulent characteristics like any other non-small cell lung cancer and has occasional lymph node metastasis. Therefore, if tumor grade could be predicted before surgery, it might reduce unnecessary lymph node dissection and even preserve lung function with limited pulmonary resection in patients with low-grade PMEC. On the other hand, in cases expected to have high-grade tumor, extended pulmonary resection with more radical lymph node dissection or neoadjuvant treatments could be performed. However, there is no diagnostic tool to predict tumor grade prior to surgery for PMEC.
This study evaluated whether the maximum standardized uptake value (SUVmax) of fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is a significant predictor for pathologic grade and postsurgical outcomes in patients following surgery for PMEC.
This retrospective study was approved by our hospital's Institutional Review Board. From 2005 to 2013, 27 patients (0.5% of all primary lung cancer patients) underwent complete resection with curative intent for PMEC. Four patients with PET/CTs taken at other hospitals or without studies prior to surgery were excluded from enrollment. Finally, 23 patients were enrolled. Their clinical records and surgicopathologic features were retrospectively reviewed.
Patients were instructed to fast for six hours prior to receiving 370 MBq (10 mCi) of 18F-FDG by intravenous injection. Forty-five minutes after the injection, PET/CT scans (GE Healthcare; Milwaukee, WI, USA) were performed. From 2005 to 2008, a Discovery LS scanner was used for PET/CT in eight patients. CT was performed at 140 keV, 40-120 mA, tube rotation time of 0.5 seconds per rotation, pitch of 6, and section thickness of 5 mm. From 2008 to 2013, a Discovery STe scanner was used for the other 15 patients, with CT performed at 140 keV, 30-170 mA, tube rotation time of 0.5 seconds per rotation, pitch of 6, and section thickness of 3.75 mm. PET data sets were reconstructed iteratively with an ordered subsets expectation-maximization algorithm and a segmented attenuation correction (two iterations, 28 subsets), and also with the CT data. Commercial software (Advantage Workstation version 4.4; GE Healthcare) was used to accurately co-register the separate CT and PET scan data. The SUVmax of the primary tumor was measured by the software. In brief, a volume-of-interest encircling the whole primary tumor was manually drawn, taking into account the CT, PET and fused PET/CT images, which allowed the software to automatically show the SUVmax of primary tumor.
Tumors were located in the segmental bronchi or lobar bronchus in 17 patients, main bronchus in five patients and trachea in one patient. Complete resection of the tumor (R0) was histologically confirmed in all subjects, and every operation also included mediastinal lymph node dissection. There were nine lobectomies, seven sleeve lobectomies, one bilobectomy, one sleeve bilobectomy, three pneumonectomies, one bronchial wedge resection, and one tracheal resection and anastomosis. Eighteen patients underwent pulmonary resection via open thoracotomy, and five patients underwent video-assisted thoracoscopic surgery (VATS).
The patients visited the outpatient clinic and had CT or PET/CT scans every three months for two years after surgery and then every six months for three more years. The patients visited the hospital annually after five years from the initial operation. Patient survival was reviewed, and the end date was defined as the latest follow-up date or the date of patient death. Disease-free survival was defined as the time between diagnosis and the first clinical or pathologic evidence of loco-regional or distant recurrent disease.
Histopathologic tumor grade was defined according to the grading system of the Armed Forces Institute of Pathology (15,16). Tumors that met the criteria for grade 1 were classified as low-grade tumors in our study. Similarly, tumors that met the grade 2 and 3 criteria were classified as high-grade tumors. Overall, there were 16 patients with low-grade tumors and seven patients with high-grade tumors (one patient with grade 2, six patients with grade 3). Pathologic staging was classified according to the 7th American Joint Committee on Cancer staging criteria.
All data were statistically analyzed using Stata Statistical Software 2007, Version 10 (StataCorp LP, College Station, TX, USA). SUVmax of the main tumor in PET/CT images was correlated with tumor grade. The optimal cutoff value was calculated as 6.5 by receiver operating characteristic (ROC) curve and area under curve was 0.92. The ROC curve is diagrammed in Figure 1. Patients with a SUVmax of 6.5 or higher were assigned to the high SUV group (n = 7) and the rest were assigned to the low SUV group (n = 16). We compared tumor grade, pathologic stage, and long-term outcomes between the low SUV group and the high SUV group. χ2 tests were performed for categorical variables, and unpaired t tests were performed for continuous variables. Overall survival was analyzed with Kaplan-Meier curves and the log-rank test.
