1. Lederlin M, Thambo JB, Latrabe V, Corneloup O, Cochet H, Montaudon M, et al. Coronary imaging techniques with emphasis on CT and MRI. Pediatr Radiol. 2011; 41:1516–1525. PMID:
22127683.

2. Goo HW. State-of-the-art CT imaging techniques for congenital heart disease. Korean J Radiol. 2010; 11:4–18. PMID:
20046490.

3. Tang L, Merkle N, Schär M, Korosoglou G, Solaiyappan M, Hombach V, et al. Volume-targeted and whole-heart coronary magnetic resonance angiography using an intravascular contrast agent. J Magn Reson Imaging. 2009; 30:1191–1196. PMID:
19856454.

4. Vranicar M, Hirsch R, Canter CE, Balzer DT. Selective coronary angiography in pediatric patients. Pediatr Cardiol. 2000; 21:285–288. PMID:
10818198.

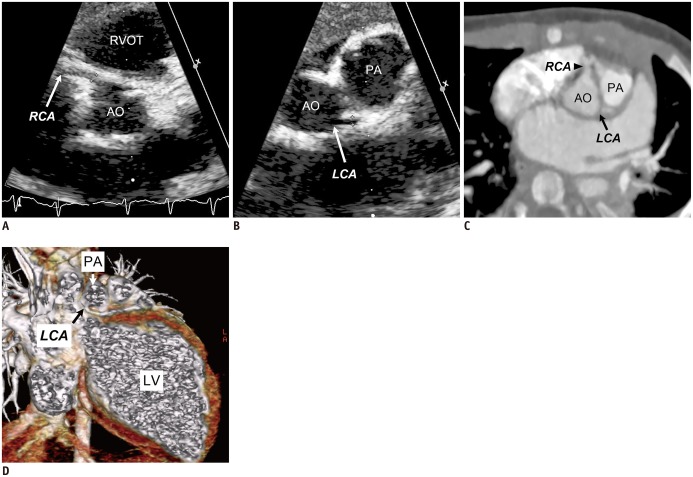
5. Attili A, Hensley AK, Jones FD, Grabham J, DiSessa TG. Echocardiography and coronary CT angiography imaging of variations in coronary anatomy and coronary abnormalities in athletic children: detection of coronary abnormalities that create a risk for sudden death. Echocardiography. 2013; 30:225–233. PMID:
23167634.

6. Goo HW. Cardiac MDCT in children: CT technology overview and interpretation. Radiol Clin North Am. 2011; 49:997–1010. PMID:
21889018.

7. Goo HW. Current trends in cardiac CT in children. Acta Radiol. 2013; 54:1055–1062. PMID:
23104372.

8. Weininger M, Barraza JM, Kemper CA, Kalafut JF, Costello P, Schoepf UJ. Cardiothoracic CT angiography: current contrast medium delivery strategies. AJR Am J Roentgenol. 2011; 196:W260–W272. PMID:
21343473.

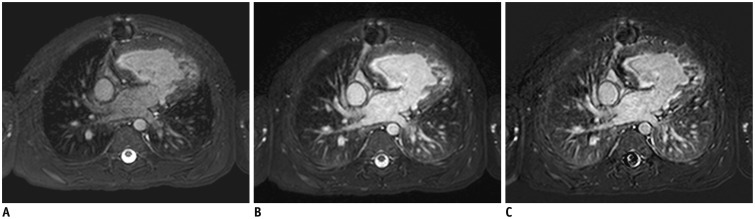
9. Kim JW, Goo HW. Coronary artery abnormalities in Kawasaki disease: comparison between CT and MR coronary angiography. Acta Radiol. 2013; 54:156–163. PMID:
23482350.

10. Mendoza DD, Joshi SB, Weissman G, Taylor AJ, Weigold WG. Viability imaging by cardiac computed tomography. J Cardiovasc Comput Tomogr. 2010; 4:83–91. PMID:
20430338.

11. Goo HW, Suh DS. Tube current reduction in pediatric non-ECG-gated heart CT by combined tube current modulation. Pediatr Radiol. 2006; 36:344–351. PMID:
16501970.

12. Goo HW, Suh DS. The influences of tube voltage and scan direction on combined tube current modulation: a phantom study. Pediatr Radiol. 2006; 36:833–840. PMID:
16642311.

13. Yang DH, Goo HW. Pediatric 16-slice CT protocols: radiation dose and image quality. J Korean Radiol Soc. 2008; 59:333–347.

