Abstract
Contrast-enhanced computed tomography colonography (CE-CTC) is a useful guide for the laparoscopic surgeon to avoid incorrectly removing the colonic segment and the failure to diagnose of synchronous colonic and extra-colonic lesions. Lymph node dissection and vessel ligation under a laparoscopic approach can be time-consuming and can damage vessels and organs. Moreover, mesenteric vessels have extreme variations in terms of their courses and numbers. We describe the benefit of using an abdominal vascular map created by CE-CTC in laparoscopic colorectal surgery candidates. We describe patients with different diseases (colorectal cancer, diverticular disease, and inflammatory bowel disease) who underwent CE-CTC just prior to laparoscopic surgery.
Contrast-enhanced computed tomography colonography (CE-CTC) is the best technique for colorectal cancer sites and staging (12), as well as to diagnose synchronous colonic lesions (3) in patients with obstructing cancers. CE-CTC is also useful to preoperatively evaluate others colorectal diseases, such as diverticular disease and inflammatory bowel disease (45). The laparoscopic approach for colonic surgery has become common and widely used because of the multiple advantages compared to conventional laparotomy. Laparoscopic surgery produces smaller surgical incisions, less intraoperative blood loss, faster recovery of normal bowel function, and shorter hospitalization (67). Nevertheless, the disadvantages to this approach include lack of a panoramic view of the operative field and tactile sensation, leading to potential inaccurate localization of a colonic lesion and difficulties with vessel ligation and lymph node dissection (8). Only a few studies have analysed the vascular anatomy of the colon using multidetector CT (91011) and only one used CT colonography (12).
Bowel preparation consisted of a low-fiber diet and a mild laxative (macrogol solution) the day before CT. Faeces were tagged by administering 60-90 mL amidotrizoate meglumine and 500 mL water at least 3 hours before the examination. The colon was distended by insufflating at least 3 L of carbon dioxide using an automatic insufflator. A vial of hyoscine N-butylbromide was intravenously injected just prior to insufflation. We performed a pre-contrast scan with the patient in the prone position using low mAs and different post-contrast scans in the supine position after injecting 500-600 mgI/kg/body weight. Post-contrast scans may have included arterial (obtained using bolus-tracking monitoring technique), portal venous, and delayed phases depending on the disease.
Comprehending the complex three-dimensional (3D) anatomy of the colon and branching vessels is difficult on axial images, particularly for inexperienced readers. 3D imaging provides surgeons with a precise and immediate understanding of the patient's anatomy, including colonic loop shapes, colonic lesion sites, and the courses and relationships of the branching vessels. We obtained 3D fused images using a dedicated workstation (Advantage Workstation 4, General Electric Healthcare, Waukesha, WI, USA) by processing the CT dataset from the arterial and portal-venous phases. Three reformations with different settings (3D colon map and two different 3D vascular presets) were prepared separately and fused together into a single volume, which included the 3D colon map, a 3D arteriogram, and a 3D venogram, with the mesenteric arteries colored in red and relevant venous branches colored in blue. This resulted in a colon map that overlapped with the vascular map and showed the mesenteric branching pattern and the relationships between the colonic lesions, arteries and veins. The 3D images could be tilted and rotated to obtain the view that best simulates the intraoperative field of view.
CT colonography allows for an accurate pre-operative assessment of colonic anatomy, and the locations of the colonic lesions and lymph nodes. Post-contrast acquisition and the vascular map allow for a precise evaluation of mesenteric artery branching patterns and the relationships between arterial and venous vessels. Although the laparoscopic approach has many obvious benefits compared to laparotomy, it suffers from a restricted operative field of view and an inability to manipulate tissues, which can result in time-consuming dissections when searching for anatomical landmarks, lymph nodes, or vessels. Intraoperative conversion rates to laparotomy from laparoscopic colectomy are 10-20% (713) and is often due to difficulties identifying mesenteric vessels, synchronous tumors, intraoperative bleeding or procedure length (7). Complications, such as bleeding and bowel ischemia, can occur because of vascular injury while dissecting nodes or ligating a vessel. Previous knowledge of the patient's mesenteric vascular anatomy, including arterial branching variants and relationships with adjacent veins, reduces operative time and the incidence of intraoperative complications (11).
