Abstract
Objective
The aim of the present study was to determine the prevalence and reporting rate of incidental findings (IF) in adult outpatients undergoing lumbar magnetic resonance imaging (MRI).
Materials and Methods
Re-evaluation of a total of 1278 lumbar MRI images (collected from patients with a mean age of 50.5 years, range 16-91 years) captured between August 2010-August 2011 was done by a neuroradiologist and a musculoskeletal radiologist. IFs were classified according to organ or system (liver, gallbladder, kidney, bladder, uterus, ovary, lymph node, intestine and aorta). The rate of reporting of a range of IF was examined. The outcome of each patient's treatment was evaluated based on review of hospital records and by telephone interviews.
Results
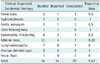
A total of 253 IFs were found in 241 patients (18.8% of 1278). Among these, clinically significant IFs (n = 34) included: 2 renal masses (0.15%), 2 aortic aneurysms (0.15%), 2 cases of hydronephrosis (0.15%), 11 adrenal masses (0.86%), 7 lymphadenopathies (0.55%), 6 cases of endometrial or cervical thickening (0.47%), 1 liver hemangioma (0.08%), 1 pelvic fluid (0.08%) and 2 ovarian dermoid cysts (0.15%). Overall, 28% (71/253) of IFs were included in the clinical reports, while clinically significant findings were reported in 41% (14/34) of cases.
Incidental findings (IF) are usually asymptomatic abnormalities other than expected pathologies, which are encountered during radiological examinations. In recent years, advances in digital evaluation of radiological imaging (e.g., high magnification zoom, the ability to focus on individual images, and digital archiving) have dramatically improved detection limit of incidental lesions (1). There are studies that reviewed the frequency of IF, legal issues and the cost issue depending on additional requirements of investigation (123456). Lee et al. (5) reported that 4.6% of IF are clinically significant in lumbar computed tomography (CT) scans (renal mass, aortic aneurysm, lymphadenopathy). According to this result, it is evident that the majority of IF (> 95%) harbor little clinical significance. However, careful observation of anatomic structure outside of the immediate region of interest creates opportunities for early detection of potentially life threatening conditions such as malignancies and aneurysms (78). On the other hand, Quattrocchi et al. (9) were the first to use modified CT colonography reporting and data system (C-RADS) to report a wide variety of incidental extraspinal pathologies found during lumbar magnetic resonance (MR) examinations. This study reported a high rate of IF using the C-RADS system (68.6%). Some studies also suggest that localizer images (low-resolution series, which are used at the planning process of the imaging) may be useful in detecting IF (110). The aim of this study was to investigate the prevalence and reporting rates of extraspinal IF in routine lumbar MR examinations.
The retrospective study was approved by the local ethics committee. Due to the nature of the study design, there was no need to obtain specific informed consent from patients. Lumbar MR images obtained between August 2010 and August 2011 were reassessed from the imaging archive. A neuroradiologist with 7 years of experience and a musculoskeletal radiologist completed the assessments and recorded consensus findings during the same session. In case of dispute, opinion was taken from an experienced body radiologist (with experience of 10 years). Patients who were admitted with complaints of back or leg pain or numbness and whose images were collected during elective procedures were included in the study. Children under 16 years of age and patients with known malignancies were excluded from the study. Extraspinal IF, which include anatomical variants and anomalies (retroaortic renal vein [RARV], horse-shoe kidney, etc.), solid organ cysts (liver, kidney, etc.), the pathologies of reproductive system (ovarian cysts, uterine fibroids, endometrial thickening, etc.), tumoral lesions (liver hemangioma, renal and adrenal mass, etc.), hydronephrosis, aortic aneurysm, gallbladder stone, bowel diverticulosis and demographic data were recorded in an Excel spreadsheet. IF were classified according to organ or system (liver, gallbladder, kidney, bladder, uterus, ovary, lymph node, intestine and aorta). Clinically significant findings (E3 and E4 according to modified C-RADS classification), anatomic variations (C-RADS E1) and benign conditions (C-RADS E2) were noted during the review of the reports (9). Localizer images were excluded from the study, as these images are not evaluated in our daily practice due to low quality of image and high time demand. We have acquired the entire clinical information through chart review. In cases of clinical significance (such as aortic aneurysm, abnormal endometrial thickening, mass lesions or large cysts) that lacked hospital records, information about the treatment was obtained via telephonic conversation.
