Abstract
Objective
To estimate and compare radiation exposure during transforaminal fluoroscopy-guided epidural steroid injection (TFESI) at different vertebral levels.
Materials and Methods
Fluoroscopy-guided TFESI was performed in 181 patients. The patients were categorized into three groups according to the injected lumbosacral nerve level of L2-4, L5, or S1. Fluoroscopy time (FT) and dose area product (DAP) were recorded for all patients; correlations between FT and DAP were determined at each level, and both FT and DAP were compared between the different vertebral levels.
Results
The numbers of patients who received ESI at L2-4, L5, and S1 were 29, 123, and 29. Mean FT was 44 seconds at L2-4, 33.5 seconds at L5, and 37.7 seconds at S1. Mean DAP was 138.6 µGy·m2 at L2-4, 100.6 µGy·m2 at L5, and 72.1 µGy·m2 at S1. FT and DAP were positively correlated in each group (p values < 0.001). FT was significantly shorter at L5 than that at L2-4 (p = 0.004) but was not significantly different between S1 and L2-4 or L5 (p values = 0.286 and 0.532, respectively). DAP was significantly smaller at L5 and S1 than that at L2-4, but L5 and S1 were not significantly different. After correcting for FT, DAP was significantly smaller at S1 than that at either L2-4 or L5 (p values = 0.001 and 0.010).
Epidural steroid injections (ESI) are widely used for managing low back pain and radiating symptoms. ESIs are used to relieve pain associated with conditions, such as degenerative disc disease, annular tear, lumbar spinal stenosis, spondylosis, spondylolisthesis, or post-laminectomy syndrome (1), and can be effective for treatment prior to or adjuvant with surgery and decrease the need for surgical intervention (2, 3).
Techniques available to access the lumbosacral epidural space include transforaminal, caudal, and interlaminar approaches, although the transforaminal route is considered more specific for the lumbosacral spine because it provides direct delivery of the injectate.
The needle for transforaminal ESI can be placed without imaging guidance; however, incorrect placement may occur in up to 30% of patients when conducted blindly, and intravenous injection has been reported in some cases (1). Accordingly, fluoroscopy is commonly and increasingly used as a guidance modality during ESI to ensure accurate needle placement (4). Computed tomography fluoroscopy-guided ESI can be used but conventional fluoroscopy is favored because of concerns about higher radiation exposure (5).
Similar to all other types of interventional radiology, fluoroscopy-guided ESI has associated risks stemming from patient and radiologist radiation exposure; thus, monitoring radiation dose is mandatory to minimize these risks. Estimates of radiation doses to patients during spinal pain intervention have been reported, although these studies compared ESI with other procedures, such as facet joint injection or sacroiliac joint injection (6, 7).
Almost no studies have compared radiation doses at different lumbosacral levels in patients receiving transforaminal ESI. Radiation doses are cumulative, as patients can receive repeated transforaminal ESI (7); therefore, knowledge and monitoring of the amount of radiation exposure is important. No universally accepted reference level is available for fluoroscopy-guided spinal pain management. This study was undertaken to determine and compare radiation exposure during transforaminal ESI at different vertebral levels.
We retrospectively reviewed patients who received a lumbosacral transforaminal ESI to treat back pain or sciatica over a 6-month period (July 2010-December 2011). Patients who underwent an operation without instrumentation, such as a simple discectomy or foraminotomy, were included, whereas those with a history of surgery using metallic implants were excluded because of the risk of increased radiation scatter. Patients who had received lumbosacral ESI at more than one level and/or more than one time were also excluded.
A total of 181 patients (68 males and 113 females; mean age, 61.3 years; range, 19-87 years) were included. The numbers of patients that received ESI at L2-4, L5, and S1 were 29 (15 males and 14 females; mean age, 70.3 years), 123 (45 males and 78 females; mean age, 59.8 years), and 29 (8 males and 21 females; mean age, 60.8 years), respectively.
We reviewed L-spine magnetic resonance images and plain radiographs prior to ESI and decided on the appropriate level by comparing symptoms with dermatome and imaging findings.