The branching pattern of the superior mesenteric artery (SMA) must be assessed before a right hemicolectomy and right transverse colon surgery. The middle colic artery (MCA) and the ileocolic artery (ICA) are present in almost all patients, whereas the right colic artery (RCA) is present in about 50% of cases (Figs. 1, 2). The inconsistency in the presence of the accessory left colic artery (ALCA), known as the artery of Riolan, originates from the SMA or MCA and anastomoses with the left colic artery (LCA), feeding the transverse colon (Figs. 3, 4). The common origin of the MCA, RCA, and ICA (Fig. 5) has been described (89). The most significant variant to be considered during laparoscopic right hemicolectomy is the relationship between the colic arteries and the superior mesenteric vein (SMV); arteries cross anterior to the SMV in most patients, but a posterior crossing pattern of the ICA, MCA, or RCA is also common (Figs. 5, 6). The ICA runs posteriorly to the SMV in 67% of cases (8). It is important to locate the ALCA and the branching pattern of the inferior mesenteric artery (IMA) when planning left transverse colon surgery and left hemicolectomy. The LCA is absent in 12% of individuals (Fig. 7) (14). The same considerations can be applied to sigmoid colon and rectal surgery. Moreover, pre-operative planning for sigmoidectomy should include an evaluation of the sigmoid artery (SA) branching pattern because the IMA can be preserved if the SAs are selectively ligated. The number of SAs varies and they can either originate from the IMA or LCA (Figs. 2, 4, 7) (15). The relationship between arteries and the inferior mesenteric vein (IMV) can also vary: LCA and SAs can either cross anteriorly or posteriorly to the IMV (Figs. 8, 9). Because of their close proximity, the relationships between the LCA, SAs, and the left gonadic vein and ureter must be assessed. The origins of other splanchnic arteries from the SMA or IMA must also be considered be. For example, right hepatic artery frequently branches from the SMA (Fig. 7) (15). Variants in mesenteric vein drainage should also be evaluated (Fig. 8).
Figures and Tables
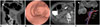 | Fig. 175-year-old man with distal ascending colon cancer (pT3N1a).
A. Coronal computed tomography colonography (CTC) image demonstrates stenosing cancer (arrowhead) in distal ascending colon. B. Three-dimensional (3D) endoluminal view confirms stenosis. C. Axial CTC image shows enlarged locoregional lymph node (arrow). D. 3D-fused image shows apple-core wall deformation (arrowhead), presence of right colic artery (RCA), and superior mesenteric vein (SMV) running posterior to arteries. ICA = ileocolic artery, MCA = middle colic artery, SMA = superior mesenteric artery
|
 | Fig. 277-year-old woman with pT3N0 rectal cancer.Axial CTC (A) image shows large stenosing tumor (arrowheads) in proximal rectum. Three-dimensional (3D)-fused images (B, C) demonstrate common origin of left colic artery (LCA) and sigmoid artery (SA), both running anterior to inferior mesenteric vein (IMV); right colic artery (RCA) is also detectable. Lateral view of 3D-fused image (C) shows cancer (arrowheads), its extension, and relationship with feeding vessels. CTC = computed tomography colonography, ICA = ileocolic artery, IMA = inferior mesenteric artery, MCA = middle colic artery, SMA = superior mesenteric artery, SRA = superior rectal artery
|
 | Fig. 376-year-old man with colonic cancer.