The mean age was significantly higher in the high SUV group than the low SUV group (57.6 ± 11.7 years vs. 39.6 ± 17.2 years respectively, p = 0.010). Notably, all three patients under age 20 were included in the low SUV group and had a low grade tumor. The majority of patients (73.9%) had symptoms before surgery. Common symptoms were coughing (43.5%) and hemoptysis (30.4%). Most of the patients (87.0%) showed an Eastern Cooperative Oncology Group performance score of 0 or 1 and only three patients had a performance score of 2 (two patients from high SUV group and one patient from low SUV group). The mean SUVmax was 15.4 ± 11.5 in the high SUV group and 3.9 ± 1.3 in the low SUV group. The high SUV group had more high grade tumors (p < 0.001) and larger tumor sizes (43.6 ± 9.0 mm vs. 21.4 ± 3.0 mm, p = 0.003). Typical enhanced CT and PET/CT images of low SUV group are presented in Figure 2 and images of high SUV group in Figure 3. The high SUV group also had more frequent T3/4 stage (72.4% vs. 6.3%, p = 0.006), more frequent lymph node metastases (57.1% vs. 0%, p = 0.001), and consequently, higher cancer stages (stage I/II vs. III, p = 0.001) than the low SUV group. Enhanced CT and PET/CT images of the patient with regional lymph node metastasis are presented in Figure 4. The low SUV group had low grade tumors, except for one patient, and no lymph node metastasis. The sensitivity and specificity of PET/CT for predicting tumor grade were 85.7% and 93.8%, respectively. Accuracy was 91.3% and the positive and negative predictive value was 85.7% and 93.8%, respectively. Clinicopathologic characteristics are summarized in Table 1.
Length of follow-up was similar between the two groups (mean 48.6 ± 38.7 months; p = 0.660). In the high SUV group, four patients (57.1%) suffered cancer recurrence during follow-up, and one died of cancer 5 months after surgery. Another patient from high SUV group showed no evidence of cancer recurrence, but died of brain infarct during the follow-up. In contrast, none of the patients in the low SUV group experienced recurrence or mortality. As a result, the 5-year overall survival rate was significantly higher in the low SUV group than the high SUV group (100% vs. 71.4% respectively, p = 0.031). Three-year disease-free survival was also significantly higher in the low SUV group (100% vs. 17.9% respectively, p < 0.001). High grade tumor (p < 0.001), pathologic stage III (p < 0.001) and high SUV group (p < 0.001) were significant prognostic factors in univariate analysis. Multivariate analysis for long-term survival was unavailable, because there was no mortality or recurrence in patients with the low SUV group. Kaplan-Meier curves of overall and disease-free survival rates according to SUV group are diagrammed in Figure 5.
Since FDG-PET uptake in PMEC was first reported in a 5-year-old girl (17), several studies have addressed the subject. Case of low-grade PMEC without nodal metastasis and reported a SUVmax of 3.63 (18) and 6.2 (19). A case report involving high-grade PMEC with nodal metastasis reported a SUVmax of 7.4 (20). The SUVmax data from these studies precisely matches our results, further suggesting that a SUVmax higher than 6.5 indicates a possible high-grade tumor.
The correlation between SUVmax and histologic grade has been highlighted in several studies. SUVmax in salivary gland type carcinoma (including seven cases of PMEC) reportedly tends to be greater in high-grade tumors (21). Additionally, a recent study concerning surgical outcomes in 14 patients with PMEC, the median SUVmax increased significantly along with tumor grade (p = 0.041) (14). Presently, PET revealed significant differences (p < 0.001) in tumor grade according to SUV group.
The association of SUVmax with long-term survival remains unclear. High FDG uptake has been associated with more frequent nodal or distant metastases, but failed to predict long-term survival (22). However in this study, PET/CT data was available in 11 patients (36.7%) and other subtypes of salivary gland type lung cancer were included. Presently, nodal metastasis was significantly associated with the high SUV group (p = 0.001). Furthermore, overall and disease-free survivals were significantly better in the low SUV group. To our knowledge, this is the first study to report the prognostic value of FDG-PET/CT for long-term outcomes in PMEC patients.
The low SUV group had good long-term prognosis without recurrence after complete resection of tumor. In contrast, despite complete resection, the high SUV group suffered from local or distant recurrence. In the high SUV group, four patients received adjuvant chemotherapy, but two patients had distant metastasis. These results are similar to the prior conclusion that adjuvant chemotherapy does not seem to be effective in high grade PMEC (23).
The most common site of PMEC in the tracheobronchial tree is the segmental bronchi, which are located within the lung parenchyma. In the present study, nine patients (56.3%) in the low SUV group underwent simple lobectomies, and five of these simple lobectomies were performed by VATS. Even in patients who required sleeve resection of the bronchus, VATS could be attempted. Use of VATS sleeve lobectomy in low-grade PMEC in the left main bronchus has been described (24). Therefore, in selected patients with low PET/CT uptake, VATS represents a feasible and effective surgical option.