14. Goo HW. Individualized volume CT dose index determined by cross-sectional area and mean density of the body to achieve uniform image noise of contrast-enhanced pediatric chest CT obtained at variable kV levels and with combined tube current modulation. Pediatr Radiol. 2011; 41:839–847. PMID:
21656275.

15. Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012; 13:1–11. PMID:
22247630.

16. Tsai IC, Goo HW. Cardiac CT and MRI for congenital heart disease in Asian countries: recent trends in publication based on a scientific database. Int J Cardiovasc Imaging. 2013; 29(Suppl 1):1–5. PMID:
23344910.

17. Makowski MR, Wiethoff AJ, Uribe S, Parish V, Botnar RM, Bell A, et al. Congenital heart disease: cardiovascular MR imaging by using an intravascular blood pool contrast agent. Radiology. 2011; 260:680–688. PMID:
21613441.

18. Greil GF, Seeger A, Miller S, Claussen CD, Hofbeck M, Botnar RM, et al. Coronary magnetic resonance angiography and vessel wall imaging in children with Kawasaki disease. Pediatr Radiol. 2007; 37:666–673. PMID:
17541574.

19. Hussain T, Fenton M, Peel SA, Wiethoff AJ, Taylor A, Muthurangu V, et al. Detection and grading of coronary allograft vasculopathy in children with contrast-enhanced magnetic resonance imaging of the coronary vessel wall. Circ Cardiovasc Imaging. 2013; 6:91–98. PMID:
23223637.

20. Taylor AM, Dymarkowski S, Hamaekers P, Razavi R, Gewillig M, Mertens L, et al. MR coronary angiography and late-enhancement myocardial MR in children who underwent arterial switch surgery for transposition of great arteries. Radiology. 2005; 234:542–547. PMID:
15591430.

21. Tacke CE, Kuipers IM, Groenink M, Spijkerboer AM, Kuijpers TW. Cardiac magnetic resonance imaging for noninvasive assessment of cardiovascular disease during the follow-up of patients with Kawasaki disease. Circ Cardiovasc Imaging. 2011; 4:712–720. PMID:
21921132.

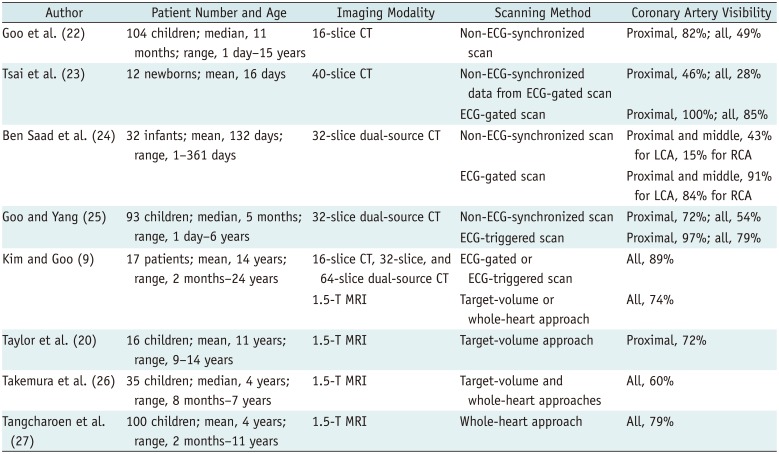
22. Goo HW, Park IS, Ko JK, Kim YH, Seo DM, Yun TJ, et al. Visibility of the origin and proximal course of coronary arteries on non-ECG-gated heart CT in patients with congenital heart disease. Pediatr Radiol. 2005; 35:792–798. PMID:
15886981.

23. Tsai IC, Lee T, Chen MC, Fu YC, Jan SL, Wang CC, et al. Visualization of neonatal coronary arteries on multidetector row CT: ECG-gated versus non-ECG-gated technique. Pediatr Radiol. 2007; 37:818–825. PMID:
17562037.

24. Ben Saad M, Rohnean A, Sigal-Cinqualbre A, Adler G, Paul JF. Evaluation of image quality and radiation dose of thoracic and coronary dual-source CT in 110 infants with congenital heart disease. Pediatr Radiol. 2009; 39:668–676. PMID:
19319514.

25. Goo HW, Yang DH. Coronary artery visibility in free-breathing young children with congenital heart disease on cardiac 64-slice CT: dual-source ECG-triggered sequential scan vs. single-source non-ECG-synchronized spiral scan. Pediatr Radiol. 2010; 40:1670–1680. PMID:
20464385.

26. Takemura A, Suzuki A, Inaba R, Sonobe T, Tsuchiya K, Omuro M, et al. Utility of coronary MR angiography in children with Kawasaki disease. AJR Am J Roentgenol. 2007; 188:W534–W539. PMID:
17515343.

