Abstract
Objective
To evaluate the rates of technical success, clinical success, and complications of fluoroscopy-guided lumbar cerebrospinal fluid drainage.
Materials and Methods
This retrospective study was approved by the Institutional Review Board of our hospital, and informed consent was waived. Ninety-six procedures on 60 consecutive patients performed July 2008 to December 2013 were evaluated. The patients were referred for the fluoroscopy-guided procedure due to failed attempts at a bedside approach, a history of lumbar surgery, difficulty cooperating, or obesity. Fluoroscopy-guided lumbar drainage procedures were performed in the lateral decubitus position with a midline puncture of L3/4 in the interspinous space. The catheter tip was positioned at the T12/L1 level, and the catheter was visualized on contrast agent-aided fluoroscopy. A standard angiography system with a rotatable C-arm was used. The definitions of technical success, clinical success, and complications were defined prior to the study.
Results
The technical and clinical success rates were 99.0% (95/96) and 89.6% (86/96), respectively. The mean hospital stay for an external lumbar drain was 4.84 days. Nine cases of minor complications and eight major complications were observed, including seven cases of meningitis, and one retained catheter requiring surgical removal.
Cerebrospinal fluid (CSF) drainage has been historically used to relieve intracranial pressure or to control a CSF fistula, otorrhea, or rhinorrhea. Lumbar access is a safe and efficacious route for draining CSF (123). Due to its simplicity, initial CSF drainage attempts are widely performed at the bedside. However, technical failure can occasionally occur, with incorrect placement of the catheter due to "blind" maneuvering. Previous studies have described the use of fluoroscopic or computed tomography (CT)-guided techniques to overcome blind access to the thecal sac (4567). Although the technical success rate of fluoroscopic-guided lumboperitoneal shunt, which shares a procedure with fluoroscopic-guided external lumbar drainage, has been described with a small number of patients, overall technical or clinical success and complication rates of fluoroscopic-guided external lumbar drainage have not been reported (7). Therefore, the purpose of this single-arm study was to report the technical success, clinical success, and complications rates of a fluoroscopic-guided lumbar drainage procedure in patients in whom a blind bedside approach for draining CSF is difficult to perform.
This retrospective study was approved by the Institutional Review Board of our hospital, and informed consent was waived.
Lumbar CSF drainage is initially attempted at bedside according to the standard care protocol of our hospital. Patients who fail attempts at the bedside approach or who have a history of lumbar surgery, difficulty cooperating, or obesity (body mass index ≥ 30 kg/m2), are referred to the radiological department for a fluoroscopic-guided procedure. This study included 96 consecutive fluoroscopic-guided lumbar drainage procedures of 60 patients (age range, 22-88 years; mean age, 62.1 years; 24 males and 36 females) who underwent the procedure between July 2008 and December 2013. The indications for lumbar drainage in this difficult patient group are listed in Table 1. Mean hospital stay for the lumbar drainage catheter was 4.84 days (range, 0-13 days).
All procedures were conducted by fellow or staff radiologists who specialize in musculoskeletal disorders and had 1-10 years of experience. The patient was positioned in the left or right lateral decubitus position on a radiolucent operating table, and the puncture site was fluoroscopically confirmed using a standard angiography system with a rotatable C-arm (RF-1000-125; Philips Inc., Andover, MA, USA). A midline approach to the L3/4 interspinous space was preferred in most cases to avoid repeated puncture, as the L4/5 and L5/S1 interspinous spaces pose a greater risk of degenerative changes in our experience. The skin was prepped with Povidone-iodine solution and draped in a sterile fashion. After marking the skin puncture site with mosquito forceps, and administering 1% lidocaine locally, a 2-3 cm deep puncture was attempted initially without fluoroscopic guidance using an 18-gauge × 80-mm Tuohy needle. If this attempt failed, the needle tip was advanced gently under fluoroscopic guidance with lateral and antero-posterior (AP) views. When the needle tip traversed the spinolaminar line, which is a landmark of the posterior wall of the dura, the needle was advanced cautiously. The dura was punctured with a snap or rotation to avoid tenting the dura. Once CSF was encountered, contrast media was infused to confirm access to the subarachnoid