MR examinations were performed using a 1.5-T MR unit (Signa; GE Medical System, Milwaukee, WI, USA) with an 8-channel spinal coil. Our routine lumbar spinal MR protocol includes sagittal T1-weighted (repetition time [TR]/echo time [TE], 600/8-23 ms; matrix, 416 x 224; field of view [FOV], 28 cm; echo train length [ETL], 3), sagittal T2-weighted (TR/TE, 2540/85 ms; matrix, 416 x 224; FOV 28 cm; ETL, 23), and axial T2-weighted (TR/TE 3360/85 ms; matrix, 320 x 224; FOV, 20 cm; ETL, 23) sequences. The axial section images were taken between the L1 and S1 vertebrae. In all sequences, 4-mm slice thickness with a 1-mm inter-slice gap and number of excitations 4 was used. The presaturation band has only been applied in sagittal series.
The mean age of patients in our study was 50.5 years (range 16-91 years). After excluding repeat MR study belonging to the same patient, there were a total of 1334 studies in the imaging archives. Of those images, 22 were excluded from the study due to the patients being less than 16 years old, 3 cases were excluded due to low quality or incomplete imaging, and 31 images were excluded due to the presence of known malignancy. Out of a total number of 1278 patients, 485 were men (37.9%) and 793 were women (62.1%).
About 80% (9/11) of renal cysts were reported to be larger in size (> 5 cm), while rate was only 15% (11/71) in smaller sized cysts (< 5 cm). A similar situation was seen in ovarian cysts: the reporting rate was 50% (2/4) for cysts larger than 5 cm, while the reporting rate was only 29% (7/24) if the cyst was smaller than 5 cm. Alternately, a 50% (18/36) reporting rate was found for fibroids smaller than 4 cm (Fig. 1C). A diagnosis of dermoid cyst was confirmed after surgery in two ovarian cyst cases (one 7 cm in diameter and the other 8 cm in diameter) that were identified as dermoid cysts based on radiological evaluation (Fig. 1A). The surgical record regarding one of these cases was not available in the hospital records and the patient could not be reached by phone.
A ureteral stone was detected in one of the patients with hydronephrosis (Fig. 2C). The findings were mentioned in the clinical reports and an ultrasonography examination was recommended. Thus, the etiology was also revealed by two IFs.
The presence of a renal mass was detected in two cases. In one of the patients, the positron emission tomography (PET) examination revealed a mass in the lung and brain metastasis and one month later the patient died. Meanwhile, nodular lesion in the retroperitoneal area was detected in the other case (Fig. 3) and this patient had 2 IFs. The hospital records contained no record of the surgical intervention in this case and the patient could not be reached by phone.
Endometrial and cervical thickenings were reported at a rate of 50% (3/6) in our data set. One of these cases resulted in a diagnosis of endometrial polyps. In the same case, there were renal cyst 2.5 cm in diameter as the second IF and it had not been reported. In other cases there was no pathology detected in the follow-up evaluations (Fig. 1B).
Furthermore, we determined that in 3 cases, liver cysts and 8 millimeter-sized calculi were unreported (Fig. 2B). However, a large lesion (8.5 cm) that was assessed as hemangioma was reported and ultrasonography was recommended (Fig. 2A). There was no problem through the follow-up.
Out of 11 cases with detected adrenal mass, 4 cases were noted in the report. Liver cyst was present in one of those cases, although PET examination indicated no involvement. Another case included a history of femur fracture after a fall. MR examination of this patient revealed the presence of an aneurysm (36 mm in diameter) and lung nodules; additional brain metastases were detected during the period of hospitalization and the patient died during the hospital stay (Fig. 2E). This patient was also a unique case that had 3 IFs including renal cyst. There were no problems during follow-up in the remaining cases evaluated for IF.
Abdominal aortic aneurysms were detected in two patients. In one of these cases, the aneurysm (47 mm in diameter) was not specified in the report and it was determined that there were no problems in the follow-up examination (Fig. 2D). The second case involved a patient being examined for an adrenal mass, as discussed above.