All ESIs were conducted under single-plane fluoroscopy guidance by one musculoskeletal radiologist with 16 years experience. We used a single-plane fluoroscopy machine (Artis Zee Multi-Purpose System, Siemens Healthcare, Erlangen, Germany) and controlled projection of the X-ray beam manually. Tube current and beam energy dose were automatically chosen based on body mass index. The procedure was conducted in the prone position, as follows: The skin was sterilized, and X-rays were applied obliquely to localize the anesthetic point. The skin and subcutaneous layers were anesthetized with 2% lidocaine (Rapidocain 20 mg/mL, Sintetica SA, Switzerland). The spinal needle was located at the anesthetic injection site. An oblique fluoroscopy view was used parallel to the needle direction. The spinal needle was advanced in this direction to the neural foramen under oblique X-ray imaging guidance, and the X-ray tube was rotated to the anteroposterior (AP) projection to check that the needle tip was in the epidural space. The precise needle location was confirmed by visualizing contrast medium spread in the epidural space along the nerve root (Figs. 1, 2). The procedure was completed by injecting 0.5 mL ropivacaine hydrochloride (2 mg/mL, Naropin 0.2%, AstraZeneca, Wilmington, DE, USA) and 1 mL triamcinolone acetate (40 mg/mL, TRIAM, Shin Poong Pharm., Seoul, Korea). Fluoroscopy was used to determine the location for anesthesia, to introduce the spinal needle, and to confirm that the contrast media (Iohexol 300 mg I/mL, Omnipaque 300, GE Healthcare, Milwaukee, WI, USA) was in the epidural space. Collimation and last image hold were used to minimize radiation dose. Fluoroscopy time and dose area product were recorded automatically by the fluoroscopy equipment.
The patients were divided into three groups according to the lumbosacral nerve level injected, such as the L2-4, L5, or S1 groups; L2, L3, and L4 were allocated to one group because of similar anatomy with respect to ESI performance.
The relationship between fluoroscopy time and dose area product was evaluated in all three groups. Pearson's correlation coefficients were used for the statistical analysis (Stata ver. 11; Stata Corp LP, College Station, TX, USA). Fluoroscopy times and dose area products, as well as the dose area product after correcting for fluoroscopy time in the three groups were compared using analysis of variance and analysis of covariance, respectively (SPSS ver. 16; SPSS Inc., Chicago, IL, USA). Statistical significance was accepted for p values < 0.05.
Fluoroscopy times were 14-113 seconds at L2-4 (mean, 44.0 seconds), 11-161 seconds at L5 (mean, 33.5 seconds), and 18-138 seconds at S1 (mean, 37.7 seconds). The dose area products were 37.4-529.6 µGy·m2 (mean, 138.6 µGy·m2) at L2-4, 3.02-1048.2 µGy·m2 (mean, 100.6 µGy·m2) at L5, and 26.3-209.7 µGy·m2 at S1 (mean, 72.1 µGy·m2).
Fluoroscopy time and dose area product were positively correlated in each group (Table 1). Fluoroscopy time was significantly shorter at L5 than that at L2-4 when the three were compared pairwise (p = 0.004). Fluoroscopy time was not significantly different between S1 and L2-4 or L5 (p values = 0.286 and 0.532, respectively). Dose area product was smaller at L5 and S1 than that at L2-4 (p values = 0.003 and 0.001). However, after correcting for fluoroscopy time, dose area product at S1 was significantly smaller than that at L2-4 or L5 (p values = 0.001 and 0.010) (Table 2).
Four metrics are used for estimating radiation dose during fluoroscopy-guided procedures, such as peak skin dose, reference point air kerma, dose area product, and fluoroscopy time. Dose area product, which is also known as the kerma area product, is a measure of total X-ray energy leaving the X-ray tube (8) and provides better estimates of the risk for radiation injury than those of fluoroscopy time, according to Fletcher et al. (9). Dose area product is convenient and widely used to measure total X-ray energy and to estimate stochastic injury. However, it is limited with respect to predicting skin effects because dose area product values are not affected by the source-to-patient distance but radiation dose decreases with increasing distance (2, 8, 10). Despite this limitation, Hirshfeld et al. (11) reported that dose area product can be used as a benchmark measure.
Fluoroscopy time is measured easily; thus, providing a way to easily monitor the amount of radiation used. However, fluoroscopy time is not correlated strongly with radiation risk (12), with other dose metrics, or the doses administered to patients (8). In our study, fluoroscopy times correlated well with radiation doses, although fluoroscopy times and dose area products differed at the three lumbosacral nerve levels, suggesting that more effort should be given to shortening fluoroscopy time.