space after removing the stylet. Diffuse spreading of the contrast media was typically observed after a successful puncture. If the needle was in the epidural space, the typical radiological findings were an irregularly shaped contrast pattern, with multifocal filling defects on the AP view, with contrast flowing along the spinolaminar line in the lateral view (Fig. 1). If the needle was in the subdural space, a typical "railroad track appearance" may be seen on the AP view and a thin linear line of contrast is seen on the lateral view (Fig. 2). The Tuohy needle was rotated to orient the bevel in the cranial direction, and the catheter was advanced 10-15 cm, slowly without resistance. If any resistance was encountered while advancing the catheter, the procedure was stopped, and contrast agent was used to confirm the location of the catheter tip and whether there was kinking or looping in the catheter. Finally, the level of the catheter tip was confirmed with contrast agent, which was usually positioned at the T12/L1 level. After connecting the drainage circuit to the catheter, the drain site was dressed with dry gauze and secured with transparent dressing (Tegaderm; 3M Health Care, St. Paul, MN, USA).
One radiologist (second year resident) retrospectively reviewed the electronic medical records (EMRs) of the patients during their in hospital stay to assess the technical success and complication rates of the lumbar drainage. We predefined technical and clinical success prior to the study. The following four conditions were required for technical success: 1) confirmation of CSF through the puncture needle, 2) diffuse spread of contrast media into the subarachnoid space, 3) advance of the catheter by 10-15 cm without kinking or hairpin looping of the catheter tip, and 4) no intraprocedural complications, such as intradural or extradural hemorrhage, breakage of the catheter drainage system during manipulation, or pain severe enough to interrupt the procedure. Clinical success was defined as no clinical need for re-inserting the lumbar drainage catheter within 24 hours, with the exception of removal by the patient. If the system stopped draining, the catheter was adjusted or pulled back at the bedside before requesting re-insertion.
The complications documented in the EMRs after fluoroscopic-guided lumbar drainage were analyzed. The diagnosis of clinical meningitis associated with lumbar external drainage was made using the following criteria: 1) no preceding meningitis before inserting the lumbar drain, 2) continuous lumbar drainage ≥ 24 hours before the CSF analysis, and 3) CSF pleocytosis (white blood cell [WBC] count ≥ 11 cells/mm3), with or without a positive culture from the lumbar drain CSF specimen. Itching and oozing were considered complications only if they required early removal or re-insertion of the drain.
The technical success rate was 99.0% (95% confidence interval [CI], 94.3-99.8%), and the clinical success rate was 89.6% (95% CI, 81.9-94.2%). On case of technical failure was encountered as a loop that formed in the catheter (Fig. 3), which was detected the day after the procedure. The catheter was removed and successfully re-inserted without any complications.
Insufficient CSF drainage was identified in 10 cases, including one case of technical failure in which the lumbar drain had to be re-inserted within 24 hours after the first procedure. One case of a disconnected catheter drainage system was observed during a positional change of the patient, and another case of leakage of the mid-portion of the catheter drainage system was observed. No other sources of clinical failure were reported in the EMRs.
Seventeen complications were documented among the 96 procedures (Table 2). The lumbar drain was not tolerable in one patient after two serial procedures due to itching at the puncture site. Two patients developed nerve root irritation. Symptoms were controlled with analgesics in one of these cases and a transforaminal epidural steroid injection was needed to alleviate the symptoms in the other case.
Organisms were identified in CSF cultures in three of seven meningitis cases (Table 3). One patient diagnosed with meningitis had increased CSF WBC of 12 cells/mm3 but had no clinical symptoms of meningitis. Therefore, no additional CSF cultures were done. The drainage system was removed immediately in the remaining six patients who developed clinical meningitis, and intravenous antibiotic therapy was maintained until the infection was controlled. External lumbar drains were re-inserted in two cases after the infection was controlled.