A male patient with small amount of free fluid in the pelvis was suffering from multiple sclerosis. The accumulation of pelvic fluid was detected during the hospital stay, but not mentioned in the report. However, the follow-up was uneventful.
A case with a cyst measuring 2 cm in diameter in the anterior of the psoas muscle in the retroperitoneal tissue went unmentioned in the official report. Furthermore, no further intervention or examinations were indicated in this patient's records.
In general, a total of 241 patients had IFs. In terms of the distribution of cases, 230 patients had only 1 IF, 10 patients had 2 IFs, while 1 patient had 3 IFs. Out of 11 patients with more than one IF, 4 clinically significant cases are explained above. The others were clinically unimportant cases with small renal cysts, uterine fibroids, horseshoe kidney, RARV and bladder wall thickening.
The overall IF prevalence in our dataset was 19.8% (Table 1). This rate is less than the values reported in the literature. Cases involving renal cysts, ovarian cysts, and fibroids measuring 1-1.5 cm were not included in our study. Previous studies (59) apparently included all cystic structures and fibroids regardless of size.
Findings related to anatomical variation and lesions that had no effect on the patient's clinical course (renal cyst < 5 cm, fibroid < 4 cm, ovarian cyst < 5 cm, etc.) were not mentioned in the clinical report in 72% of cases. This did not result in any disruption in patient management due to lack of clinical significance. Moreover, RARV variation was not specified in the Quattrocchi's study (9).
Similar to other published reports, we observed that the renal findings made up the largest proportion of IF (37%). There was a greater tendency to report renal cysts > 5 cm in diameter (80% > 5 cm were reported and 15% of cysts < 5 cm were reported). Small cysts are not clinically significant, but large cysts (> 6 cm) are potentially indicative of sclerotherapy by percutaneous treatment with ultrasonography (11). Anomalies and pathological conditions are most commonly reported. The detection of asymptomatic hydronephrosis or atrophy of one kidney is essential in addressing potential health problems in the other kidney.
Xiong et al. (7) evaluated 18 studies, reporting high variance (0.15-7.5%) in the detection of aneurysms during CT colonography. The aneurysm rate in our dataset (0.15%) was similar to the report by Pickhardt et al. (12) in which 1233 cases of CT colonography were examined. However, the aneurysm rate in our data set was lower than that reported by Quattrocchi et al. (9) (0.6%). The average patient age was relatively low in our study; however, the evaluation of other potentially relevant factors such as genetic and environmental variables was beyond the scope of the current study. We assume that the values do not reflect the true prevalence of aneurysms because the lumbar magnetic resonance imaging (MRI) has limited field of image and is not a screening method. One of two cases of aneurysms was not specifically discussed in the report, but in both cases, dilation of the aorta < 55 mm indicated the need for urgent intervention. The incidence of aneurysm increases with advanced age, and the abdominal aorta should be examined during routine lumbar MR evaluations in older patients.
Lymphadenopathies were generally not reported in cases where the short axis was less than 1 cm and the long axis was greater than 1 cm. Several cases that were excluded from our study due to the presence of primary malignancies involved larger lymphadenopathies that were mentioned in the clinical report. We recommend that spherical lymph nodes with short axis larger than 1 cm should be closely monitored for the possibility of malignancy.
Quattrocchi et al. (9) observed a 20% incidence of diverticulosis in their publication. Our dataset included one case of diverticulosis. This difference in diverticulosis incidence may be due to the lower average age of the patients in our study and regional dietary differences (incidence of constipation). In addition, they reported only a single case of adrenal solid lesion. The higher frequency of adrenal solid lesions in our dataset may be due to the difference in techniques; we captured axial sections at the upper lumbar level (descending from the L1 vertebra), a highly effective technique in our experience. The study by Quattrocchi et al. (9) does not specify the location of the axial sections. The overall prevalence of IF in our study was consistent with previous reports in the literature (0.6-1.5%) (13).
In our study, approximately 5% of patients with IF (11/241) had more than one IF. As seen in our series, it is necessary not to omit ureteral stone in patients with hydronephrosis, retroperitoneal node in patients with renal mass, and adrenal mass in patients with aortic aneurysm. Although clinically insignificant conditions are mostly encountered, the detection of IF in important cases as mentioned earlier can contribute greatly to patient management.