27. Tangcharoen T, Bell A, Hegde S, Hussain T, Beerbaum P, Schaeffter T, et al. Detection of coronary artery anomalies in infants and young children with congenital heart disease by using MR imaging. Radiology. 2011; 259:240–247. PMID:
21325034.

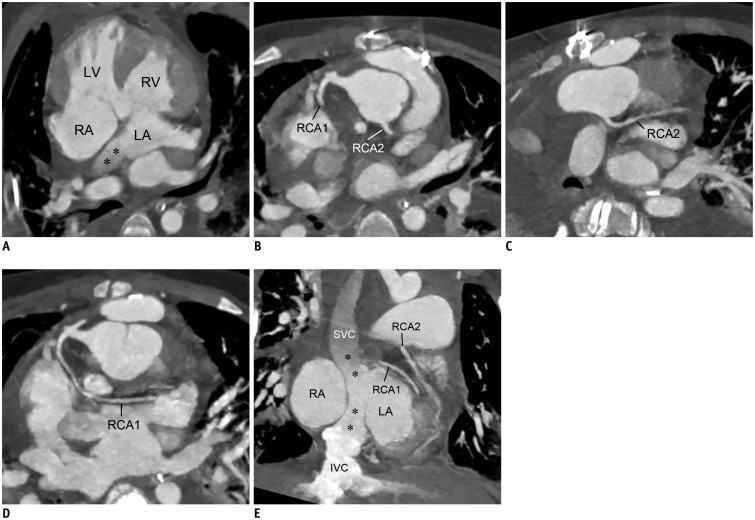
28. Goo HW, Seo DM, Yun TJ, Park JJ, Park IS, Ko JK, et al. Coronary artery anomalies and clinically important anatomy in patients with congenital heart disease: multislice CT findings. Pediatr Radiol. 2009; 39:265–273. PMID:
19159923.

29. Shriki JE, Shinbane JS, Rashid MA, Hindoyan A, Withey JG, DeFrance A, et al. Identifying, characterizing, and classifying congenital anomalies of the coronary arteries. Radiographics. 2012; 32:453–468. PMID:
22411942.

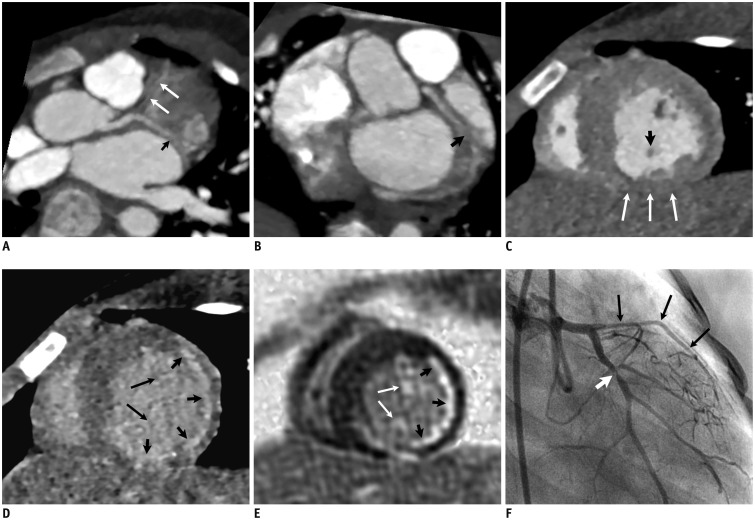
30. Peña E, Nguyen ET, Merchant N, Dennie G. ALCAPA syndrome: not just a pediatric disease. Radiographics. 2009; 29:553–565. PMID:
19325065.

31. Miller JA, Anavekar NS, El Yaman MM, Burkhart HM, Miller AJ, Julsrud PR. Computed tomographic angiography identification of intramural segments in anomalous coronary arteries with interarterial course. Int J Cardiovasc Imaging. 2012; 28:1525–1532. PMID:
21892610.

32. Zenooz NA, Habibi R, Mammen L, Finn JP, Gilkeson RC. Coronary artery fistulas: CT findings. Radiographics. 2009; 29:781–789. PMID:
19448115.

33. Hu X, Wu L, Liu F, Shen Q, Pa M, Huang G. Coronary artery fistulas in children. Evaluation with 64-slice multidetector CT. Herz. 2013; 38:729–735. PMID:
23558553.
34. Marini D, Agnoletti G, Brunelle F, Bonnet D, Ou P. Left coronary to right ventricle fistula in a child: management strategy based on cardiac-gated 64-slice CT. Pediatr Radiol. 2008; 38:325–327. PMID:
17985125.