The lumbar drainage catheter was retained in the epidural space of one patient without technical failure during the procedure. In this case, the catheter was accidentally sheared off during catheter management in the ward on day 4 after the procedure. A lumbar spine CT scan revealed the location of the catheter at the L2-4 level (Fig. 4). The catheter was removed in an operation, and the patient was discharged 14 days later with no neurological deficit.
Since the first reported external lumbar drainage system was used by Voursh in 1963, the success rate of treating CSF fistulas with an external lumbar drainage system has varied at 85-94% (3891011). The high success rate of treating or preventing CSF leaks, together with the simplicity of the procedure and low complication rates, has made the procedure widely accepted.
Fluoroscopic-guided lumbar drainage has been used for several decades to overcome the challenge of blind attempts to access the thecal sac. Eskey and Ogilvy (5) reported that fluoroscopic-guided lumbar puncture lowers the frequency of a traumatic spinal tap in patients with a CT-negative subarachnoid hemorrhage. Another study showed that fluoroscopic-guided lumbar puncture procedures are successful in patients with a history of a failed tap (6).
Given the lack of a concurrent comparator arm, it was not possible to compare the success and complication rates with those of bedside lumbar drainage cases. As the standard care protocol of our hospital states that lumbar drainage should be attempted initially at bedside, it was a reasonable assumption to regard the patient group referred to the radiological department as the technically difficult patient group. Although not all of the causes of failed bedside attempts were recorded, patients with a history of lumbar surgery, difficulty cooperating, or obesity were referred to the radiological department. Our single-arm study resulted in a technical success rate of 99.0% and a clinical success rate of 89.6% after 96 procedures, suggesting that the fluoroscopic-guided procedure is reliable in a difficult patient group.
The complication rate was 17.7%, including both minor and major complications. The definition of a minor complication differs among previous studies (3111213). In our study, we included oozing or itching symptoms that required re-insertion of the catheter as minor complications, which were not included in previous studies. However, unlike other studies (310111314), headache was not included as a complication in our study. Although it is a common and significant complication, it is unclear whether headache is associated with the procedure itself or with the CSF drainage, and it was unrealistic to distinguish between these two possible causes based on the medical records and the retrospective nature of our study.
The complication rate of clinical meningitis was 7.3% (95% CI, 3.6-14.3%) and that of bacterial meningitis was 3.1% (95% CI, 1.1-8.8%) in our study with use of prophylactic antibiotics. These results are comparable with the bacterial meningitis complication rate in a study by Shapiro and Scully (10) who reported a 3.0% complication rate with prophylactic antibiotic use. Others have reported 4.2% and 10.0% complication rate without the use of prophylactic antibiotics (311).
Attempts to overcome the blind procedure using CT have been introduced (4). The effective radiation dose of CT-guided and fluoroscopic-guided lumbar puncture are not different. Although CT guidance has an advantage of direct visualization of the thecal sac, no studies have compared the radiation doses between the two procedures for lumbar drainage.
This study had several limitations. The main limitation is due to the retrospective nature of the study. First, some EMRs did not state why the patient required fluoroscopic-guided external lumbar drainage, which may have affected our assumption that our patient group was technically difficult. Second, minor complications were not fully analyzed. Various symptoms, such as itching, oozing, or headache, may have been underestimated based on the EMRs. Therefore, we excluded headache as a complication, and itching and oozing requiring catheter removal or re-insertion were considered minor complications. Third, the patient group was heterogeneous. Therefore, direct comparisons between the complications that occurred in our patients with those reported in other studies or in a subgroup analysis are limited.
In conclusion, fluoroscopic-guided external lumbar drainage is a technically reliable procedure in patients who have failed bedside attempts, a history of lumbar surgery, difficulties in cooperation, or obesity.
Figures and Tables
Fig. 1
Epidural location of needle, which was not intrathecal position.
Fluoroscopic-guided lumbar drainage showing flowing or lentiform-shaped appearance of contrast (arrow), indicating that needle position in posterior epidural space was inappropriate.