The Society of Interventional Radiology-Cardiovascular and Interventional Radiological Society of Europe (SIR-CIRSE) guidelines on radiation management defined the significant radiation dose threshold using a dose area product of 500 Gy·cm2 and fluoroscopy time of 40-60 minutes (13). In the present study, the dose area product was 3.02-529.6 µGy·m2 during transforaminal ESI at the lumbosacrum, and fluoroscopy time was 11-161 seconds (mean values, 101.7 ± 108.0 µGy·m2 and 36.0 ± 22 seconds, respectively). Accordingly, dose area products were much lower and fluoroscopy times were much shorter in the present study than those of other interventional procedures and in the SIR-CIRSE guidelines. Nevertheless, care should be taken when monitoring the accumulated radiation dose, as patients commonly receive repeated ESI, distinct from other interventional procedures. Moreover, dose area products and fluoroscopy times were greater and longer than those reported by Hanu-Cernat for the radiation dose during lumbar or caudal epidural injections, and a mean fluoroscopy time of 16 ± 7 seconds and a mean dose area product of 0.79 ± 0.66 Gy·cm2 was reported (7). However, their study involved a smaller number of patients, included a caudal injection, and did not subdivide the cohort into lumbosacral levels.
Zhou et al. (6) measured fluoroscopy times required for ESI by seven physicians. The results ranged from 22 ± 8 to 92 ± 21 seconds among physicians. The major reason for these differences was the training system in place at these university pain clinics, which provide hands-on experience to residents and fellows that are not fully experienced with the technique. These results indicate that experience is a major contributor to fluoroscopy exposure time. In fact, Manchikanti et al. (14) concluded that considerable experience-based differences exist among physicians. However, in our study, experience-based effects were eliminated, as one fully experienced radiologist performed all procedures. Nevertheless, fluoroscopy times in our study were more widely variable than those in previous studies, probably due to the much larger study population of 181 patients. In addition, patient variables, such as age and resulting degenerative change underlying spinal pathology or anatomic variants, may have influenced fluoroscopy time. In our study, a few elder patients had much longer fluoroscopy times, which increased variation in the fluoroscopy time.
According to our results, an L5 injection produced the shortest fluoroscopy time during transforaminal ESI. This level exhibits more degenerative changes and is more often used during ESI than the upper lumbar spine and sacrum, which means that radiologist experience is greater at this level. In addition, L5 is slightly more superficially located than the upper lumbar spine and offers an easier approach.
After correcting for fluoroscopy time, the S1 dose area product was significantly smaller than that at the lumbar level, indicating that radiation exposure per seconds was smaller at S1. This smaller radiation dose may be explained by the relatively superficial location and smaller body parts involved.
The neural foramen of the sacrum differs in shape from those of the lumbar spine, and precise targeting of the neural foramen can be difficult, particularly when the ventral and dorsal foramen area is over-projected on the fluoroscopic images. This difficulty can be solved by using slight caudal tilt or oblique projection fluoroscopy, as reported by Fish et al. (15). In our study, the AP view or a slightly oblique view to the ipsilateral side of the targeted foramen with < 10° rotation of the tube and without cranial or caudal tilt was used when the approach to the S1 foramen was difficult. We believe this method is effective for visualizing the S1 foramen, even in complicated cases.
In the present study, injections into the L2-4 level resulted in longer fluoroscopy times and greater dose area product values than those at the L5 and S1 levels, which may have been due to different degrees of degenerative change at L2-4 and L5, as well as the deeper location of L2-4 than that at L5 and S1. Moreover, these two levels are the most commonly affected levels for which many repeated lumbosacral transforaminal injections occur. Because of expected patho-anatomical obstacles in the needle pathway at these levels, we highlight the importance of the technical expertise of the radiologist.
We used continuous fluoroscopy mode rather than pulsed mode. Although pulsed fluoroscopy may have lower temporal resolution, it decreases the radiation dose significantly during fluoroscopy-guided spinal interventional pain procedures (2, 10). However, we only used fluoroscopy for a short time with intermittent exposure to confirm needle location and spread of contrast media in the epidural space. In addition, the procedure was conducted using the last image hold technique, which shows the last image continuously after completing exposure, and this may have reduced the radiation dose. This technique decreases fluoroscopy time by up to 50% as well (10). We also used collimation during fluoroscopy, which may have reduced tissue exposure volumes and radiation scatter and improved image contrast (2, 16).