Limitations in this study include the retrospective design and very small number of patients. Considering the rarity of PMEC, multi-center studies with large number of cases are needed to reconfirm and support the results of this study. Another limitation is that the change in PET/CT device once during follow-up might have caused alteration of SUVmax, although the differences were likely minimal.
In conclusion, 18F-FDG PET/CT appears to be a useful preoperative imaging modality for predicting tumor grade, nodal stage and postsurgical prognosis. Patients with a SUVmax greater than 6.5 were more likely to have a high-grade tumor, lymph node metastasis and cancer recurrence. Therefore, PMEC patients with high uptake on PET/CT imaging might require aggressive mediastinal lymph node dissection and adjuvant therapies. Further studies with more cases of PMEC are necessary to verify the validity of PET/CT for prediction of long-term prognosis.
Figures and Tables
Fig. 1
Receiver operating characteristics (ROCs) curve for maximum standardized uptake value (SUVmax) for prediction of tumor grade of pulmonary mucoepidermoid carcinoma.
Optimal cut-off value of SUVmax from PET/CT was calculated as 6.5 by ROCs curve. Area under curve for SUVmax was 0.92 and sensitivity and specificity for predicting tumor grade were 85.7% and 93.8%, respectively. PET/CT = positron emission tomography/computed tomography
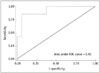
Fig. 2
Chest CT and PET/CT results for 17-year-old female with PMEC in low SUV group.
A. In CT image, 14 mm intraluminal nodule (arrow) obliterated lumen of right middle lobar bronchus and protruded into lumen of intermediate bronchus. B. SUVmax of tumor in PET/CT was 4.2 (arrow) and pathologic result verified stage IA low grade PMEC. CT = computed tomography, PET/CT = positron emission tomography/computed tomography, PMEC = pulmonary mucoepidermoid carcinoma, SUV = standardized uptake value, SUVmax = maximum SUV

Fig. 3
Chest CT and PET/CT results for 67-year-old male with PMEC in high SUV group.
A. In CT image, 53 mm mass (arrow) in left upper lobe with possibility of chest wall invasion was visible. B. SUVmax of tumor in PET/CT was 11.9 (arrow) and pathologic result verified stage IIB high grade PMEC. CT = computed tomography, PET/CT = positron emission tomography/computed tomography, PMEC = pulmonary mucoepidermoid carcinoma, SUV = standardized uptake value, SUVmax = maximum SUV

Fig. 4
Nodal metastasis of PMEC on chest CT and PET/CT in 68-year-old female.
A. In CT image, 10 cm large mass (arrow) was evident in right upper lobe and mediastinal lymph nodes in para-tracheal area (arrowhead) were enlarged, representing possible nodal metastases. B. In PET/CT, SUVmax of mass was 13.1 (arrow) and slightly increased uptake in right para-tracheal lymph nodes (SUVmax = 2.9, arrowhead) were seen. Pathologic results revealed high grade PMEC with single metastasis in right lower para-tracheal lymph node representing stage IIIA. CT = computed tomography, PET/CT = positron emission tomography/computed tomography, PMEC = pulmonary mucoepidermoid carcinoma, SUVmax = maximum standardized uptake value

Fig. 5
Kaplan-Meier overall and disease-free survival of 23 patients after complete resection for PMEC according to SUV group.
Overall survival (A) was significantly higher in low SUV group than high SUV group (5-year survival rates of 100% vs. 71.4%, p = 0.031). Disease-free survival (B) was also significantly higher in low SUV group (3-year survival rates of 100% vs. 17.9%, p < 0.001). PMEC = pulmonary mucoepidermoid carcinoma, SUV = standardized uptake value

Table 1
Clinicopathologic Characteristics of Patients with PMEC According to SUV Group

References
1. Turnbull AD, Huvos AG, Goodner JT, Foote FW Jr. Mucoepidermoid tumors of bronchial glands. Cancer. 1971; 28:539–544.
2. Leonardi HK, Jung-Legg Y, Legg MA, Neptune WB. Tracheobronchial mucoepidermoid carcinoma. Clinicopathological features and results of treatment. J Thorac Cardiovasc Surg. 1978; 76:431–443.
3. Heitmiller RF, Mathisen DJ, Ferry JA, Mark EJ, Grillo HC. Mucoepidermoid lung tumors. Ann Thorac Surg. 1989; 47:394–399.
4. Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol. 2005; 40:90–97.
5. Yousem SA, Hochholzer L. Mucoepidermoid tumors of the lung. Cancer. 1987; 60:1346–1352.
6. Klacsmann PG, Olson JL, Eggleston JC. Mucoepidermoid carcinoma of the bronchus: an electron microscopic study of the low grade and the high grade variants. Cancer. 1979; 43:1720–1733.
7. Chin CH, Huang CC, Lin MC, Chao TY, Liu SF. Prognostic factors of tracheobronchial mucoepidermoid carcinoma--15 years experience. Respirology. 2008; 13:275–280.
8. Xi JJ, Jiang W, Lu SH, Zhang CY, Fan H, Wang Q. Primary pulmonary mucoepidermoid carcinoma: an analysis of 21 cases. World J Surg Oncol. 2012; 10:232.
9. Zhu F, Wang W, Hou Y, Shi J, Liu Z, He D, et al. MAML2 rearrangement in primary pulmonary mucoepidermoid carcinoma and the correlation with FLT1 expression. PLoS One. 2014; 9:e94399.
10. Vadasz P, Egervary M. Mucoepidermoid bronchial tumors: a review of 34 operated cases. Eur J Cardiothorac Surg. 2000; 17:566–569.
11. Song Z, Liu Z, Wang J, Zhu H, Zhang Y. Primary tracheobronchial mucoepidermoid carcinoma--a retrospective study of 32 patients. World J Surg Oncol. 2013; 11:62.
12. Kang DY, Yoon YS, Kim HK, Choi YS, Kim K, Shim YM, et al. Primary salivary gland-type lung cancer: surgical outcomes. Lung Cancer. 2011; 72:250–254.
13. Molina JR, Aubry MC, Lewis JE, Wampfler JA, Williams BA, Midthun DE, et al. Primary salivary gland-type lung cancer: spectrum of clinical presentation, histopathologic and prognostic factors. Cancer. 2007; 110:2253–2259.
14. Lee GD, Kang do K, Kim HR, Jang SJ, Kim YH, Kim DK, et al. Surgical outcomes of pulmonary mucoepidermoid carcinoma: a review of 23 cases. Thorac Cardiovasc Surg. 2014; 62:140–146.
15. Brandwein MS, Ivanov K, Wallace DI, Hille JJ, Wang B, Fahmy A, et al. Mucoepidermoid carcinoma: a clinicopathologic study of 80 patients with special reference to histological grading. Am J Surg Pathol. 2001; 25:835–845.
16. Goode RK, Auclair PL, Ellis GL. Mucoepidermoid carcinoma of the major salivary glands: clinical and histopathologic analysis of 234 cases with evaluation of grading criteria. Cancer. 1998; 82:1217–1224.
17. Kinoshita H, Shimotake T, Furukawa T, Deguchi E, Iwai N. Mucoepidermal carcinoma of the lung detected by positron emission tomography in a 5-year-old girl. J Pediatr Surg. 2005; 40:E1–E3.
18. Ishizumi T, Tateishi U, Watanabe S, Maeda T, Arai Y. F-18 FDG PET/CT imaging of low-grade mucoepidermoid carcinoma of the bronchus. Ann Nucl Med. 2007; 21:299–302.
19. Lee EY, Vargas SO, Sawicki GS, Boyer D, Grant FD, Voss SD. Mucoepidermoid carcinoma of bronchus in a pediatric patient: (18)F-FDG PET findings. Pediatr Radiol. 2007; 37:1278–1282.
20. Kuzucuoglu M, Karamustafaoglu YA, Cicin I, Yoruk Y. A rarely seen mucoepidermoid carcinoma of the left main bronchus. J Cancer Res Ther. 2014; 10:384–386.
21. Jeong SY, Lee KS, Han J, Kim BT, Kim TS, Shim YM, et al. Integrated PET/CT of salivary gland type carcinoma of the lung in 12 patients. AJR Am J Roentgenol. 2007; 189:1407–1413.
22. Elnayal A, Moran CA, Fox PS, Mawlawi O, Swisher SG, Marom EM. Primary salivary gland-type lung cancer: imaging and clinical predictors of outcome. AJR Am J Roentgenol. 2013; 201:W57–W63.
23. Yang CS, Kuo KT, Chou TY, Lin CM, Hsu WH, Huang MH, et al. Mucoepidermoid tumors of the lung: analysis of 11 cases. J Chin Med Assoc. 2004; 67:565–570.
24. Santambrogio L, Cioffi U, De Simone M, Rosso L, Ferrero S, Giunta A. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest. 2002; 121:635–636.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download