Fig. 2
Subdural location of needle, which was not intrathecal position.
Thick linear filling of contrast on lateral view (A, arrow) and antero-posterior view (B, arrows), without contrast filling along nerve roots in central canal or near neural foramen, indicative of needle positioned in subdural space.

Fig. 3
Malpositioning of catheter tip.
Contrast filling was only seen near puncture site at lumbar spine level (dashed arrow) and not at thoracolumbar junction via obtuse-angled catheter (arrow) on follow-up myelogram of 65-year-old male patient with inefficient cerebrospinal fluid drainage day after fluoroscopic-guided lumbar drainage. Malpositioning of catheter tip with loop was suspected in this patient, and patient was discharged without complications after re-inserting catheter.

Fig. 4
Broken catheter with loop.
47-year-old male complained of inefficient cerebrospinal fluid drainage on day 4 after fluoroscopic-guided lumbar drainage procedure due to accidental disconnection. Computed tomography scan taken 11 days after procedure revealed that long loop had formed in catheter in posterior epidural space at L2/4 level (arrows), which was removed by operation (A, reformmated coronal image; B, axial image).

Table 1
Indications for Lumbar Drainage in Selected Patients

Table 2
Complications after Fluoroscopic-Guided Lumbar Drainage
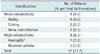
Table 3
Meningitis after Fluoroscopic Guided Lumbar Drainage

*One patient had pleocytosis, with white blood cell of 12 cells/mm3. Although classified as clinical meningitis in our study, clinically, it was regarded as subclinical meningitis. Therefore, cerebrospinal fluid culture study was not performed in this patient. CNS = Coagulase Negative Staphylococcus, EVD = extraventricular drainage, ICH = intracerebral hemorrhage, IVH = intraventricular hemorrhage, K. pneumoniae = Klebsiella pneumoniae, MMD = Moyamoya disease, SAH = subarchnoid hemorrhage, TSA = transphenoidal approach
References
1. Findler G, Sahar A, Beller AJ. Continuous lumbar drainage of cerebrospinal fluid in neurosurgical patients. Surg Neurol. 1977; 8:455–457.
2. Post KD, Stein BM. Technique for spinal drainage. Neurosurgery. 1979; 4:255.
3. Roland PS, Marple BF, Meyerhoff WL, Mickey B. Complications of lumbar spinal fluid drainage. Otolaryngol Head Neck Surg. 1992; 107:564–569.
4. Gold MM, Miller TS, Farinhas JM, Altschul DJ, Bello JA, Brook AL. Computed tomography-guided lumbar drain placement. J Neurosurg Spine. 2008; 9:372–373.
5. Eskey CJ, Ogilvy CS. Fluoroscopy-guided lumbar puncture: decreased frequency of traumatic tap and implications for the assessment of CT-negative acute subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2001; 22:571–576.
6. Brook AD, Burns J, Dauer E, Schoendfeld AH, Miller TS. Comparison of CT and fluoroscopic guidance for lumbar puncture in an obese population with prior failed unguided attempt. J Neurointerv Surg. 2014; 6:324–328.
7. Sato K, Shimizu S, Oka H, Fujii K. Intraoperative fluoroscopy with contrast medium for correct lumbar catheter placement in lumboperitoneal shunts. Kitasato Med J. 2013; 43:155–158.
8. Graf CJ, Gross CE, Beck DW. Complications of spinal drainage in the management of cerebrospinal fluid fistula. J Neurosurg. 1981; 54:392–395.
9. Kitchel SH, Eismont FJ, Green BA. Closed subarachnoid drainage for management of cerebrospinal fluid leakage after an operation on the spine. J Bone Joint Surg Am. 1989; 71:984–987.
10. Shapiro SA, Scully T. Closed continuous drainage of cerebrospinal fluid via a lumbar subarachnoid catheter for treatment or prevention of cranial/spinal cerebrospinal fluid fistula. Neurosurgery. 1992; 30:241–245.
11. Açikbaş SC, Akyüz M, Kazan S, Tuncer R. Complications of closed continuous lumbar drainage of cerebrospinal fluid. Acta Neurochir (Wien). 2002; 144:475–480.
12. Coplin WM, Avellino AM, Kim DK, Winn HR, Grady MS. Bacterial meningitis associated with lumbar drains: a retrospective cohort study. J Neurol Neurosurg Psychiatry. 1999; 67:468–473.
13. Governale LS, Fein N, Logsdon J, Black PM. Techniques and complications of external lumbar drainage for normal pressure hydrocephalus. Neurosurgery. 2008; 63:4 Suppl 2. 379–384. discussion 384
14. Farhat HI, Elhammady MS, Levi AD, Aziz-Sultan MA. Cervical subarachnoid catheter placement for continuous cerebrospinal fluid drainage: a safe and efficacious alternative to the classic lumbar cistern drain. Neurosurgery. 2011; 68:1 Suppl Operative. 52–56. discussion 56




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download