Some limitations of this study should be considered. First, the number of patients in each level differed, although the size of the study population was considerably larger than that in previous studies. Second, generalizing our results is limited, as all procedures were conducted by one radiologist at a single center, although this eliminated inter-operator variability. Finally, patient variables, such as body habitus, were not considered, although the effects of body habitus on radiation exposure remain controversial. In fact, Miller et al. (12) concluded that correcting for patient weight has no significant effect on radiation dose.
In conclusion, radiation exposure during a single ESI procedure was assessed in a fairly large cohort. The radiation dose was small and differed between the different lumbosacral spine levels.
Figures and Tables
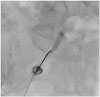
 | Fig. 148-year-old male with right sciatica.Transforaminal epidural steroid injection was conducted at right L5 neural foramen under anteroposterior X-ray imaging guidance. Precise needle location was confirmed by visualizing spread of contrast medium in epidural space.
|
 | Fig. 276-year-old female with low back pain and left sciatica.Transforaminal epidural steroid injection was conducted at left S1 level. X-ray tube was projected to anteroposterior direction to check needle tip location in epidural space. Needle location was confirmed by spread of contrast medium.
|
Table 1
FTs, DAPs during ESI and Their Correlation

Table 2
Comparisons of Group FTs, DAPs and DAP after FT Correction

References
1. Stout A. Epidural steroid injections for low back pain. Phys Med Rehabil Clin N Am. 2010; 21:825–834.
2. Fink GE. Radiation safety in fluoroscopy for neuraxial injections. AANA J. 2009; 77:265–269.
3. Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000; 82-A:1589–1593.
4. Friedly J, Chan L, Deyo R. Geographic variation in epidural steroid injection use in medicare patients. J Bone Joint Surg Am. 2008; 90:1730–1737.
5. Hoang JK, Yoshizumi TT, Toncheva G, Gray L, Gafton AR, Huh BK, et al. Radiation dose exposure for lumbar spine epidural steroid injections: a comparison of conventional fluoroscopy data and CT fluoroscopy techniques. AJR Am J Roentgenol. 2011; 197:778–782.
6. Zhou Y, Singh N, Abdi S, Wu J, Crawford J, Furgang FA. Fluoroscopy radiation safety for spine interventional pain procedures in university teaching hospitals. Pain Physician. 2005; 8:49–53.
7. Hanu-Cernat DE, Duarte R, Raphael JH, Mutagi H, Kapur S, Senthil L. Type of interventional pain procedure, body weight, and presence of spinal pathology are determinants of the level of radiation exposure for fluoroscopically guided pain procedures. Pain Pract. 2012; 12:434–439.
8. Miller DL, Balter S, Schueler BA, Wagner LK, Strauss KJ, Vañó E. Clinical radiation management for fluoroscopically guided interventional procedures. Radiology. 2010; 257:321–332.
9. Fletcher DW, Miller DL, Balter S, Taylor MA. Comparison of four techniques to estimate radiation dose to skin during angiographic and interventional radiology procedures. J Vasc Interv Radiol. 2002; 13:391–397.
10. Axelsson B. Optimisation in fluoroscopy. Biomed Imaging Interv J. 2007; 3:e47.
11. Hirshfeld JW Jr, Balter S, Brinker JA, Kern MJ, Klein LW, Lindsay BD, et al. ACCF/AHA/HRS/SCAI clinical competence statement on physician knowledge to optimize patient safety and image quality in fluoroscopically guided invasive cardiovascular procedures: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training. Circulation. 2005; 111:511–532.
12. Miller DL, Kwon D, Bonavia GH. Reference levels for patient radiation doses in interventional radiology: proposed initial values for U.S. practice. Radiology. 2009; 253:753–764.
13. Stecker MS, Balter S, Towbin RB, Miller DL, Vañó E, Bartal G, et al. Guidelines for patient radiation dose management. J Vasc Interv Radiol. 2009; 20:7 Suppl. S263–S273.
14. Manchikanti L, Cash KA, Moss TL, Rivera J, Pampati V. Risk of whole body radiation exposure and protective measures in fluoroscopically guided interventional techniques: a prospective evaluation. BMC Anesthesiol. 2003; 3:2.
15. Fish DE, Lee PC, Marcus DB. The S1 "Scotty dog": report of a technique for S1 transforaminal epidural steroid injection. Arch Phys Med Rehabil. 2007; 88:1730–1733.
16. Schueler BA. The AAPM/RSNA physics tutorial for residents: general overview of fluoroscopic imaging. Radiographics. 2000; 20:1115–1126.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download