Lumbar MRI is not a screening method, and the vast majority of clinical findings are not of clinical significance. However, Xiong et al. (7) reported that the prevalence of incidental extracolonic cancer in their CT colonography examinations (2549 cases, 24 early stage cancer) was no lower than the incidence of cancer detected by some specific cancer screening methods. Similarly, a lumbar MR study of 3000 patients conducted by Quattrocchi et al. (9) reported 4 solid renal lesions, and 7 incidents of colorectal wall thickening. In another summary of lumbar CT findings, 2 renal masses and 1 mesenteric mass were detected among a group of 400 patients. Meanwhile in the present study, two renal masses and two ovarian dermoid cysts were observed; one of these was later confirmed by surgery.
Quattrocchi et al. (9) indicated that 90% of IF, including cases with clinical significance, are not commonly included in the clinical reports. The same was true in our data set, although the overall rate of unreported IF was lower (72%). The rate of reporting of IF is significant for professional liability and other legal concerns (23). The lack of sufficient time for the evaluation of imaging data, the absence of sufficient clinical information, and various distractions present in the work environment are important factors that influence the rate of IF reporting.
Detailed protocols for reporting IF such as the C-RADS system (14) might be useful in routine lumbar MR imaging, but are often difficult for practical purpose. Classifications generally allow objective assessment. However, we think it is a deficit that cyst size (large cysts) and types (such as dermoid cyst) are not specified in the C-RADS and modified C-RADS classifications. We suggest that the findings in the C-RADS E3 and E4 groups should be noted in the report. Nevertheless, we believe that the situations like large cysts and cholelithiasis should not be considered unimportant, in spite of belonging to the E2 group. Furthermore, additional radiological imaging can be recommended in the report (such as ultrasonography for cholelithiasis).
We agree with previous studies (110) suggesting that evaluation of localizer images may be useful for the detection of clinically significant incidental pathologies (Table 2). However, the clinical efficacy of localizer images in daily practice is debatable due to the poor quality of acquired images.
The number of female patients was higher in our study, which is similar to the literature. The rate of lumbar MRI request is higher in women because coexisting undefined symptoms and uncertain neurological findings are more common in female patients.
Although clinically significant findings are identified, their situation of 'to be critical' is seen only as a possibility unless proven with follow-up or additional examination. As an indicator to that, the conditions such as adrenal lesions, lymphadenopathy, endometrial thickening, pelvic free fluid, bladder wall thickening, solid lesions of liver did not cause clinical problems through the follow-up in our study. The prospective studies including the large number of patients in which the clinical significance of IF is determined in real terms with the follow-up and further investigation are needed for objective review.
In our country, MR examination has become a routine component of clinical examination, with costs lower than in many European countries. A large number of MR imaging is prescribed regardless of clinical indication. The high volume of imaging requests results in unnecessary congestion in radiologic imaging facilities and increases the cost of medical care. It is hypothesized that accurate and effective communication between patients, radiologists, and clinicians can help to resolve these issues.
The retrospective design of our study may be considered a significant limitation. In addition, the clinical reports used in the analysis were filed by independent radiologists, leading to wide variation in the reporting of IF. The cost analysis depending on additional investigations and the stress effect on the patient during the follow-up of the identified findings were not investigated and not all images were examined by abdominal radiologist. Our data set included only two cases (one with renal mass and the other with an initial diagnosis of dermoid cyst) that were clinically significant, and we were unable to obtain additional information on these cases through our hospital records or by contacting the patients or their families. To the best of our knowledge, the current study is among the broadest reports of IF in lumbar MR examinations. In addition, this study has determined the size-specific reporting rate of benign cystic lesions.
Regardless of whether IFs are clinically significant, the inclusion of IF in the clinical report is an indicator that the radiologist performed a thorough examination of the imaging data. Although the description of benign IF may contribute to anxiety in some patients, it does not create additional legal issues. Moreover, if IFs are not reported in potential life-threatening situations, serious legal ramifications may apply. It is an important issue to be considered that clinically important findings are omitted in our study in a high rate. We believe that individual and organizational measures must be taken to provide adequate attention during the reporting process. The studies from different centers (academic and community) with wider participation will provide information on the prevalence of the condition.