35. Séguéla PE, Houyel L, Loget P, Piot JD, Paul JF. Critical stenosis of a right ventricle to coronary artery fistula seen at dual-source CT in a newborn with pulmonary atresia and intact ventricular septum. Pediatr Radiol. 2011; 41:1069–1072. PMID:
21487673.

36. Tsai WL, Wei HJ, Tsai IC. High-take-off coronary artery: a haemodynamically minor, but surgically important coronary anomaly. Pediatr Radiol. 2010; 40:232–233. PMID:
19924411.

37. Goo HW, Park IS, Ko JK, Kim YH, Seo DM, Yun TJ, et al. CT of congenital heart disease: normal anatomy and typical pathologic conditions. Radiographics. 2003; 23 Spec No:S147–S165. PMID:
14557509.

38. Goo HW, Park IS, Ko JK, Kim YH, Seo DM, Park JJ. Computed tomography for the diagnosis of congenital heart disease in pediatric and adult patients. Int J Cardiovasc Imaging. 2005; 21:347–365. discussion 367. PMID:
16015453.

39. Nie P, Wang X, Cheng Z, Ji X, Duan Y, Chen J. Accuracy, image quality and radiation dose comparison of high-pitch spiral and sequential acquisition on 128-slice dual-source CT angiography in children with congenital heart disease. Eur Radiol. 2012; 22:2057–2066. PMID:
22592808.

40. Beerbaum P, Sarikouch S, Laser KT, Greil G, Burchert W, Körperich H. Coronary anomalies assessed by whole-heart isotropic 3D magnetic resonance imaging for cardiac morphology in congenital heart disease. J Magn Reson Imaging. 2009; 29:320–327. PMID:
19161183.

41. Yu FF, Lu B, Gao Y, Hou ZH, Schoepf UJ, Spearman JV, et al. Congenital anomalies of coronary arteries in complex congenital heart disease: diagnosis and analysis with dual-source CT. J Cardiovasc Comput Tomogr. 2013; 7:383–390. PMID:
24331934.

42. Sengupta PP, Saxena A, Rajani M. Left main coronary artery compression by aneurysmal pulmonary artery in a patient with tetralogy of Fallot with absent pulmonary valve. Catheter Cardiovasc Interv. 1999; 46:438–440. PMID:
10216010.

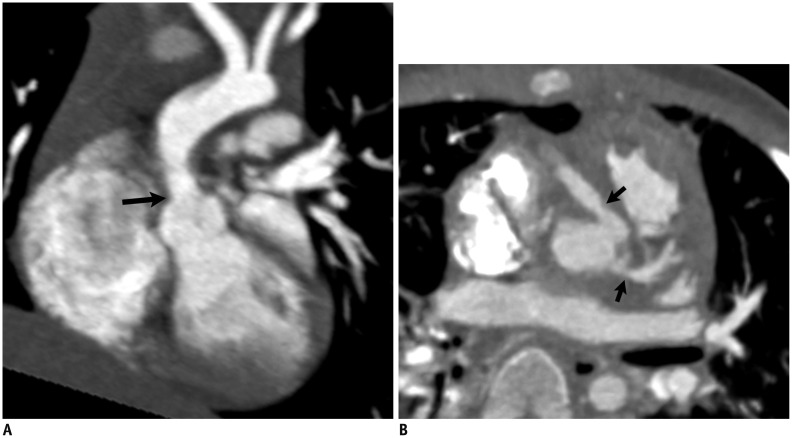
43. Kajita LJ, Martinez EE, Ambrose JA, Lemos PA, Esteves A, Nogueira da, et al. Extrinsic compression of the left main coronary artery by a dilated pulmonary artery: clinical, angiographic, and hemodynamic determinants. Catheter Cardiovasc Interv. 2001; 52:49–54. PMID:
11146522.

44. Safi M, Eslami V, Shabestari AA, Saadat H, Namazi MH, Vakili H, et al. Extrinsic compression of left main coronary artery by the pulmonary trunk secondary to pulmonary hypertension documented using 64-slice multidetector computed tomography coronary angiography. Clin Cardiol. 2009; 32:426–428. PMID:
19685513.

45. Ou P, Celermajer DS, Marini D, Agnoletti G, Vouhé P, Brunelle F, et al. Safety and accuracy of 64-slice computed tomography coronary angiography in children after the arterial switch operation for transposition of the great arteries. JACC Cardiovasc Imaging. 2008; 1:331–339. PMID:
19356445.