A. Axial computed tomography colonography (CTC) image shows stenosing tumor involving left transverse colon (arrowhead). B. CTC also allows for diagnosis of pedunculated 2-cm synchronous polypoid lesion in sigmoid colon, together with diverticular disease findings. C. Three-dimensional-fused image demonstrates accessory left colic artery (ALCA) branching from middle colic artery (MCA) with separate origin from left colic artery (LCA) and sigmoid arteries (SAs). ICA = ileocolic artery, IMA = inferior mesenteric artery, SMA = superior mesenteric artery, SRA = superior rectal artery
|
 | Fig. 453-year-old woman with sigmoid chronic diverticulitis was referred for surgery because of symptomatic disease.
A, B. Pre-operative computed tomography colonography to assess presence of diverticula (arrowhead in A) and sigmoid colon wall thickening (arrowhead in B) related to disease. C, D. Three-dimensional-fused images demonstrate sigmoid arteries (SAs) branching from left colic artery (LCA) and accessory left colic artery (ALCA) branching from middle colic artery (MCA); LCA and SAs run anteriorly to inferior mesenteric vein (IMV). ICA = ileocolic artery, IMA = inferior mesenteric artery, SMA = superior mesenteric artery, SRA = superior rectal artery
|
 | Fig. 566-year-old woman with relapsing Crohn's disease.Axial, para-sagittal, and maximum intensity projection reformatted computed tomography colonography (A-C) depict perivisceral "comb sign", enlarged lymph nodes and diffuse colonic wall thickening causing two stenoses (arrowheads in A, C) in transverse colon. Three-dimensional-fused image (D) shows common origin of middle colic artery (MCA) and ileocolic artery (ICA) running posteriorly to superior mesenteric vein (SMV); right colic artery is absent; left colic artery (LCA) runs posteriorly to inferior mesenteric vein (IMV), which drains into SMV. IMA = inferior mesenteric artery, SA = sigmoid artery, SMA = superior mesenteric artery, SRA = superior rectal artery
|
 | Fig. 632-year-old man with severe Crohn's disease.Axial and coronal computed tomography colonography images (A, B) show involvement of distal ileum and right and transverse colon, causing colonic wall thickening with characteristic "cobblestone" appearance of mucosa (arrowhead), together with perivisceral "comb sign" and enlarged lymph nodes. Three-dimensional-fused images (C, D) demonstrate ileocolic artery (ICA) running posteriorly to superior mesenteric vein (SMV), absence of right colic artery, and inferior mesenteric vein (IMV) draining into SMV, together with characteristic wall thickening (arrowhead). IMA = inferior mesenteric artery, LCA = left colic artery, MCA = middle colic artery, SA = sigmoid artery, SMA = superior mesenteric artery, SMV = superior mesenteric vein, SRA = superior rectal artery
|
 | Fig. 774-year-old man with sigmoid colon cancer (pT3N1b).Axial and coronal computed tomography colonography images (A, B) show severe sigmoid colon stenosing lesion (arrowhead), preventing adequate bowel preparation. Three-dimensional reconstructions (C, D) demonstrate sigmoid colon lesion (arrowhead in D), sigmoid arteries (SAs) branching directly from inferior mesenteric artery (IMA), running anteriorly to inferior mesenteric vein (IMV); left colic artery is absent; multiple enlarged lymph nodes along tumor feeding vessels are present; moreover, right hepatic artery (RHA) branches from superior mesenteric vein. SMA = superior mesenteric artery, SRA = superior rectal artery
|
 | Fig. 872-year-old man with sigmoid colon cancer.Axial computed tomography colonography images (A, B) demonstrate sigmoid colon stenosing cancer (arrowhead in A), and enlarged lymph nodes. Three-dimensional-fused images (C, D) show "apple-core" sigmoid colon wall deformity (arrowhead in D), descending branch of left colic artery (LCA), and sigmoid artery (SA) running posteriorly to inferior mesenteric vein (IMV); IMV drains into splenic vein (SV). IMA = inferior mesenteric artery, SRA = superior rectal artery
|
 | Fig. 974-year-old male with 3-cm tubular-villous adenoma and high-grade dysplasia (pTis).Axial and three-dimensional (3D) endoluminal computed tomography colonography (A, B) show vegetating lesion (arrowhead in A) in transverse colon. 3D-fused image (C) shows that right colic artery is absent and both middle colic artery (MCA) and ileocolic artery (ICA) run anteriorly to superior mesenteric vein (SMV); left colic artery (LCA) runs posteriorly to inferior mesenteric vein (IMV); IMV drains into SMV. SA = sigmoid artery, SRA = superior rectal artery
|
References
1. Neri E, Turini F, Cerri F, Faggioni L, Vagli P, Naldini G, et al. Comparison of CT colonography vs. conventional colonoscopy in mapping the segmental location of colon cancer before surgery. Abdom Imaging. 2010; 35:589–595.