In conclusion, the IFs are common in routine lumbar MRI although clinically significant IFs were uncommon. Clinically significant IFs are occasionally omitted from formal clinical reports. Therefore, a systematic evaluation of spinal and non-spinal structures in lumbar MR images might be of importance in daily practice.
Figures and Tables
 | Fig. 1Sample images from genital system.
A. Ovarian dermoid cyst (hyperintense lesion [arrow] on sagittal T1-weighted image) with central dermoid nodule (asterisk), which is verified after surgery. B. Endometrial thickening (asterisk). C. Uterine fibroid (encircled) on T2-weighted sagittal images.
|
 | Fig. 2Pathologies of hepatobiliary, urinary, vascular system and adrenal mass.
A. Hepatic hemangioma (arrow). B. Gallbladder stone (arrow). C. Unilateral hydronephrosis (arrow). D. Aortic aneurysm (asterisk). E. Ovoid hyperintense adrenal mass lesion (asterisk) on T2-weighted axial images.
|
 | Fig. 358-year-old man with three incidental pathologies.
A. Renal mass on left kidney and paraaortic enlarged lymph node (arrows). B. Retroperitoneal nodular lesion (arrow) on axial T2-weighted images.
|
Table 1
Summary of Incidental Findings and Reporting Rates

Table 2
Clinical Important Incidental Findings and Reporting Rates
References
1. Wagner SC, Morrison WB, Carrino JA, Schweitzer ME, Nothnagel H. Picture archiving and communication system: effect on reporting of incidental findings. Radiology. 2002; 225:500–505.
2. Fileni A, Magnavita N. A 12-year follow-up study of malpractice claims against radiologists in Italy. Radiol Med. 2006; 111:1009–1022.
3. Magnavita N, Magnavita G, Fileni A, Bergamaschi A. Ethical problems in radiology: medical error and disclosure. Radiol Med. 2009; 114:1345–1355.
4. Park HJ, Jeon YH, Rho MH, Lee EJ, Park NH, Park SI, et al. Incidental findings of the lumbar spine at MRI during herniated intervertebral disk disease evaluation. AJR Am J Roentgenol. 2011; 196:1151–1155.
5. Lee SY, Landis MS, Ross IG, Goela A, Leung AE. Extraspinal findings at lumbar spine CT examinations: prevalence and clinical importance. Radiology. 2012; 263:502–509.
6. Hlatky MA, Iribarren C. The dilemma of incidental findings on cardiac computed tomography. J Am Coll Cardiol. 2009; 54:1542–1543.
7. Xiong T, Richardson M, Woodroffe R, Halligan S, Morton D, Lilford RJ. Incidental lesions found on CT colonography: their nature and frequency. Br J Radiol. 2005; 78:22–29.
8. Konnak JW, Grossman HB. Renal cell carcinoma as an incidental finding. J Urol. 1985; 134:1094–1096.
9. Quattrocchi CC, Giona A, Di Martino AC, Errante Y, Scarciolla L, Mallio CA, et al. Extra-spinal incidental findings at lumbar spine MRI in the general population: a large cohort study. Insights Imaging. 2013; 4:301–308.
10. Kamath S, Jain N, Goyal N, Mansour R, Mukherjee K. Incidental findings on MRI of the spine. Clin Radiol. 2009; 64:353–361.
11. Baysal T, Soylu A. Percutaneous treatment of simple renal cysts with n-butyl cyanoacrylate and iodized oil. Diagn Interv Radiol (Ank). 2009; 15:148–152.
12. Pickhardt PJ, Choi JR, Hwang I, Butler JA, Puckett ML, Hildebrandt HA, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003; 349:2191–2200.
13. Dahnert W. Radiology review manual. 4th ed. Baltimore: Williams & Wilkins;1999. p. 759.
14. Zalis ME, Barish MA, Choi JR, Dachman AH, Fenlon HM, Ferrucci JT, et al. CT colonography reporting and data system: a consensus proposal. Radiology. 2005; 236:3–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download