46. Marini D, Agnoletti G, Brunelle F, Sidi D, Bonnet D, Ou P. Cardiac CT angiography after coronary artery surgery in children using 64-slice CT scan. Eur J Radiol. 2009; 71:492–497. PMID:
18620830.

47. Ou P, Kutty S, Khraiche D, Sidi D, Bonnet D. Acquired coronary disease in children: the role of multimodality imaging. Pediatr Radiol. 2013; 43:444–453. PMID:
22972555.

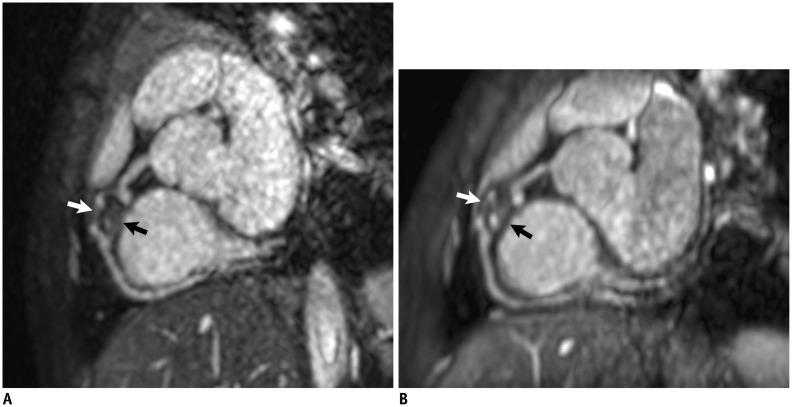
48. Goo HW, Park IS, Ko JK, Kim YH. Coronary CT angiography and MR angiography of Kawasaki disease. Pediatr Radiol. 2006; 36:697–705. PMID:
16770673.

49. Arnold R, Ley S, Ley-Zaporozhan J, Eichhorn J, Schenk JP, Ulmer H, et al. Visualization of coronary arteries in patients after childhood Kawasaki syndrome: value of multidetector CT and MR imaging in comparison to conventional coronary catheterization. Pediatr Radiol. 2007; 37:998–1006. PMID:
17768616.

50. Peng Y, Zeng J, Du Z, Sun G, Guo H. Usefulness of 64-slice MDCT for follow-up of young children with coronary artery aneurysm due to Kawasaki disease: initial experience. Eur J Radiol. 2009; 69:500–509. PMID:
18164157.

51. Carbone I, Cannata D, Algeri E, Galea N, Napoli A, De Zorzi A, et al. Adolescent Kawasaki disease: usefulness of 64-slice CT coronary angiography for follow-up investigation. Pediatr Radiol. 2011; 41:1165–1173. PMID:
21717166.

52. Yu Y, Sun K, Wang R, Li Y, Xue H, Yu L, et al. Comparison study of echocardiography and dual-source CT in diagnosis of coronary artery aneurysm due to Kawasaki disease: coronary artery disease. Echocardiography. 2011; 28:1025–1034. PMID:
21854436.

53. Duan Y, Wang X, Cheng Z, Wu D, Wu L. Application of prospective ECG-triggered dual-source CT coronary angiography for infants and children with coronary artery aneurysms due to Kawasaki disease. Br J Radiol. 2012; 85:e1190–e1197. PMID:
22932064.

54. Gray JC 3rd, Krazinski AW, Schoepf UJ, Meinel FG, Pietris NP, Suranyi P, et al. Cardiovascular manifestations of Williams syndrome: imaging findings. J Cardiovasc Comput Tomogr. 2013; 7:400–407. PMID:
24331936.

55. Ergul Y, Nisli K, Kayserili H, Karaman B, Basaran S, Dursun M, et al. Evaluation of coronary artery abnormalities in Williams syndrome patients using myocardial perfusion scintigraphy and CT angiography. Cardiol J. 2012; 19:301–308. PMID:
22641550.

56. Rohnean A, Houyel L, Sigal-Cinqualbre A, To NT, Elfassy E, Paul JF. Heart transplant patient outcomes: 5-year mean follow-up by coronary computed tomography angiography. Transplantation. 2011; 91:583–588. PMID:
21297555.

57. Mittal TK, Panicker MG, Mitchell AG, Banner NR. Cardiac allograft vasculopathy after heart transplantation: electrocardiographically gated cardiac CT angiography for assessment. Radiology. 2013; 268:374–381. PMID:
23657888.

58. Rackley C, Schultz KR, Goldman FD, Chan KW, Serrano A, Hulse JE, et al. Cardiac manifestations of graft-versus-host disease. Biol Blood Marrow Transplant. 2005; 11:773–780. PMID:
16182178.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download