2. Flor N, Ceretti AP, Mezzanzanica M, Rigamonti P, Peri M, Tresoldi S, et al. Impact of contrast-enhanced computed tomography colonography on laparoscopic surgical planning of colorectal cancer. Abdom Imaging. 2013; 38:1024–1032.
3. Park SH, Lee JH, Lee SS, Kim JC, Yu CS, Kim HC, et al. CT colonography for detection and characterisation of synchronous proximal colonic lesions in patients with stenosing colorectal cancer. Gut. 2012; 61:1716–1722.
4. Flor N, Rigamonti P, Pisani Ceretti A, Romagnoli S, Balestra F, Sardanelli F, et al. Diverticular disease severity score based on CT colonography. Eur Radiol. 2013; 23:2723–2729.
5. Regge D, Neri E, Turini F, Chiara G. Role of CT colonography in inflammatory bowel disease. Eur J Radiol. 2009; 69:404–408.
6. Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007; 246:655–662. discussion 662-664
7. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005; 6:477–484.
8. Ignjatovic D, Sund S, Stimec B, Bergamaschi R. Vascular relationships in right colectomy for cancer: clinical implications. Tech Coloproctol. 2007; 11:247–250.
9. Spasojevic M, Stimec BV, Fasel JF, Terraz S, Ignjatovic D. 3D relations between right colon arteries and the superior mesenteric vein: a preliminary study with multidetector computed tomography. Surg Endosc. 2011; 25:1883–1886.
10. Hirai K, Yoshinari D, Ogawa H, Nakazawa S, Takase Y, Tanaka K, et al. Three-dimensional computed tomography for analyzing the vascular anatomy in laparoscopic surgery for right-sided colon cancer. Surg Laparosc Endosc Percutan Tech. 2013; 23:536–539.
11. Mari FS, Nigri G, Pancaldi A, De Cecco CN, Gasparrini M, Dall'Oglio A, et al. Role of CT angiography with three-dimensional reconstruction of mesenteric vessels in laparoscopic colorectal resections: a randomized controlled trial. Surg Endosc. 2013; 27:2058–2067.
12. Matsuki M, Okuda J, Kanazawa S, Kanamoto T, Inada Y, Tatsugami F, et al. Virtual CT colectomy by three-dimensional imaging using multidetector-row CT for laparoscopic colorectal surgery. Abdom Imaging. 2005; 30:698–708.
13. Belizon A, Sardinha CT, Sher ME. Converted laparoscopic colectomy: what are the consequences? Surg Endosc. 2006; 20:947–951.
14. Kobayashi M, Morishita S, Okabayashi T, Miyatake K, Okamoto K, Namikawa T, et al. Preoperative assessment of vascular anatomy of inferior mesenteric artery by volume-rendered 3D-CT for laparoscopic lymph node dissection with left colic artery preservation in lower sigmoid and rectal cancer. World J Gastroenterol. 2006; 12:553–555.
15. Horton KM, Fishman EK. Volume-rendered 3D CT of the mesenteric vasculature: normal anatomy, anatomic variants, and pathologic conditions. Radiographics. 2002; 22:161–172.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download